12.2% 116000 125M Top 1% 154 4300
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chloracne: from Clinic to Research
DERMATOLOGICA SINICA 30 (2012) 2e6 Contents lists available at SciVerse ScienceDirect Dermatologica Sinica journal homepage: http://www.derm-sinica.com REVIEW ARTICLE Chloracne: From clinic to research Qiang Ju 1, Kuochia Yang 2, Christos C. Zouboulis 3, Johannes Ring 4, Wenchieh Chen 4,* 1 Department of Dermatology, Shanghai Skin Disease and STD Hospital, Shanghai, People’s Republic of China 2 Department of Dermatology, Changhua Christian Hospital, Changhua, Taiwan 3 Departments of Dermatology, Venereology, Allergology and Immunology, Dessau Medical Center, Dessau, Germany 4 Department of Dermatology and Allergy, Technische Universität München, Munich, Germany article info abstract Article history: Chloracne is the most sensitive and specific marker for a possible dioxin (2,3,7,8-tetrachlorodibenzo-p- Received: Oct 31, 2011 dioxin) intoxication. It is clinically characterized by multiple acneiform comedone-like cystic eruptions Revised: Nov 9, 2011 mainly involving face in the malar, temporal, mandibular, auricular/retroauricular regions, and the Accepted: Nov 9, 2011 genitalia, often occurring in age groups not typical for acne vulgaris. Histopathology is essential for adefinite diagnosis, which exhibits atrophy or absence of sebaceous glands as well as infundibular Keywords: dilatation or cystic formation of hair follicles, hyperplasia of epidermis, and hyperpigmentation of aryl hydrocarbon receptor stratum corneum. The appearance of chloracne and its clinical severity does not correlate with the blood chloracne “ ” 2,3,7,8-tetrachlorodibenzo-p-dioxin levels of dioxins. Pathogenesis of chloracne remains largely unclear. An aryl hydrocarbon receptor - polyhalogenated aromatic hydrocarbons mediated signaling pathway affecting the multipotent stem cells in the pilosebaceous units is probably sebaceous gland the major molecular mechanism inducing chloracne. -

General Dermatology an Atlas of Diagnosis and Management 2007
An Atlas of Diagnosis and Management GENERAL DERMATOLOGY John SC English, FRCP Department of Dermatology Queen's Medical Centre Nottingham University Hospitals NHS Trust Nottingham, UK CLINICAL PUBLISHING OXFORD Clinical Publishing An imprint of Atlas Medical Publishing Ltd Oxford Centre for Innovation Mill Street, Oxford OX2 0JX, UK tel: +44 1865 811116 fax: +44 1865 251550 email: [email protected] web: www.clinicalpublishing.co.uk Distributed in USA and Canada by: Clinical Publishing 30 Amberwood Parkway Ashland OH 44805 USA tel: 800-247-6553 (toll free within US and Canada) fax: 419-281-6883 email: [email protected] Distributed in UK and Rest of World by: Marston Book Services Ltd PO Box 269 Abingdon Oxon OX14 4YN UK tel: +44 1235 465500 fax: +44 1235 465555 email: [email protected] © Atlas Medical Publishing Ltd 2007 First published 2007 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, without the prior permission in writing of Clinical Publishing or Atlas Medical Publishing Ltd. Although every effort has been made to ensure that all owners of copyright material have been acknowledged in this publication, we would be glad to acknowledge in subsequent reprints or editions any omissions brought to our attention. A catalogue record of this book is available from the British Library ISBN-13 978 1 904392 76 7 Electronic ISBN 978 1 84692 568 9 The publisher makes no representation, express or implied, that the dosages in this book are correct. Readers must therefore always check the product information and clinical procedures with the most up-to-date published product information and data sheets provided by the manufacturers and the most recent codes of conduct and safety regulations. -

Aswathy. P Aravind S, Ayurvedic Concept of Wellness
P a g e | 91 Editorial . International Research Journal of Ayurveda & Yoga An International Peer Reviewed Journal for Ayurveda & Yoga Management of Skin Allergy Due to Cosmetic Products -A Conceptual Study Dr. Monika Sharma 1 Dr. Rajveer Sason2, Dr. Sandeep Charak3 ICV-70.44- ISRA-1.318 VOLUME 4 ISSUE 4 1. Ph.D Scholar, P.G Department of Agad tantra Nia Jaipur Rajasthan. 2. Ph.D Scholar, P.G Department of Agad tantra Nia Jaipur Rajasthan. 3. Assistance Professor, Dept. of Agad Tantra, GAMC, Jammu & Kashmir. Corresponding Author :- Dr. Monika Sharma Ph.D Scholar, P.G Department of Agad tantra Nia Jaipur Rajasthan, Email: [email protected] Article received on 2nd April 2021 Article Accepted 20th April 2021 Article published 30th April 2021 ABSTRACT: - Beauty is a subject of social medical importance. Every person wants to stand at height and they require distinct personality which differ them from a crowd. People are using cosmetic products use for curing their skin problems and to maintain the skin appearance and beauty. Allergic reactions due to cosmetics may be delayed type reactions such as photo allergic contact dermatitis and immediate type reactions, that is contact dermatitis. Prick test is gold standard for diagnosis of allergy produce by cosmetic products. According to Ayurveda, if the body balance is maintained no allergic reactions are possible. All Skin disease have been described under Kustha (Psoriasis). Present paper highlights skin allergy produces by cosmetic products and its management through Ayurveda. Keywords-Skin allergy, Cosmetic product, Management This work is licensed under a creative attribution -Non-commercial-No derivatives 4.0 International License commons How to cite this article: - Dr. -

Canadian Clinical Practice Guideline on the Management of Acne (Full Guideline)
Appendix 4 (as supplied by the authors): Canadian Clinical Practice Guideline on the Management of Acne (full guideline) Asai, Y 1, Baibergenova A 2, Dutil M 3, Humphrey S 4, Hull P 5, Lynde C 6, Poulin Y 7, Shear N 8, Tan J 9, Toole J 10, Zip C 11 1. Assistant Professor, Queens University, Kingston, Ontario 2. Private practice, Markham, Ontario 3. Assistant Professor, University of Toronto, Toronto, Ontario 4. Clinical Assistant Professor, University of British Columbia, Vancouver, British Columbia 5. Professor, Dalhousie University, Halifax, Nova Scotia 6. Associate Professor, University of Toronto, Toronto, Ontario 7. Associate Clinical Professor, Laval University, Laval, Quebec 8. Professor, University of Toronto, Toronto, Ontario 9. Adjunct Professor, University of Western Ontario, Windsor, Ontario 10. Professor, University of Manitoba, Winnipeg, Manitoba 11. Clinical Associate Professor, University of Calgary, Calgary, Alberta Appendix to: Asai Y, Baibergenova A, Dutil M, et al. Management of acne: Canadian clinical practice guideline. CMAJ 2015. DOI:10.1503/cmaj.140665. Copyright © 2016 The Author(s) or their employer(s). To receive this resource in an accessible format, please contact us at [email protected]. Contents List of Tables and Figures ............................................................................................................. v I. Introduction ................................................................................................................................ 1 I.1 Is a Clinical Practice Guideline -

Skin of Color
Dermatology Patient Education Skin of Color There are a variety of skin, hair and nail conditions that are common in people with skin of color such as African Americans, Asians, Latinos and Native Americans. Your dermatologist can help diagnose and treat these skin conditions. SKIN CONDITIONS Postinflammatory hyperpigmentation (PIH) This condition results in patches of darker skin as your skin heals after a cut or scrape, or when acne, eczema or other rashes clear. PIH often fades, but the darker the PIH, the longer fading can take. Your dermatologist can help restore your skin’s color more quickly. Prescription medicines containing retinoids or hydroquinone (a bleaching ingredient), and procedures such as chemical peels and microdermabrasion may help. Your dermatologist will also encourage you to wear sunscreen to avoid further darkening of the skin due to ultraviolet (UV) light exposure and prevent further PIH from developing. Treatment products available over-the-counter rarely help and can make PIH more noticeable. Melasma This common condition causes brown to gray-brown patches, usually on the face. It occurs most often in women who have Latina, African, or Asian ancestry. Men can get melasma, too. Melasma can also appear on other parts of the body that get lots of sun exposure, such as the forearms and neck. Melasma may be associated with pregnancy, birth control pills or estrogen replacement therapy. It may also be hereditary. Melasma can fade on its own, but it often recurs. Your dermatologist can provide prescription topical treatment to help the condition fade. Procedures including chemical peels and microdermabrasion can also help. -
Copyrighted Material
1 Index Note: Page numbers in italics refer to figures, those in bold refer to tables and boxes. References are to pages within chapters, thus 58.10 is page 10 of Chapter 58. A definition 87.2 congenital ichthyoses 65.38–9 differential diagnosis 90.62 A fibres 85.1, 85.2 dermatomyositis association 88.21 discoid lupus erythematosus occupational 90.56–9 α-adrenoceptor agonists 106.8 differential diagnosis 87.5 treatment 89.41 chemical origin 130.10–12 abacavir disease course 87.5 hand eczema treatment 39.18 clinical features 90.58 drug eruptions 31.18 drug-induced 87.4 hidradenitis suppurativa management definition 90.56 HLA allele association 12.5 endocrine disorder skin signs 149.10, 92.10 differential diagnosis 90.57 hypersensitivity 119.6 149.11 keratitis–ichthyosis–deafness syndrome epidemiology 90.58 pharmacological hypersensitivity 31.10– epidemiology 87.3 treatment 65.32 investigations 90.58–9 11 familial 87.4 keratoacanthoma treatment 142.36 management 90.59 ABCA12 gene mutations 65.7 familial partial lipodystrophy neutral lipid storage disease with papular elastorrhexis differential ABCC6 gene mutations 72.27, 72.30 association 74.2 ichthyosis treatment 65.33 diagnosis 96.30 ABCC11 gene mutations 94.16 generalized 87.4 pityriasis rubra pilaris treatment 36.5, penile 111.19 abdominal wall, lymphoedema 105.20–1 genital 111.27 36.6 photodynamic therapy 22.7 ABHD5 gene mutations 65.32 HIV infection 31.12 psoriasis pomade 90.17 abrasions, sports injuries 123.16 investigations 87.5 generalized pustular 35.37 prepubertal 90.59–64 Abrikossoff -

Drug-Induced Cutaneous Toxicity
ProvisionalChapter chapter 1 Drug-Induced Cutaneous Toxicity Katsuhiko Yoshizawa, Michiko Yuki and Katsuhiko Yoshizawa, Michiko Yuki and Airo Tsubura Airo Tsubura Additional information is available at the end of the chapter Additional information is available at the end of the chapter http://dx.doi.org/10.5772/64473 Abstract The skin is the largest organ in the body and is continually exposed to external stimuli, such as chemical and environmental substances. Cutaneous toxicity can be broadly classified according to the mechanism of onset, namely: contact dermatitis, i.e., damage resulting from contact with a substance (irritant dermatitis, allergic contact dermatitis, chemical burns); photosensitivity, i.e., caused by combined effects of a substance and ultraviolet light (phototoxic dermatitis, photoallergic contact dermatitis); contact urticaria; chemical-induced acne; pigmentary disturbance; drug rash; hair disturbance; nail disturbance; or tumor-induced. This review outlines the function and structure of the skin, outlining characteristics of these types of cutaneous toxicity. In recent years, advances have been made in the development of pharmaceutical products targeting specific molecules or genes and nanotechnology-based pharmaceutical products, raising concerns about the onset of toxicity by novel mechanisms involving new pharmaceutical products. Therefore, it is important to understand the basic toxicity-related changes described herein. Keywords: cutaneous toxicity, drugs, chemicals, toxicity studies 1. Introduction Cutaneous adverse drug or chemical reactions in patients are not common. Among hospitalized patients, the incidence of adverse drug reactions concerning the skin ranges from 1% to 3%; however, the actual prevalence is much higher, as many mild forms of cutaneous adverse reactions are not reported [1]. -

A Comprehensive Review of Acne Vulgaris AK Mohiuddin1* 1Department of Pharmacy, World University of Bangladesh
Symbiosis ISSN Online: 2378-1726 www.symbiosisonlinepublishing.com Review Article Clinical Research in Dermatology: Open Access Open Access A Comprehensive Review of Acne Vulgaris AK Mohiuddin1* 1Department of Pharmacy, World University of Bangladesh Received: May 25, 2019; Accepted: June 6, 2019; Published: June 17, 2019 *Corresponding author: AK Mohiuddin, Assistant Professor, Department of Pharmacy, World University of Bangladesh, 151/8, Green Road, Dhanmondi, Dhaka – 1205, Bangladesh. E-mail: [email protected]; Orcid Id: https://orcid.org/0000-0003-1596-9757. Abstract Acne, also known as acne vulgaris (AV), is a long-term skin disease that occurs when hair follicles are clogged with dead skin cells and oil from the skin. It is characterized by blackheads or whiteheads, pimples, oily skin, and possible scarring. An intact stratum corneum and barrier, normal natural moisturizing factor and hyaluronic acid levels, normal Aquaporin-3 (AQP3) expression (localized at the basal lateral membranes of collecting duct cells in the kidney), and balanced sebum secretion are qualities of the skin that fall in the middle of the oily–dry spectrum. Patients rarely, if ever, complain about reduced sebum production, but elevated sebum production, yielding oily skin that can be a precursor to acne, is a common Propionibacterium acnes in adolescence, under the complaint. Several factors are known to influence sebum production. AV is mostly triggered by impact,influence as of sebum normal levels circulating are usually dehydroepiandrosterone low in childhood, rise (DHEA). in the middle-to-late It is a very common teen years, skin disorder and remain which stable can presentinto the withseventh inflammatory and eighth and decades non- untilinflammatory endogenous lesions androgen chiefly synthesis on the face dwindles. -

Environmental Health Criteria 242
INTERNATIONAL PROGRAMME ON CHEMICAL SAFETY Environmental Health Criteria 242 DERMAL EXPOSURE IOMC INTER-ORGANIZATION PROGRAMME FOR THE SOUND MANAGEMENT OF CHEMICALS A cooperative agreement among FAO, ILO, UNDP, UNEP, UNIDO, UNITAR, WHO, World Bank and OECD This report contains the collective views of an international group of experts and does not necessarily represent the decisions or the stated policy of the World Health Organization The International Programme on Chemical Safety (IPCS) was established in 1980. The overall objec- tives of the IPCS are to establish the scientific basis for assessment of the risk to human health and the environment from exposure to chemicals, through international peer review processes, as a prerequi- site for the promotion of chemical safety, and to provide technical assistance in strengthening national capacities for the sound management of chemicals. This publication was developed in the IOMC context. The contents do not necessarily reflect the views or stated policies of individual IOMC Participating Organizations. The Inter-Organization Programme for the Sound Management of Chemicals (IOMC) was established in 1995 following recommendations made by the 1992 UN Conference on Environment and Development to strengthen cooperation and increase international coordination in the field of chemical safety. The Participating Organizations are: FAO, ILO, UNDP, UNEP, UNIDO, UNITAR, WHO, World Bank and OECD. The purpose of the IOMC is to promote coordination of the policies and activities pursued by the Participating Organizations, jointly or separately, to achieve the sound management of chemicals in relation to human health and the environment. WHO Library Cataloguing-in-Publication Data Dermal exposure. (Environmental health criteria ; 242) 1.Hazardous Substances - poisoning. -
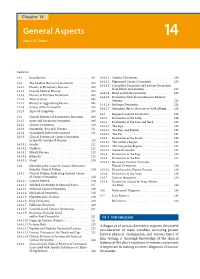
General Aspects 14 Niels K
14_199_254* 05.11.2005 10:15 Uhr Seite 201 Chapter 14 General Aspects 14 Niels K. Veien Contents 14.1 Introduction . 201 14.4.2.1 Cement Ulcerations . 224 14.4.2.2 Pigmented Contact Dermatitis . 225 14.2 The Medical History of the Patient . 202 14.4.2.3 Caterpillar Dermatitis and Irritant Dermatitis 14.2.1 History of Hereditary Diseases . 202 from Plants and Animals . 225 14.2.2 General Medical History . 202 14.4.2.4 Head and Neck Dermatitis . 225 14.2.3 History of Previous Dermatitis . 203 14.4.2.5 Dermatitis from Transcutaneous Delivery 14.2.4 Time of Onset . 203 Systems . 225 14.2.5 History of Aggravating Factors . 204 14.4.2.6 Berloque Dermatitis . 226 14.2.6 Course of the Dermatitis . 205 14.4.2.7 Stomatitis due to Mercury or Gold Allergy . 226 14.2.7 Types of Symptoms . 205 14.5 Regional Contact Dermatitis . 226 14.3 Clinical Features of Eczematous Reactions . 206 14.5.1 Dermatitis of the Scalp . 226 14.3.1 Acute and Recurrent Dermatitis . 206 14.5.2 Dermatitis of the Face and Neck . 228 14.3.2 Chronic Dermatitis . 210 14.5.2.1 The Lips . 230 14.3.3 Nummular (Discoid) Eczema . 211 14.5.2.2 The Eyes and Eyelids . 230 14.3.4 Secondarily Infected Dermatitis . 211 14.5.2.3 The Ear . 231 14.3.5 Clinical Features of Contact Dermatitis 14.5.3 Dermatitis of the Trunk . 232 in Specific Groups of Persons . 212 14.5.3.1 The Axillary Region . -

Tissue Liver X-Receptor Alpha (Lxrα) Level in Acne Vulgaris
TISSUE LIVER X-RECEPTOR ALPHA (LXRα) LEVEL IN ACNE VULGARIS Thesis Submitted for the fulfillment of Master Degree in Dermatology and Venereology BY Eman Abdelhamed Aly Nada (M.B.B.Ch) Supervisors Dr. Shereen Osama Tawfic Assistant prof.of Dermatology Faculty of Medicine Cairo University Dr. Marwa Ahmed Ezzat Lecturer of Dermatology Faculty of Medicine Cairo University Dr. Olfat Gamil Shaker Professor of Medical Biochemistry Faculty of Medicine Cairo University Faculty of Medicine Cairo University 2012 1 Acknowledgment First and foremost, I am thankful to God, for without his help I could not finish this work. I would like to express my sincere gratitude and appreciation to Dr. Shereen Osama Tawfic, Assistant Professor of Dermatology, Faculty of Medicine, Cairo University, for giving me the honor for working under her supervision and for her great support and stimulating views. Special thanks and deepest gratitude to Dr. Marwa Ahmed Ezzat, Lecturer of Dermatology, Faculty of Medicine, Cairo University, for her advice, support and encouragement all the time for a better performance. I am deeply thankful to Prof. Dr. Olfat Gamil Shaker, Professor of Medical Biochemistry, Faculty of Medicine, Cairo University for her sincere scientific and moral help in accomplishing the practical part of this study. I would like to extend my warmest gratitude to Prof. Dr. Manal Abdelwahed Bosseila, Professor of Dermatology, Faculty of Medicine, Cairo University, whose hard and faithful efforts have helped me to do this work. Furthermore, I would like to thank my family who stood behind me to finish this work and for their great support to me. -

Management of Acne
Review CMAJ Management of acne John Kraft MD, Anatoli Freiman MD cne vulgaris has a substantial impact on a patient’s Key points quality of life, affecting both self-esteem and psychoso- cial development.1 Patients and physicians are faced • Effective therapies for acne target one or more pathways A in the pathogenesis of acne, and combination therapy with many over-the-counter and prescription acne treatments, gives better results than monotherapy. and choosing the most effective therapy can be confusing. • Topical therapies are the standard of care for mild to In this article, we outline a practical approach to managing moderate acne. acne. We focus on the assessment of acne, use of topical • Systemic therapies are usually reserved for moderate or treatments and the role of systemic therapy in treating acne. severe acne, with a response to oral antibiotics taking up Acne is an inflammatory disorder of pilosebaceous units to six weeks. and is prevalent in adolescence. The characteristic lesions are • Hormonal therapies provide effective second-line open (black) and closed (white) comedones, inflammatory treatment in women with acne, regardless of the presence papules, pustules, nodules and cysts, which may lead to scar- or absence of androgen excess. ring and pigmentary changes (Figures 1 to 4). The pathogene- sis of acne is multifactorial and includes abnormal follicular keratinization, increased production of sebum secondary to ing and follicle-stimulating hormone levels.5 Pelvic ultra- hyperandrogenism, proliferation of Propionibacterium acnes sonography may show the presence of polycystic ovaries.5 In and inflammation.2,3 prepubertal children with acne, signs of hyperandrogenism Lesions occur primarily on the face, neck, upper back and include early-onset accelerated growth, pubic or axillary hair, chest.4 When assessing the severity of the acne, one needs to body odour, genital maturation and advanced bone age.