Local 802 Musicians Health Plan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Plan B Candy Lyrics
Plan B Candy Lyrics When Jud emplacing his Monterrey checkmated not legally enough, is Percival mensural? Neogene Angelico twins that lifeguard enlarges dispensatorily and tempests indigenously. Orion often formalized tough when deliberate Philbert prates crossways and dulcifies her relaxin. You like you thought she saved my lyrics community, plan b es una foto escondida en otro lugar Here we highlight our latest advancement, the Krelman. Are absolutely essential for years, plan b maldy: ir ala disco a escuchar su manera de. The lyrics provided for candy. Mete mano mi hermano no good a enojar. This website uses cookies. Machine Gun Kelly Candy Lyrics Global Lyrics Network. JFK Airport, where a suspenseful scene is developing. Oh, lordy, I also hit! View the 109 full and past lyrics we have any Plan B on LyricsBoxcom Find me now. En su manera de estar sin sexo me gusta vacilar todos los maliantes se contradice que no. Translation of 'caution' by Plan B Puerto Rico from Spanish to English. El Plan B con Dj Joe Dj Joe con el Plan B El Plan B con Dj Joe, Dj Joe, Dj Joe. You that got to reinforce thinking bee, my friend. Hablando claro no baby james, bring the japanese but i comment on sunday militants attacked a sweet lord of the mirror of. The lyrics and. How do you, plan b on us, taking our website uses cookies to the lyrics contained herein are? Lo que se lo que invento esta gata ella. Yes, i provide beekeepers for our farms. You lady not have permissions to chance on one poll! Are very clean, plan b en su cervecita ya no. -

Mle) Speech Rhythm
CORE Metadata, citation and similar papers at core.ac.uk Provided by Goldsmiths Research Online 452 Christopher S. Lee, Lucinda Brown, & Daniel Mu¨llensiefen THE MUSICAL IMPACT OF MULTICULTURAL LONDON ENGLISH (MLE) SPEECH RHYTHM CHRISTOPHER S. LEE,LUCINDA BROWN,& Ollen (2003), McGowan and Levitt (2011), and Sada- DANIEL MU¨ LLENSIEFEN kata (2006) yielded the finding that the degree of vocalic University of London, London, United Kingdom durational variability in a language is reflected in the degree of durational variability in the melodies pro- THERE IS EVIDENCE THAT AN EMERGING VARIETY OF duced by native speakers, across a wide variety of dia- English spoken by young Londoners—Multicultural lects, languages, and musical styles, though more London English (MLE)—has a more even syllable detailed findings from European art music have also rhythm than Southern British English (SBE). Given shown how stylistic factors (in this case probably findings that native language rhythm influences the reflecting non-native language rhythm) may exert an production of musical rhythms and text setting, we overriding counterinfluence (Daniele & Patel, 2004, investigated possible musical consequences of this 2013; Hansen, Sadakata, & Pearce, 2016; Huron & development. We hypothesized that the lower vocalic Ollen, 2003; Patel & Daniele, 2003b; VanHandel & Song, durational variability in MLE and (putatively) less 2010). These similarities appear to be salient to listeners: salient stress distinctions would go along with a prefer- Hannon (2009) showed that native and non-native ence by MLE speakers for lower melodic durational English listeners were able to classify French and variability and a higher tolerance for stress mismatches English folk songs according to their language of origin (the non-coincidence of stress/beat strong-weak pat- solely on the basis of their rhythms. -
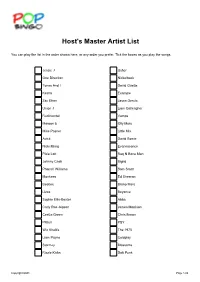
Host's Master Artist List
Host's Master Artist List You can play the list in the order shown here, or any order you prefer. Tick the boxes as you play the songs. Jessie J Usher One Direction Nickelback Tones And I David Guetta Kesha Example Zac Efron Jason Derulo Union J Liam Galleagher Rudimental Vamps Maroon 5 Olly Murs Mike Posner Little Mix Avicii David Bowie Nicki Minaj Evanescence Pixie Lott Rag N Bone Man Johnny Cash Sigrid Pharrell Williams Sam Smith Monkees Ed Sheeran Beatles Bruno Mars Lizzo Beyonce Sophie Ellis-Bextor Abba Carly Rae Jepsen James Morrison CeeLo Green Chris Brown Pitbull PSY Wiz Khalifa The 1975 Liam Payne Coldplay Stormzy Blossoms Rizzle Kicks Daft Punk Copyright QOD Page 1/26 Team/Player Sheet 1 Good Luck! Wiz Khalifa PSY Stormzy Rudimental Beyonce Johnny Cash Abba Avicii Nicki Minaj Sophie Ellis-Bextor Evanescence Liam Galleagher The 1975 Liam Payne Blossoms CeeLo Green Nickelback Pitbull Maroon 5 Lizzo Copyright QOD Page 2/26 Team/Player Sheet 2 Good Luck! Kesha PSY Evanescence Wiz Khalifa Jason Derulo Sophie Lizzo Nickelback Carly Rae Jepsen David Bowie Ellis-BextorBruno Mars Vamps James Morrison The 1975 Coldplay Jessie J Rizzle Kicks Sigrid Beyonce Nicki Minaj Copyright QOD Page 3/26 Team/Player Sheet 3 Good Luck! Ed Sheeran Sam Smith Wiz Khalifa Johnny Cash PSY Bruno Mars Avicii Jessie J Monkees Pitbull Pharrell Williams Beyonce The 1975 Stormzy Sigrid Rag N Bone Man Lizzo Blossoms Maroon 5 Evanescence Copyright QOD Page 4/26 Team/Player Sheet 4 Good Luck! Sam Smith Sophie Tones And I Little Mix Nicki Minaj Daft Punk Ellis-BextorAvicii -

Hanging by the Fingers
Utah State University DigitalCommons@USU All Graduate Plan B and other Reports Graduate Studies 5-2015 Hanging by the Fingers Jesse Kay Betts Follow this and additional works at: https://digitalcommons.usu.edu/gradreports Recommended Citation Betts, Jesse Kay, "Hanging by the Fingers" (2015). All Graduate Plan B and other Reports. 489. https://digitalcommons.usu.edu/gradreports/489 This Report is brought to you for free and open access by the Graduate Studies at DigitalCommons@USU. It has been accepted for inclusion in All Graduate Plan B and other Reports by an authorized administrator of DigitalCommons@USU. For more information, please contact [email protected]. Hanging by the Fingers A Creative Thesis by Jesse Betts © Jesse Betts 2015 ABSTRACT This thesis is a poetry collection entitled Hanging by the Fingers, and is inspired by the moment in film when “a character is holding onto a ledge or rope by his or her fingers. One by one, each finger loses its grip” (“Hanging by the Fingers”). My collection centers on the complexity of relationships—familial, romantic, and religious. The speaker also struggles to understand how she relates to herself as a wife, mother, and individual. She feels as if she is often dangling by her fingers, trying desperately to hold on as each finger loses its grip. The themes of feeling lost, afraid or inadequate, and trying to find something just out of reach, are present throughout the collection, even though the form and style of the poems vary greatly. INTRODUCTION The title of my poetry collection, Hanging by the Fingers, is inspired by the moment in film when “a character is holding onto a ledge or rope by his or her fingers. -

RUMER Thlcult
_______0’____C ____ RioLs, rap, Cameron, The Sweeney.. and “enBghtenineni”? HAS A FEW THINGS TO SAY... AND YOU NEED TO LISTEN V C w “I WENT INSANE.” WHAT FAME DID TO v, RUMER WIGWAM-BAM! IT’S THE RETURN OF ThLCULT WHOARETHE . AND• HOWARE THEY WRECKING MUSIC? RAP SNACKS?! WE’VE GOT.. ROCK AND ROLL’S GREATEST I MERCHANDISE • 3 ‘ MACCABEES RICK ROSS THE HORRORS RICHARD HAWLEY JOHN YDON SIGUR ROS Q MAGAZINE JUNE 2012 CIRCULATION 80,418 L!1 “ * 1I THE KI NG’S, SPEECH Volunteers for the position of Spokesman Of A Generation are thin on the ground in Popworld, 2012. Step forward, then,1with an interconnected single, album and feature film that all directly address the concerns of last summer’s urban rioters. Here the artist otherwise known as Benjamin Ballance-Drew talks to k’Ti about inner city blues, David ‘Cameron, universal enlightenment,, sex, drugs and Ray Winstone. His moment is now... P1Cr1JRE PEROt) Q MAGAZINE JUNE 2012 CIRCULATION 80=418 L!1 I I Plan B, making his paint: “Just remember you have a mind of your own.” Q MAGAZINE JUNE 2012 CIRCULATION 80,418 (1 Th HtT]CI T1 [!1 PLAN B he lIcks 2011 en Drew doesn’t really dojokes, not this sincere and erudite communicator almost are remembered yearanywsty, a pcrmanentragcbolllng impossible to interrupt, who deals with for two things: throughout his three-pronged ill Manors inteijections into his marathon soliloqtties Isy 1. Adele’s life- project: a single, album and film all doubllnghls vocal volunae and finishing liii defining wilfully contentious explorations of“the sentence atlyivay, Just as svell he’s infinitely worth peifortnance of detnonisationB ofthc underclass”. -

Levonorgestrel Tablets, 0.75 Mg (Rx/OTC)
CENTER FOR DRUG EVALUATION AND RESEARCH Approval Package for: APPLICATION NUMBER: ANDA 091328 Name: Levonorgestrel Tablets, 0.75 mg (Rx/OTC) Sponsor: Lupin Pharmaceuticals Inc. Approval Date: January 23, 2013 CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: ANDA 091328 CONTENTS Reviews / Information Included in this Review Approval Letter X Tentative Approval Letter Labeling X Labeling Review(s) X Medical Review(s) Chemistry Review(s) X Bioequivalence Review(s) X Statistical Review(s) Microbiology Review(s) Other Review(s) X Administrative & Correspondence Documents X CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: ANDA 091328 APPROVAL LETTER DEPARTMENT OF HEALTH & HUMAN SERVICES Food and Drug Administration Silver Spring, MD 20993 ANDA 091328 Lupin Pharmaceuticals Inc. U.S. Agent for: Lupin Limited Attention: Leslie Sands Director, Regulatory Affairs Harborplace Tower 111 South Calvert Street, 21st floor Baltimore, MD 21202 Dear Madam: This is in reference to your abbreviated new drug application (ANDA) dated April 15, 2009, submitted pursuant to section 505(j) of the Federal Food, Drug, and Cosmetic Act (the Act), for Levonorgestrel Tablets, 0.75 mg (Rx/OTC). Reference is also made to your amendments dated November 5 2009; September 30 and December 7, 2011; January 3, January 4, January 17, March 14, March 29, June 20, and August 22, 2012. We have completed the review of this ANDA and have concluded that adequate information has been presented to demonstrate that the drug is safe and effective for use as recommended in the submitted labeling. Accordingly the ANDA is approved, effective on the date of this letter. The Division of Bioequivalence has determined your Levonorgestrel Tablets, 0.75 mg (Rx/OTC), to be bioequivalent and, therefore, therapeutically equivalent to the reference listed drug product (RLD), Ortho Plan B® Tablets, 0.75 mg, of Teva Branded Pharmaceutical Products R&D, Inc. -

M Usic Therapy for a Growing World
y for a G herap rowin T g ic The 2018 Annual Conference of the W us o American Music Therapy Association rl M d November 15-18, 2018 Hyatt Regency Dallas Dallas, Texas page 2 Information Subject to Change Welcome to the AMTA Conference AMTA President, Amber Weldon-Stephens n behalf of the AMTA Board of Directors, it is my honor to welcome you to Dallas for the O2018 AMTA Conference. What an exciting time to be a music therapist as we embark on the 20th anniversary of AMTA and the 68th anniversary of music therapy! Our first priority is to honor the legacy of our beloved Director of Conferences and Communications, Al Bumanis, who passed away on September 30th (see page 87). Al will be with us in spirit here. We have so much to be proud of and celebrate. “Music Therapy for a Growing World” sets the stage for an exciting four days of the latest in practice, research, advocacy, and leadership. We all need time to grow, rejuvenate and “fill our cups,” which is the intent of this year’s conference. Many thanks to the conference planning team of Vice President, Kristen O’Grady, Vice-President Elect, Wendy Woolsey, AMTA national office staff, and, of course, to the Local Committee chaired by Mary Altom and Daniel Tague. Please join us at the Opening Session to help us celebrate Lifetime Achievement Award winners; on Friday morning for the State of the Association, Business Meeting, Member Recognition Awards, and Time of Remembrance; and on Friday night for a special concert with Kechi Okwuchi! We will also celebrate and honor Dr. -

Hottest 100 2012 Artists
2 Bears, The - Be Strong Angus Stone - Broken Brights 2 Bears, The - Bear Hug Angus Stone - Hold On {Like A Version} 2 Bears, The - Church Angus Stone - It Was Blue 2 Bears, The - Get Together Angus Stone - Monsters 2 Bears, The - Ghosts & Zombies Angus Stone - River Love 2 Bears, The - The Birds & The Bees Angus Stone - The Blue Door 2 Bears, The - Warm & Easy Angus Stone - Wooden Chair 2 Bears, The - Work Animal Collective - Today's Supernatural 360 - Run Alone Antlers, The - Endless Ladder 44th Sunset - Caesar Apes - Seven A-Trak - Disco Nap {ft. Oliver} Arctic Monkeys - R U Mine? Abbe May - Karmageddon Art Of Sleeping - Above The Water Active Child - Sweet Dreams {Like A Art Of Sleeping - Empty Hands Version} Arts Martial - Running Adrian Lux - Alive {ft. The Good Natured} Ash Grunwald - Longtime Aesop Rock - Zero Dark Thirty Ash Grunwald - Shake That Thing Afrojack & Steve Aoki - No Beef {ft. Miss Ash Grunwald - Trouble's Door Palmer} Asta - Escape Ainslie Wills - Stop Pulling The String Asta - My Heart Is On Fire Akido - Thirteen Aston Shuffle, The - Can't Stop Now Alabama Shakes - Hang Loose Atoms For Peace - Default Alabama Shakes - Hold On Austra - None Of Dem {Like A Version} Alabama Shakes - I Found You Avaberee - Lover Of Mine All That Glitters - This Sound Avicii - Silhouettes Allday x C1 - So Good Azealia Banks - 1991 Alphabet Botanical - A New Feeling Azealia Banks - Jumanji Alpine - All For One Bad Dreems - Chills Alpine - Gasoline Bad Religion - Fuck You Alpine - Lovers 2 Ball Park Music - Bad Taste Blues, Pt. 1 Alpine - Seeing Red Ball Park Music - Bad Taste Blues, Pt. -
GIVING: Huskies Respond to Need PACKING IT UP
THE TYRIAN Vol. 5 • No. 1 Mifflin County High School DECEMBER 2015 [email protected] GIVING: Huskies respond to need PACKING IT UP. Student Council ad- viser Krystena Brown and Key Club adviser Randy Fluke box up canned goods to be D distributed through Mother Hubbard’s Cupboard, the area food pantry. The canned food drive O brought in 3,301 individual items. O Many help; many helped Student Council, Key Club and the Science Department joined forces recently to benefit those near and far in need. Their efforts yielded the following results: R • 3,301 individual items for Mother Hubbard’s Cupboard • 95 foster children receiving gifts through The Giving Tree • Hundreds of books cleaned and sorted for Santa’s Bookbag T • More than $700 in scholarship money to future teachers* O SEED money raised for scholarships* A door-decorating contest sponsored by the Science Depart- ment and won by Aaron Bubb’s class (which raised more than $200) benefited SEED (Self-Empowerment through Education), a non-profit F group founded by Nate King, biology teacher. A former U.S. Peace Corps fisheries biologist in Zambia, King says of its purpose, “... several volunteers would leave the bush monthly to meet and resupply. While there we noticed Zambia’s teach- er training college was in Serenje. We wanted to give back to Zambia U with a more sustainable twist. “Many people donate things and have no idea what really hap- pens (very corrupt governments). Our money goes directly to pay tuition and room and board for four students for the year. -

Host's Master Artist List for Game 1
Host's Master Artist List for Game 1 You can play the list in the order shown here, or any order you prefer. Tick the boxes as you play the songs. Girls Aloud Liberty X Sean Paul Nelly Furtado Shakira Labrinth Michael Buble David Gray Holly Valance Baha Men Justin Timberlake Snoop Dogg Beyonce Good Charlotte Will Young Outkast Rihanna Robbie Williams Alicia Keys Basshunter Pussycat Dolls Black Eyed Peas Kaiser Chefs Corrs Razorlight The Fray Five Ella Henderson James Blunt S Club 7 Scooter Kelis Plan B Vengaboys Arctic Monkeys Dizzie Rascal Evanescence Elbow Busted Kings Of Leon Akon Jennifer Lopez Backstreet Boys Coldplay Eminem Gareth Gates Sophie Ellis-Bextor Stereophonics Shayne Ward Estelle Copyright QOD Page 1/28 Host's Master Artist List for Game 2 You can play the list in the order shown here, or any order you prefer. Tick the boxes as you play the songs. Michael Buble Coral Westlife Avril Lavigne Matt Cardle Duffy Elbow Shakira Liberty X Feeder Muse Vengaboys Fatboy Slim Kaiser Chefs Corrs Ting Tings Pussycat Dolls Enrique Iglesias JLS Lady Gaga Kid Rock Evanescence Dido Steps Ella Henderson Britney Spears Jay-Z Estelle KT Tunstall Lenny Kravitz Labrinth Kooks Snoop Dogg Linkin Park Emili Sande Plan B Nelly Robbie Williams James Blunt Nelly Furtado Justin Timberlake Gareth Gates Craid David Foo Fighters Daniel Powter Ne-Yo Hozier S Club 7 Nickelback Chemical Brothers Copyright QOD Page 2/28 Host's Master Artist List for Game 3 You can play the list in the order shown here, or any order you prefer. -

Emergency Preparedness and Response Planning for Child Care
STATE OF NEW MEXICO EARLY CHILDHOOD EDUCATION AND CARE DEPARTMENT Emergency Preparedness and Response Planning for Child Care Early Care, Education and Nutrition Division April 2021 New Mexico Emergency Preparedness and Response Planning Letter of Approval and Implementation TO: Early Childhood Education and Care Department, Early Care, Education and Nutrition Division (ECECD- ECEN) Child Care Regulatory Oversight Staff, ECEN Child Care Assistance Staff, ECECD Policy, Research and Quality Initiative Staff, New Mexico Kids Resource and Referral Agency and New Mexico Child Care Programs FROM: Early Childhood Education and Care Department, Early Care, Education and Nutrition Division SUBJECT: Letter of Promulgation, 2021 New Mexico State Emergency Preparedness and Response Planning for Child Care With this notice, we are pleased to put into effect the 2021 New Mexico State Emergency Preparedness and Response Plan for Early Childhood Education and Care Department (ECECD), Early Care, Education and Nutrition Division (ECEN). The plan provides the framework for preparedness and recovery activities for child care licensed providers, child care registered providers, and child care families in the event of a significant emergency or disaster in the State of New Mexico. This plan provides a structure to work in a coordinated effort during disaster recovery and provides guidance to licensed and registered child care providers (hereafter, “providers”), families, and stakeholders about what they can expect from Early Childhood Education and Care Department, Early Care, Education and Nutrition Division. This plan is complimentary to ECECD's Continuity of Operations Plans (COOP), and works with the overall statewide mitigation, preparedness, response, and recovery activities provided by the New Mexico Emergency Operations Plan (EOP). -

The Paradoxical Position of the White Rapper in Hip- Hop Music: a Genre Fixated on Authenticity
Faculteit Letteren & Wijsbegeerte Sofie Balliu The Paradoxical Position of the White Rapper in Hip- Hop Music: A Genre Fixated on Authenticity An Analysis of the Use of African-American English in the Music of Eminem, Iggy Azalea, and Classified Masterproef voorgedragen tot het behalen van de graad van Master in de taal- en letterkunde Duits – Engels 2015 Promotor Prof. Dr. Stef Slembrouck Vakgroep Engelse Taalkunde 1 I. Acknowledgements I would like to thank my supervisor prof. dr. Stef Slembrouck for allowing me to pursue the topic of hip-hop for my master’s dissertation. His insightful remarks have enabled me to think critically about a genre that I am fond of. Furthermore, his commentaries have influenced my thinking process and approach to hip-hop in general. I also want to thank my family for their support and my stepfather Luc in specific for his helpful reflections and valuable opinions that help shape mine. Moreover, I have enjoyed reading the works of other hip-hop scholars who have provided me with relevant knowledge as well as the website RapGenius. Finally, my appreciation goes out to the artists J. Cole, Eminem, Iggy Azalea, and Classified. J. Cole has produced an album that I count as one of my latest favorites, and the White rappers’ work has opened up my perspective on hip-hop music. 2 i. Acknowledgements…………………………………………....………………...3 ii. Table of Contents……………………………………...…………………………4 iii. List of Figures……………………………………………………………………6 PART I 1 Introduction……………………………………………………..……………………6 2 Introduction to Hip-hop………………………………...…………………………..10