Contrast Material
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Review Article Contrast Media Viscosity Versus Osmolality in Kidney Injury: Lessons from Animal Studies
Hindawi Publishing Corporation BioMed Research International Volume 2014, Article ID 358136, 15 pages http://dx.doi.org/10.1155/2014/358136 Review Article Contrast Media Viscosity versus Osmolality in Kidney Injury: Lessons from Animal Studies Erdmann Seeliger, Diana C. Lenhard, and Pontus B. Persson Institute of Physiology and Center for Cardiovascular Research, Charite-University´ Medicine Berlin, Campus Mitte, Hessische Straße 3-4, 10115 Berlin, Germany Correspondence should be addressed to Erdmann Seeliger; [email protected] Received 18 October 2013; Accepted 29 December 2013; Published 23 February 2014 Academic Editor: Richard Solomon Copyright © 2014 Erdmann Seeliger et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Iodinated contrast media (CM) can induce acute kidney injury (AKI). CM share common iodine-related cytotoxic features but differ considerably with regard to osmolality and viscosity. Meta-analyses of clinical trials generally failed to reveal renal safety differences of modern CM with regard to these physicochemical properties. While most trials’ reliance on serum creatinine as outcome measure contributes to this lack of clinical evidence, it largely relies on the nature of prospective clinical trials: effective prophylaxis by ample hydration must be employed. In everyday life, patients are often not well hydrated; here we lack clinical data. However, preclinical studies that directly measured glomerular filtration rate, intrarenal perfusion and oxygenation, and various markers of AKI have shown that the viscosity of CM is of vast importance. In the renal tubules, CM become enriched, as water is reabsorbed, but CM are not. -

EUROPEAN PHARMACOPOEIA 10.0 Index 1. General Notices
EUROPEAN PHARMACOPOEIA 10.0 Index 1. General notices......................................................................... 3 2.2.66. Detection and measurement of radioactivity........... 119 2.1. Apparatus ............................................................................. 15 2.2.7. Optical rotation................................................................ 26 2.1.1. Droppers ........................................................................... 15 2.2.8. Viscosity ............................................................................ 27 2.1.2. Comparative table of porosity of sintered-glass filters.. 15 2.2.9. Capillary viscometer method ......................................... 27 2.1.3. Ultraviolet ray lamps for analytical purposes............... 15 2.3. Identification...................................................................... 129 2.1.4. Sieves ................................................................................. 16 2.3.1. Identification reactions of ions and functional 2.1.5. Tubes for comparative tests ............................................ 17 groups ...................................................................................... 129 2.1.6. Gas detector tubes............................................................ 17 2.3.2. Identification of fatty oils by thin-layer 2.2. Physical and physico-chemical methods.......................... 21 chromatography...................................................................... 132 2.2.1. Clarity and degree of opalescence of -

The Risk of Contrast Media-Induced Ventricular Fibrillation Is Low in Canine Coronary Arteriography with Ioxilan
FULL PAPER Surgery The Risk of Contrast Media-Induced Ventricular Fibrillation is Low in Canine Coronary Arteriography with Ioxilan Kazuhiro MISUMI, Oki TATENO, Makoto FUJIKI, Naoki MIURA and Hiroshi SAKAMOTO Department of Veterinary Medicine, Kagoshima University, 21–24 Korimoto 1-chome, Kagoshima 890–0065, Japan (Received 5 August 1999/Accepted 28 December 1999) ABSTRACT. Previous studies have proposed that sodium supplement to nonionic contrast media (CM) can decrease the risk of ventricular fibrillation (VF). This study was designed to compare the occurence of VF induced by ioxilan (containing 9 mmol/LNa+) with other nonionic CMs. After wedging a catheter in the right coronary artery, test solutions including ioxilan, ioversol, iomeprol, and iopromide were infused for 30 sec at the rate of 0.4 ml/sec or until VF occurred. Then, incidence of VF, contact time (i.e. the time required to produce VF), and QTc were measured. Also, the CMs other than ioxilan were investigated at sodium levels adjusted to 9 and 20 mmol/L Na+. The incidence of VF with ioxilan (0% ) was the lowest of all. In the other CMs, the incidence decreased in accordance with increase of sodium. Iomeprol and iopromide showed significant reduction of VF incidence at the sodium level of 20 mmol/L. The higher sodium supplements also prolonged the contact times. The increase of QTc was the greatest in ioxilan. Ioxilan has the least arrythmogenic property among the current low-osmolality nonionic CMs. This property might be attributable to an optimal sodium concentration of 9 mmol/L in the CM.—KEY WORDS: contrast media, coronary arteriography, ioxilan, ventricular fibrillation. -

Alphabetical Listing of ATC Drugs & Codes
Alphabetical Listing of ATC drugs & codes. Introduction This file is an alphabetical listing of ATC codes as supplied to us in November 1999. It is supplied free as a service to those who care about good medicine use by mSupply support. To get an overview of the ATC system, use the “ATC categories.pdf” document also alvailable from www.msupply.org.nz Thanks to the WHO collaborating centre for Drug Statistics & Methodology, Norway, for supplying the raw data. I have intentionally supplied these files as PDFs so that they are not quite so easily manipulated and redistributed. I am told there is no copyright on the files, but it still seems polite to ask before using other people’s work, so please contact <[email protected]> for permission before asking us for text files. mSupply support also distributes mSupply software for inventory control, which has an inbuilt system for reporting on medicine usage using the ATC system You can download a full working version from www.msupply.org.nz Craig Drown, mSupply Support <[email protected]> April 2000 A (2-benzhydryloxyethyl)diethyl-methylammonium iodide A03AB16 0.3 g O 2-(4-chlorphenoxy)-ethanol D01AE06 4-dimethylaminophenol V03AB27 Abciximab B01AC13 25 mg P Absorbable gelatin sponge B02BC01 Acadesine C01EB13 Acamprosate V03AA03 2 g O Acarbose A10BF01 0.3 g O Acebutolol C07AB04 0.4 g O,P Acebutolol and thiazides C07BB04 Aceclidine S01EB08 Aceclidine, combinations S01EB58 Aceclofenac M01AB16 0.2 g O Acefylline piperazine R03DA09 Acemetacin M01AB11 Acenocoumarol B01AA07 5 mg O Acepromazine N05AA04 -

Delayed Adverse Reaction to Contrast-Enhanced CT: CONSTRAST MEDIA
Note: This copy is for your personal, non-commercial use only. To order presentation-ready copies for distribution to your colleagues or clients, contact us at www.rsna.org/rsnarights. Delayed Adverse Reaction to Contrast-enhanced CT: CONSTRAST MEDIA n A Prospective Single-Center Study Comparison to Control Group without Enhancement 1 ORIGINAL RESEARCH Shaun Loh , MD , MBA Purpose: To prospectively assess the incidence of delayed adverse Sepideh Bagheri , MD reactions (DARs) in patients undergoing contrast material– Richard W. Katzberg , MD enhanced computed tomography (CT) with the low osmo- Maxwell A. Fung , MD lar nonionic contrast agent iohexol and compare with the Chin-Shang Li , PhD incidence of DARs in patients undergoing unenhanced CT as control subjects. Materials and Institutional review board approval and informed written Methods: consent for this prospective study were obtained. The study was HIPAA compliant. Patients undergoing CT for routine indications were enrolled from a random next-available scheduling template by an on-site clinical trials monitor. All subjects received a questionnaire asking them to indicate any DAR occurring later than 1 hour after their examina- tion. Sixteen manifestations were listed and included rash, skin redness, skin swelling, nausea, vomiting, and dizziness, among others. To ensure maximal surveillance, a clinical tri- als coordinator initiated direct telephone contact for further assessment. Patients suspected of having moderately severe cutaneous reactions were invited to return for a complete dermatologic clinical assessment including skin biopsy, if in- dicated. Statistical analysis was performed by using a two- sided Wilcoxon-Mann-Whitney test, a logistic regression utilizing a x 2 test to adjust for sex and age, and a two-sided Fisher exact test. -

Structure and Properties of X-Ray Contrast Media
STRUCTURE AND PROPERTIES OF X-RAY CONTRAST MEDIA Optimal use of CM in radiology requires a knowl- edge of the nature and relevant properties of the available substances. This chapter describes the properties of currently used and newly developed contrast-giving agents that infuence their behav- ior in the human body, their side effects, and their practical utility. The main X-ray contrast agents in use today are insoluble barium sulfate for the diagnostic evalu- ation of the GI tract and water-soluble CM for the radiological assessment of the different vascular systems, body cavities and organs. In addition, a water-soluble CM based on tri-iodobenzene is the alternative agent of choice for oral use when bari- um sulfate is contraindicated. Barium Sulfate Barium is used in the form of the insoluble sulfate for radiography of the GI tract. If perforation is suspected, however, only water-soluble, iodinated agents (Gastrografn, Ultravist-370) can be used since the body is virtually incapable of eliminating barium sulfate once it has entered the peritoneum. Barium sulfate is available either as a powder to be prepared directly before use or as a ready-to-use suspension. For double-contrast examinations (fll- ing of the lumen with gas, coating of the wall with barium sulfate), barium sulfate is either mixed with a carbon dioxide additive, or a gas-forming agent is taken in addition. © The Author(s) 2018 20 U. Speck, X-Ray Contrast Media, https://doi.org/10.1007/978-3-662-56465-3_3 Common to all barium preparations is concentra- tion of barium sulfate which may diluted according to the needs of the examination. -
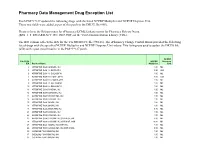
Pharmacy Data Management Drug Exception List
Pharmacy Data Management Drug Exception List Patch PSS*1*127 updated the following drugs with the listed NCPDP Multiplier and NCPDP Dispense Unit. These two fields were added as part of this patch to the DRUG file (#50). Please refer to the Release notes for ePharmacy/ECME Enhancements for Pharmacy Release Notes (BPS_1_5_EPHARMACY_RN_0907.PDF) on the VistA Documentation Library (VDL). The IEN column reflects the IEN for the VA PRODUCT file (#50.68). The ePharmacy Change Control Board provided the following list of drugs with the specified NCPDP Multiplier and NCPDP Dispense Unit values. This listing was used to update the DRUG file (#50) with a post install routine in the PSS*1*127 patch. NCPDP File 50.68 NCPDP Dispense IEN Product Name Multiplier Unit 2 ATROPINE SO4 0.4MG/ML INJ 1.00 ML 3 ATROPINE SO4 1% OINT,OPH 3.50 GM 6 ATROPINE SO4 1% SOLN,OPH 1.00 ML 7 ATROPINE SO4 0.5% OINT,OPH 3.50 GM 8 ATROPINE SO4 0.5% SOLN,OPH 1.00 ML 9 ATROPINE SO4 3% SOLN,OPH 1.00 ML 10 ATROPINE SO4 2% SOLN,OPH 1.00 ML 11 ATROPINE SO4 0.1MG/ML INJ 1.00 ML 12 ATROPINE SO4 0.05MG/ML INJ 1.00 ML 13 ATROPINE SO4 0.4MG/0.5ML INJ 1.00 ML 14 ATROPINE SO4 0.5MG/ML INJ 1.00 ML 15 ATROPINE SO4 1MG/ML INJ 1.00 ML 16 ATROPINE SO4 2MG/ML INJ 1.00 ML 18 ATROPINE SO4 2MG/0.7ML INJ 0.70 ML 21 ATROPINE SO4 0.3MG/ML INJ 1.00 ML 22 ATROPINE SO4 0.8MG/ML INJ 1.00 ML 23 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,5ML 5.00 ML 24 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,10ML 10.00 ML 25 ATROPINE SO4 1MG/ML INJ,AMP,1ML 1.00 ML 26 ATROPINE SO4 0.2MG/0.5ML INJ,AMP,0.5ML 0.50 ML 30 CODEINE PO4 30MG/ML -

OSMOVIST Iotrolan Injection
PRODUCT MONOGRAPH ® OSMOVIST Iotrolan Injection ® OSMOVIST 240 Iotrolan Injection 240 mg I/mL ® OSMOVIST 300 Iotrolan Injection 300 mg I/mL Dimeric Non-ionic Radiographic Contrast Medium For Myelography Bayer Inc. Date of Preparation: 77 Belfield Road April 11, 2007 Toronto, Ontario M9W 1G6 Canada www.bayer.ca Submission Control No.: 113334 © 2007, Bayer Inc. PRODUCT MONOGRAPH OSMOVIST® Iotrolan injection ® OSMOVIST 240 Iotrolan injection 240 mg I/mL ® OSMOVIST 300 Iotrolan injection 300 mg I/mL THERAPEUTIC CLASSIFICATION A Dimeric Non-ionic Radiographic Contrast Medium For Myelography ACTION and CLINICAL PHARMACOLOGY OSMOVIST (iotrolan) is a dimeric, non-ionic, hexaiodinated radiocontrast medium. The contrast-giving substance, iotrolan, is a dimer of triiodinated isophthalic acid derivatives, in which the firmly bound iodine absorbs the X-rays. Solutions of OSMOVIST 240 mg I/mL and 300 mg I/mL are isotonic to plasma and cerebrospinal fluid at radiologically useful iodine levels. After intrathecal administration, iotrolan is absorbed from cerebrospinal fluid (CSF) into the blood stream. The mean half-life of the transfer of iotrolan from the spinal fluid to the blood plasma was found to be 5.7 ± 6.0 hours in adults. The highest concentration of iodine in plasma occurred 3.5 ± 3.1 hours after intrathecal administration. Plasma protein binding at a concentration of 1.2 mg I/mL is 2.4%. The mean elimination half- Page 2 life of iotrolan in the plasma is 13.6 ± 13.9 hours (median of 9 hours). Approximately 50- 80% of the administered dose is excreted unmetabolized by the kidneys within 24 hours after administration, and approximately 90% within 72 hours. -

Contrast Agents in Pediatric Neuroimaging
Contrast Agents in Pediatric Neuroimaging Sylvester Chuang1 From the Hospital for Sick Children, Toronto, Ontario During the last two decades the development which substitutions are made at the acid group. of contrast agents for myelography, angiography, Examples of common contrast agents used in computed tomography (CT) and magnetic reso North America are listed in Table 1. nance imaging (MR) has been remarkable. What Recent developments have all centered on the follows is a review of contrast agents used in nonionic contrast agents, because these are less neuroradiology-specifically, the ionic and non toxic than the ionics (1); however, the cost of the ionic contrast agents for radiographic/CT proce nonionics is significantly higher than that of the dures, and the paramagnetic contrast agents used ionics. Despite the debate regarding the cost in MR studies. Topics covered are the indications effectiveness of the nonionics (2-9), we routinely for and use of contrast agents, doses and com use nonionic contrast agents for all radiologic parisons, complications and cost benefits, and investigations at the Hospital for Sick Children in what the future of contrast media might hold. Toronto. We do so because of the lower compli cation rate, although there is no convincing evi Iodinated Contrast Agents dence of any decrease in the mortality rate. Nevertheless, when there is extravasation of con The basic structure of iodinated contrast trast into the tissue on IV injection, the morbidity agents is the benzene ring (Fig. 1), with its at is lower. tached iodine atoms. The remaining components Elimination of contrast agents is dependent on are the acid group and organic substitutes which organic substitutions. -

Muscular and CNS Effects of Carotid Artery Administration of Contrast Media in Rabbits
143 Muscular and CNS Effects of Carotid Artery Administration of Contrast Media in Rabbits Christopher C. Whisson 1 Facial muscle twitching during intracarotid injections of nonionic contrast media has Charles A. Evill been observed in rabbits. To investigate the cause of this reaction, cortical EEG and Michael R. Sage facial EMG recordings were made from rabbits receiving selective internal and external Alan J . Wilson carotid artery injections of control solutions (normal saline, mannitol), an ionic contrast medium (meglumine iothalamate), and three nonionic contrast media (iohexol, iopro mide, ::tnd iotrolan). Internal carotid artery injections with all contrast media, both ionic and nonionic, produced ipsilateral EEG changes in 24 of 28 animals; however, ipsilateral EMG changes and visible twitching were observed only in animals injected with nonionic contrast media. Internal carotid artery injections with control ionic and nonionic solutions (physiological saline and mannitol, respectively) produced no EEG changes in any animals. Mannitol produced only ipsilateral EMG changes and visible twitching in most animals. The severity of the reaction to mannitol was generally less than that to the nonionic contrast media, and this difference was statistically significant when comparing mannitol with iohexol and iotrolan but not with iopromide. External carotid artery injections with nonionic solutions (contrast media and mannitol) produced significantly more severe ipsilateral EMG changes and visible twitching than were recorded with the internal carotid artery injections. Ionic solutions (contrast media and saline) had no effect. EEG changes were not observed after external carotid artery injection of any solution, with the exception of two of the seven animals injected with iotrolan. Angiog raphy demonstrated retrograde filling of the external carotid arterial system from internal carotid artery injection via functioning orbital anastamoses. -

Important Note:All Human Products Must Be Of
* Important Note:All human products must be of human recombinant origin wherever these are available in the market *For oral solution it is preferable:Syrup then Suspension and then Elixir MOH CODE ITEM NAME Qty 1 CARDIOVASCULAR SYSTEM 1A Positive inotropic drugs 1Aa Digtalis glycoside 02-01-00001 digoxin tab 62.5 mcg 800,000 02-01-00002 digitoxin tab 100 mcg 800,000 02-01-00003 digoxin tab 125 mcg 800,000 02-01-00004 digoxin tab 250 mcg 30,415,200 02-01-00005 digoxin PG elixir 50mcg /ml 800,000 02-01-00006 digoxin inj 250 mcg/ml, (2ml amp) 800,000 1Ab PHOSPHODIESTERASE INHIBITORS 02-01-00007 Enoximone inj 5mg/ml (20ml amp) 800,000 1B DIURETICS 02-01-00008 amiloride Hcl 5mg + hydrochlorthiazide 50mg tab 50,000,000 02-01-00009 bumetanide tab 1 mg 1,094,000 02-01-00010 chlorthalidone tab 50mg 3,264,000 02-01-00011 ethacrynic acid as sod.salt inj powder for 800,000 reconstitution 50mg vial 02-01-00012 frusemide inj 20mg/2ml amp 5,780,400 02-01-00013 frusemide I.V. infusion inj 10mg/ml, (25ml amp) 800,000 02-01-00014 frusemide tab 40mg 25,000,000 02-01-00015 frusemide scored tab 500mg 800,000 02-01-00016 frusemide oral solution pead liquid 1mg/1ml 800,000 02-01-00017 frusemide oral solution 4mg/ml 800,000 02-01-00018 frusemide oral solution 8mg/ml 800,000 02-01-00019 hydrochlorothiazide tab 25mg 1,084,000 02-01-00020 hydrochlorothiazide tab 50mg 1,396,000 02-01-00021 indapamide tab 2.5mg 800,000 02-01-00022 Indapamide s/r coated tab 1.5mg 800,000 02-01-00023 spironolactone tab 25mg 5,568,400 02-01-00024 spironolactone tab 100mg 5,147,200