Urinary Tract Infection in Females, a Clinicopathological Correlation and Appraisal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Head Post Office, Katchery Road, Bahraich-271801 Head Post Office, Veer Vinay Chowk, Balrampur
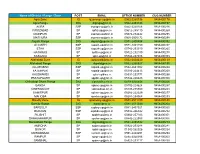
Sr. No. POPSK ADDRESS AMETHI Head post office, Near Bus Station, Amethi-227405 AZAMGARH | 2 Head Post Office, Civil line, Azamgarh-2760001 BAHRAICH Head Post Office, Katchery Road, Bahraich-271801 BALLIA Head Post Office, Harpur Middhi Road, District Court Ballia - 277001 BALRAMPUR Head Post Office, Veer Vinay Chowk, Balrampur- 271201 GONDA Head Post Ofice, Jail Road, Gonda- 271001 MAU Head Post Office, Near Railway Crossing Mau - 275101 PRATAPGARH Head Post Office, Pratapgarh- 230001 8 RAEBAREL Head Post Office, Ghantaghar, Raebareli- 229001 SITAPUR Head Post Office, Sitapur- 261001 10 SULTANPUR Head Post Office, G N Road, Civil Line, Sultanpur-228001 |11 UNNAO Head Post Office, Civil Lines, Near Railway Station, Unnao- 209801 12 JAUNPUR Head Post Office, Alfastinganj, Near Jaunpur Kotwali, Jaunpur- 222001 13 Head Post Office Chunar, Dargah Sharif Station Road, Tammanpatti - 14 CHUNAR 231304 FAIZABAD Head Post Office, Civil Lines Faizabad - 224001 |15 DEORIA Head Post Office Deoria, Sadar Taluk, Deoria 274001 16 Head Post Office Jhansi, In front ofJhansi Hotel, Sadar Bazar, Jhansi JHANSI 17 284001 ALLAHABAD Head Post Office, S.N. Marg Civil Lines, Allahabad 18 Head Post Office Ghazipur, In front of Opium Factory, Mahuwabagh, GHAZIPUR Ghazipur- 233001 19 Head Post office Near Fatehpur Railway Crossing, Behind BSNL FATEHPUR Building, Police Line Fatehpur 212601 20 21 AMBEDKAR NAGAR Head Post Office, SH-5, Moradabad Mohall, Akbarpur,- 224122 22 BANDA BANDA HEAD OFFICE, NEAR BANGALIPURA - 210001 23 HAMIRPUR HAMIRPUR HEAD OFFICE, NEAR BUS STAND-210301 | 24 BHADOHI Bhadohi Mukhya Dakghar, Bhadohi - 221401 25 SIDDHARTHNAGAR HEAD POST OFFICE, TETRI BAZAR, NAUGARH, SIDDHARTHNAGAR, | 272207 (DOMARIYAGANJ) 26 MAHARAJGANJ HEAD POST OFFICE, WARD NO. -

Research Article
Available Online at http://www.recentscientific.com International Journal of CODEN: IJRSFP (USA) Recent Scientific International Journal of Recent Scientific Research Research Vol. 10, Issue, 11(A), pp. 35764-35767, November, 2019 ISSN: 0976-3031 DOI: 10.24327/IJRSR Research Article SOME MEDICINAL PLANTS TO CURE JAUNDICE AND DIABETES DISEASES AMONG THE RURAL COMMUNITIES OF SHRAVASTI DISTRICT (U.P.) , INDIA Singh, N.K1 and Tripathi, R.B2 1Department of Botany, M.L.K.P.G. College Balrampur (U.P.), India 2Department of Zoology, M.L.K.P.G. College Balrampur (U.P.), India DOI: http://dx.doi.org/10.24327/ijrsr.2019.1011.4166 ARTICLE INFO ABSTRACT An ethnobotanical survey was undertaken to collect information from traditional healers on the use Article History: of medicinal plants in rural communities of district Shravasti Uttar Pradesh. The important th Received 4 August, 2019 information on the medicinal plants was obtained from the traditional medicinal people. Present th Received in revised form 25 investigation was carried out for the evaluation on the current status and survey on these medicinal September, 2019 plants. In the study we present 14 species of medicinal plants which are commonly used among the th Accepted 18 October, 2019 rural communities of Shravasti district (U.P.) to cure jaundice and diabetes diseases. This study is th Published online 28 November, 2019 important to preserve the knowledge of medicinal plants used by the rural communities of Shravasti district (U.P.), the survey of the psychopharmacological and literatures of these medicinal plants Key Words: have great pharmacological and ethnomedicinal significance. Medicinal plants, jaundice and diabetes diseases, rural communities of Shravasti. -

Basic Data Report of Kaliandi- Vihar Exploratory Tube
GROUND WATER SCENARIO OF SHRAVASTI DISTRICT, UTTAR PRADESH By S. MARWAHA Superintending. Hydrogeologist CONTENTS Chapter Title Page No. DISTRICT AT A GLANCE ..................3 I. INTRODUCTION ..................5 II. CLIMATE & RAINFALL ..................5 III. GEOMORPHOLOGY & SOILS ..................6 IV. HYDROGEOLOGY ..................7 V. GROUND WATER RESOURCES & ESTIMATION ..................11 VI. GROUND WATER QUALITY ..................13 VII. GROUND WATER DEVELOPMENT ..................16 VIII. GROUND WATER MANAGEMENT STRATEGY ..................17 IX. AWARENESS & TRAINING ACTIVITY ..................18 X. AREAS NOTIFIED BY CGWA/SGWA ..................18 XI. RECOMMENDATIONS ..................18 TABLES : 1. Land Utilisation of Shravasti district (2008-09) 2. Source-wise area under irrigation (Ha), Shravasti, UP 3. Block-wise population covered by hand pumps, Shravasti, UP 4. Depth to water levels - Shravasti district 5. Water Level Trend Of Hydrograph Stations Of Shravasti District, U.P. 6. Block Wise Ground Water Resources As On 31.3.2009, Shravasti 7. Constituent, Desirable Limit, Permissible Limit Number Of Samples Beyond Permissible Limit & Undesirable Effect Beyond Permissible Limit 8. Chemical Analysis Result Of Water Samples, 2011, Shravasti District, U.P 9. Irrigation Water Class & Number of Samples, Shravasti District, U.P 10. Block wise Ground water Extraction structures, 2009, Shravasti, U.P PLATES : (I) Hydrogeological Map Of Shravasti District, U.P. (II) Depth To Water Map (Pre-Monsoon, 2012), Shravasti District, U.P. (III) Depth To Water Map (Post-Monsoon, 2012) , Shravasti District, U.P. (IV) Water Level Fluctuation Map (Pre-Monsoon, 2012—Post-Monsoon,2012), Shravasti District, U.P. (V) Ground Water Resources, as on 31.3.2009, Shravasti District, U.P. 2 DISTRICT AT A GLANCE 1. GENERAL INFORMATION i. Geographical Area (Sq. Km.) : 1858 ii. -

1: Uttar Pradesh Flood A. Situation Report
Situation Report -1: Uttar Pradesh Flood A. Situation Report Due to heavy rainfall in Nepal and Uttarakhand, most of the river including Rapti, Ghaghara, Sharda and Sarayu is overflowing leading to flood situation in the state of Uttara Pradesh. Number of causalities reported 28 Number of people missing 300 Districts affected Bahraich, Shrawasti, Barabanki, Gonda, Siddharth Nagar, Lakhimpuri Kheri, Balrampur, Faizabad, Sitapur Worst affected Districts Bahraich, Shraswasti, Barabanki, Gonda and Siddharth Nagar Number of affected villages 1,500 approx. Official sources in Lucknow said that an alert has been sounded in Bahraich district, which has been the worst affected. The water has entered into hundreds of villages in Mihipurwa, Mahasi, Balha, Kaiserganj and Jarwal development blocks, affecting a population of about 2 lakhs. These sources said that two helicopters are likely to be pressed into service for relief and rehabilitation measures Floods in Uttar Pradesh have raised fears of damage to the cane crop, as 0.6 million hectares of arable lands have been submerged Rising water levels has hit road and rail traffic and Shashtra Seema Bal and PAC jawans have been deployed to evacuate people affected by the floods. In New Delhi, the Ministry of Water Resources said in a statement that the Rapti in Balrampur district of UP was flowing at 104.62m, 0.63m above danger mark. The record for water level in the river was 105.25m on September 11, 2000. According to a Central Water Commission report, after rising menacingly in Kakardhari and Bhinga yesterday, the Rapti has crossed the maximum level in Balrampur and is still rising. -

Lions Clubs International
GN1067D Lions Clubs International Clubs Missing a Current Year Club Only - (President, Secretary or Treasure) District 321B1 District Club Club Name Title (Missing) District 321B1 25971 LUCKNOW CANTONEMENT President District 321B1 25971 LUCKNOW CANTONEMENT Secretary District 321B1 25971 LUCKNOW CANTONEMENT Treasurer District 321B1 26009 PILIBHIT President District 321B1 26009 PILIBHIT Secretary District 321B1 26009 PILIBHIT Treasurer District 321B1 35855 HALDWANI President District 321B1 35855 HALDWANI Secretary District 321B1 35855 HALDWANI Treasurer District 321B1 38749 LUCKNOW METROPOLITAN President District 321B1 38749 LUCKNOW METROPOLITAN Secretary District 321B1 38749 LUCKNOW METROPOLITAN Treasurer District 321B1 41404 BALRAMPUR President District 321B1 41404 BALRAMPUR Secretary District 321B1 41404 BALRAMPUR Treasurer District 321B1 42016 RUDAULI President District 321B1 42016 RUDAULI Secretary District 321B1 42016 RUDAULI Treasurer District 321B1 44483 LAKHIMPUR KHERI UPKAR President District 321B1 44483 LAKHIMPUR KHERI UPKAR Secretary District 321B1 44483 LAKHIMPUR KHERI UPKAR Treasurer District 321B1 46344 SHAHJAHANPUR VISHAL President District 321B1 46344 SHAHJAHANPUR VISHAL Secretary District 321B1 46344 SHAHJAHANPUR VISHAL Treasurer District 321B1 48500 LUCKNOW SEVA President District 321B1 48500 LUCKNOW SEVA Secretary District 321B1 48500 LUCKNOW SEVA Treasurer District 321B1 52057 LUCKNOW SHERIFF President District 321B1 52057 LUCKNOW SHERIFF Secretary District 321B1 52057 LUCKNOW SHERIFF Treasurer District 321B1 54705 LUCKNOW -
District Survey Report
1. INTRODUCTION As per gazette notification dated 15th January 2016, of Ministry of Environment, Forest and Climate Change, the District-Environment Impact Assessment Authority (DEIAA) to be constituted by the divisional commissioner for prior environmental clearance of quarry for minor minerals. The DEIAA will scrutinize and recommend the prior environmental clearance of ministry of minor minerals on the basis of district survey report. The main purpose of preparation of District Survey Report is to identify the mineral resources and mining activities along with other relevant data of district. This DSR contains details of Lease, Sand mining and Revenue which comes from minerals in the district and prepared on the basis of data collected from different concern departments and concern Mining Inspector. DISTRICT-SHRAVASTI Shravasti district is in the north western part of Uttar Pradesh covering an area of 1858.20 Sq. Km. It is a created district carved out from Bahraich district. Shravasti, which is closely associated with the life of Lord Buddha, shares border with Balrampur, Gonda & Bahraich districts. Bhinga is the district headquarters of Shravasti and is approximately 175 kilometers away from the state capital. The district is drained by river Rapti & its tributaries. In 2001 census, Shravasti has three Tehsils, viz., Bhinga, Jamunaha and Ikauna. Shravasti is a historically famous district of eastern Uttar Pradesh. As per 2011 census, total population of the district is 1,114,615 persons out of which 594,318 are males and 520,297 are females. The district has having 3 tehsils, 5 blocks and 536 inhabited villages. According to 2001 census, the district accounted 0.71 % of the State’s population in which male and female percentages are 0.72 and 0.69 respectively. -
Name of District / Range / Zone POST EMAIL OFFICE NUMBER CUG
Name of District / Range / Zone POST EMAIL OFFICE NUMBER CUG NUMBER Agra Zone IG [email protected] 0562-2265736 9454400178 Agra Range DIG [email protected] 0562-2463343 9454400197 AGRA SSP [email protected] 0562-2250106 9454400246 FIROZABAD SP [email protected] 05612-285110 9454400269 MAINPURI SP [email protected] 05672-234442 9454400295 MATHURA SSP [email protected] 0565-2505172 9454400298 Aligarh Range DIG [email protected] 0571-2400404 9454400392 ALIGARH SSP [email protected] 0571-2401150 9454400247 ETAH SSP [email protected] 05742-233319 9454400265 HATHRAS SP [email protected] 05722-232100 9454400278 KASGANJ SP [email protected] 05744-247486 9454400393 Allahabad Zone IG [email protected] 0532-2424630 9454400139 Allahabad Range DIG [email protected] 0532-2260527 9454400195 ALLAHABAD SSP [email protected] 0532-2641902 9454400248 FATEHPUR SP [email protected] 05180-224413 9454400268 KAUSHAMBI SP [email protected] 05331-232771 9454400288 PRATAPGARH SP [email protected] 05342-220423 9454400300 Chitrakoot Dham Range DIG [email protected] 0519-2220538 9454400206 BANDA SP [email protected] 05192-224624 9454400257 CHITRAKOOT SP [email protected] 05198-235500 9454400263 HAMIRPUR SP [email protected] 05282-222329 9454400277 MAHOBA SP [email protected] 05281-254068 9454400293 Bareilly Zone IG [email protected] 0581-2511199 9454400140 Bareilly Range DIG [email protected] 0581-2511049 9454400204 BAREILLY SSP [email protected] 0581-2457021 9454400260 BUDAUN SSP [email protected] 05832-266342 9454400252 PILIBHIT SP [email protected] 05882-257183 9454400301 SHAHJAHANPUR SP [email protected] -

S.N. District Block Village 1 Balrampur Balrampur
List of flood affected near by villages in Balrampur District (U.P.) as on 2nd September 2017 Flood affected blocks=8 Flood affected villages=228 S.N. DISTRICT BLOCK VILLAGE 1 BALRAMPUR BALRAMPUR Ghughulpur 2 Bagahi 3 Chauka Khurd 4 Jambo Deep 5 Lalajot 6 Lilwa 7 Khajuria 8 Bhusailwa 9 Kailash Garh 10 Singhwapur 11 Nand Nagar 12 Gulariha Puraina 13 Gauratirkaulia 14 Kalyanpur 15 Ararpakar 16 Raghavpur 17 Chakawa 18 Samda 19 Singahi 20 Dhondhari 21 Hasuwa Dol 22 Dakahi 23 Belwasultan Jot 24 Dulhapur Ballipur 25 Belha 26 Dhusah 27 Balrampur (MB) 28 Katrasankar Nagar 29 Bhikhampur 30 Sonar 31 Bhagwanpur 32 Ramnagar 33 Rajghat 34 Siria 35 Bafanwa 36 Fattejot 37 Bhagawatpur 38 Seoraha 39 Bharbharia 40 Gondipur 41 Baherekuiyan 42 Mahadeo Misir 43 Kharhargarhi 44 MADHPUR 45 Baghani 46 Deorawan 47 Chulahbhari 48 Nand Nagar 49 Kandbhari 50 Narayanpur Manjhari 51 GAINDAS BUZURG Persauna S.N. DISTRICT BLOCK VILLAGE 52 Majhauatappa Vank 53 Malmalia 54 Chheetar Para 55 Dudhra 56 Maninaha 57 Kaitholia Saleempur 58 Poore Pande Jot 59 Barahaya Bhaisahi 60 Ajagari 61 Kermahia 62 Jigna Ghat 63 Dumaria 64 Bharwalia 65 Chheet Jot 66 Sonhat 67 Nagawa 68 Nandauri 69 Majhari Tappa Wak 70 Puraina Buland 71 Masjidia 72 Kanchanpur 73 Pranpur 74 Vank Bhawanipur 75 Shahpur Tappavank 76 Sahiapur 77 Sisahna 78 Itai Rampur 79 Baudihar 80 Terhawa Tappa Vank 81 Chichoori Sihania 82 Mohd. Pur Banjerha 83 Rasoolabad 84 GESARI Bhaduwa Shanker Nager 85 Jamuni Kalan 86 Motipur 87 Bhadui 88 Ganwariya 89 Gaura 90 Janki Nagar 91 Barhay Purwa 92 Bijuliya 93 Tegnahwa 94 Pakri Patoha 95 Pakri 96 Majhauwa 97 Jaitapur 98 Govindpur 99 Beerpur 100 Misrauliya 101 Kolhiya Bhozpur 102 Mahri 103 Kather 104 HARAIYA SATGHARWA Lalia 105 Pranpur S.N. -

Uttar Pradesh
11.28 UTTAR PRADESH 11.28.1 Introduction Situated in the northern part of the country, Uttar Pradesh covers an area of 2,40,928 sq km, which is 7.33% of the geographical area of the country. The State lies between 23°52'N to 31°28'N latitude and 77°30'E to 84°39' E longitude and is bordered by Uttarakhand in the north, Haryana, Delhi & Rajasthan in the west, Madhya Pradesh in the west and south west, Chhattisgarh in the south and Bihar in the East. It has international border with Nepal in the north. The State has three distinct regions namely, the Shiwalik region in the north, Gangetic plains in the central region and Vindhyan hills in the south. Uttar Pradesh has a humid subtropical climate with dry winters. The annual rainfall ranges between 1,000 mm to 1,200 mm and the annual temperature varies from 5°C to 46°C. The State is drained by a number of rivers, which include Ganga, Yamuna, Gomti, Ghagra, Betwa, Chambal and Gandak. There are 71 districts in the State, of which one is a tribal district and there are no hill districts. As per census 2011, Uttar Pradesh has a population of 199.81 million, which is 16.50% of India population. The urban and rural population constitute 22.27% and 77.73% respectively. The Tribal population is 0.57%. The average population density of the State is 829 per sq km, which is more than twice the national average. The 19th Livestock Census of 2012 has reported a total livestock population of 68.71 million. -

Dynamics of Socio-Economic Development of Districts of Eastern Uttar Pradesh
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Journal of Applied and Natural Science AL SC R IEN TU C A E N F D O N U A N D D Journal of Applied and Natural Science 8 (1): 5 - 9 (2016) A E I T L I O P JANS N P A ANSF 2008 Dynamics of socio-economic development of districts of eastern Uttar Pradesh Nitin Tanwar1*, Sunil Kumar1, B.V.S. Sisodia1, B.K. Hooda2 1Department of Agricultural Statistics, Narendra Deva University of Agriculture and Technology, Kumarganj, Faizabad, U.P., INDIA 2Department of Mathematics, Statistics & Physics, Chaudhary Charan Singh Haryana Agricultural University, Hisar, Haryana, INDIA *Corresponding author. E-mail: [email protected] Received: March 11, 2015; Revised received: August 17, 2015; Accepted: January 1, 2016 Abstract: Development process of any system is dynamic in nature and depends on large number of parameters. This study attempted to capture latest dynamics of development of districts of Eastern Uttar Pradesh in respect of three dimensions- Agriculture, Social and Infrastructure. Techniques adopted by Narain et al. (1991) have been used in addition to Principal component and factor analysis. Ranking seems to very close to ground reality and pro- vides useful information for further planning and corrective measures for future development of Eastern Uttar Pradesh’s Districts. The Composite Indices (C.I.) of development in respect of 18 developmental indicators for the total 28 districts of eastern Uttar Pradesh have been estimated for the year 2010-2011. The district Barabanki was showed a higher level of development (C.I. -

Devipatan Zone CSC List
Grampanchayat District Block Name Village/CSC name Pincode Location VLE Name Contact No Village Name Bahraich Bahraich1 Hathiya Bojhi 271881 hathiya bojhi Farooq Ansari 7054482275 Bahraich Behriach Chittaura(R) 271801 Samsa tarhar Adarsh Kumar Gautam Samsa tarhar 7054693883 Bahraich Bahraich Nanpara 271865 chaugodwa nawabganj Arman Ahmad Chaugorwa 7081092832 Bahraich Bahraich Mahasi 271801 Saraswati nagar India Itech_Lait Kumar bajpaiMahasi 7275011100 Bahraich Vishveshwarganj Bhagirathpurwa Nethiya 271821 Bhagirathpurwa Nethiya VASUDEV PRASAD CHAUHAN 7275248043 Bahraich Nawabganj Umariya 271881 Umriya (Nandagaon) Shrawan Kumar Verma 7376126247 Bahraich Bahraich-NIELIT MIHINPURWA 271855 GANGAPUR AKHILESH PRATAP SINGH GANGAPUR 7376145900 Bahraich Behriach Balha(R) 271865 Sugar Factory, Nanpara Deepak Kumar Siletanganj 7376640895 Bahraich Jarwal Naraunda 271872 Naraunda Deepak kumar pal 7379293493 Bahraich Mihinpurwa Bojhiya 271855 Bojhiya Bazar OM PRAKASH 7379566421 Bahraich Behriach Mihipurwa(R) 271855 Madhwapur Om Prakash Madhwapur 7379568921 Bahraich Behriach1 Mihipurwa(R) 271855 Rampurwa Satish Kumar Rampurwa 7379892297 Bahraich Bahraich-NIELIT Bahraich 271801 Banhraich Asiya Begum Bahraich 7388238777 Bahraich Bahraich-NIELIT KAISERGANJ 271903 KAISERGANJ SATISH KUMAR SRIVASTAVADIHVASHER BAHADUR SINGH7398192862 Bahraich Bahraich Etawah 271865 Nanpara Azhar Ali SARAIYAN 7398196031 Bahraich Behriach Bahraich(U) 271801 Bahraich(U) Jaleel Ahmed Dargah Shareef 7398203894 Bahraich Huzoorpur Shivnaha 271872 Shivnaha Ritu srivastava Dewanpur -

Faizabad Zone CSC List
S Grampanchayat N District Block Name Village/CSC name Pincode Location VLE Name Contact No Village Name o Ambedkar Nagar Bhiti Naghara 224141 Naghara Gunjan Pandey Balal Paikauli 979214477 Ambedkar Nagar Ambedkar Nagar1 Tanda(U) 224145 GANDHI NAGAR SHAHNAZ BANO GANDHI NAGAR 7080871152 Ambedkar Nagar Ambedkar Nagar chakmakhdoompur 224190 chakmakhdoompur Arun Kumar rasoolpur 7275195680 Ambedkar Nagar Ambedkar Nagar Ambedkar Nagar 224190 Ambedkar Nagar Pawan Kumar Maurya Ambedkar Nagar 7275195680 Ambedkar Nagar Ambedkar Nagar1 Pilkhava 224151 gram pilakhawan Amrendra Kumar PILKHAWA 7275455211 Ambedkar Nagar Jalalpur Haidrabad Chauraha 224149 Haidrabad Chauraha Rajesh kumar Prajapati 7309277441 Ambedkar Nagar Ambedkar Nagar Fattepur Khas 224147 Allapur Arvind Chauhan FATTEPUR KHAS 7309368860 Ambedkar Nagar Ambedkar Nagar1 Bhiti(R) 224141 Jaitpur nidhiyawan KULDEEP KR. VERMA Jaitpur nidhiyawan 7376777146 Ambedkar Nagar Ambedkar Nagar SUJAWALPUR 224147 SUJAWALPUR SANGEETA OJHA vishunpur bajdaha 7376878549 Ambedkar Nagar AMBEDKAR NAGAR-NIELITAmbedkar Nagar 224146 Ambedkar Nagar FIA_Sandhya Verma Ambedkar Nagar 7376878965 Ambedkar Nagar Ambedkar Nagar Tanda 224190 FAREEDPUR KALA Awanish Bharati Faridpur Kala 7398215521 Ambedkar Nagar Ambedkar Nagar Tanda 224155 Purabajgoti Nasrullahpur Mohd Hamid Purabajgoti 7398310929 Ambedkar Nagar Ambedkar Nagar Akbarpur(R) 224190 Pakari bhojpur R V STAYA PRAKASH V MAURYAPakari bhojpur 7408100615 Ambedkar Nagar Ambedkar Nagar Ambedkar Nagar 224129 dashraicha Pankaj Yadav dashraicha 7458817825 Ambedkar Nagar