Guidelines on the Use of Iodinated Contrast Media in Patients with Kidney Disease 2012 – Digest Version – JSN, JRS and JCS Joint Working Group
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacologyonline 2: 727-753 (2010) Ewsletter Bradu and Rossini
Pharmacologyonline 2: 727-753 (2010) ewsletter Bradu and Rossini COTRAST AGETS - IODIATED PRODUCTS. SECOD WHO-ITA / ITA-OMS 2010 COTRIBUTIO O AGGREGATE WHO SYSTEM-ORGA CLASS DISORDERS AD/OR CLUSTERIG BASED O REPORTED ADVERSE REACTIOS/EVETS Dan Bradu and Luigi Rossini* Servizio Nazionale Collaborativo WHO-ITA / ITA-OMS, Università Politecnica delle Marche e Progetto di Farmacotossicovigilanza, Azienda Ospedaliera Universitaria Ospedali Riuniti di Ancona, Regione Marche, Italia Summary From the 2010 total basic adverse reactions and events collected as ADRs preferred names in the WHO-Uppsala Drug Monitoring Programme, subdivided in its first two twenty years periods as for the first seven iodinated products diagnostic contrast agents amidotrizoate, iodamide, iotalamate, iodoxamate, ioxaglate, iohexsol and iopamidol, their 30 WHO-system organ class disorders (SOCDs) aggregates had been compared. Their common maximum 97% levels identified six SOCDs only, apt to evaluate the most frequent single ADRs for each class, and their percentual normalization profiles for each product. The WILKS's chi square statistics for the related contingency tables, and Gabriel’s STP procedure applied to the extracted double data sets then produced profile binary clustering, as well as Euclidean confirmatory plots. They finally showed similar objectively evaluated autoclassificative trends of these products, which do not completely correspond to their actual ATC V08A A, B and C subdivision: while amidotrizoate and iotalamate, and respectively iohesol and iopamidol are confirmed to belong to the A and B subgroups, ioxaglate behaves fluctuating within A, B and C, but iodamide looks surprizingly, constantly positioned together with iodoxamate as binary/ternary C associated. In view of the recent work of Campillos et al (Science, 2008) which throws light on the subject, the above discrepancies do not appear anymore unexpected or alarming. -

Clinical Practice Guidelines for Diagnosis and Management Of
REVIEWS Clinical Practice Guidelines for Diagnosis and Management of Hypersensitivity Reactions to Contrast Media Rosado Ingelmo A1, Doña Diaz I2, Cabañas Moreno R3, Moya Quesada MC4, García-Avilés C5, García Nuñez I6, Martínez Tadeo JI7, Mielgo Ballesteros R8, Ortega-Rodríguez N9, Padial Vilchez MA10, Sánchez-Morillas L11, Vila Albelda C1, Moreno Rodilla E12*, Torres Jaén MJ2* 1Unidad de Alergia, Hospital Universitario Fundación Alcorcón, Alcorcón, Madrid, Spain 2Allergy Unit, IBIMA-Regional University Hospital of Málaga, UMA, Málaga, Spain 3Department of Allergy, Hospital La Paz, Health Research Institute (IdiPAZ), Madrid, Spain 4Sección de Alergia CH Torrecárdenas, Almería, Spain 5Unidad de Alergia, Hospital Moncloa, Madrid, Spain 6Servicio de Alergología, Hospital Quirón Málaga, Málaga, Spain 7Servicio de Alergología, Hospital Universitario Ntra Sra de Candelaria, Santa Cruz de Tenerife, Tenerife, Spain 8Servicio de Alergología, Hospital Universitario 12 de Octubre, Madrid, Spain 9Servicio de Alergia, Hospital Universitario de Gran Canaria Dr Negrín, Las Palmas de Gran Canaria, Spain 10Servicio de Alergologia, Hospital Infanta Sofía, San Sebastián de los Reyes, Madrid, Spain 11Servicio de Alergologia, Hospital Clínico San Carlos, Madrid, Spain 12Servicio de Alergología, Complejo Asistencial Universitario de Salamanca, Salamanca, Spain *Both authors contributed equally to this study. On behalf of the Drug Allergy Committee of Spanish Society of Allergy and Clinical Immunology (SEAIC) J Investig Allergol Clin Immunol 2016; Vol. 26(3): 144-155 doi: 10.18176/jiaci.0058 Abstract The objective of these guidelines is to ensure efficient and effective clinical practice. The panel of experts who produced this consensus document developed a research protocol based on a review of the literature. The prevalence of allergic reactions to iodinated contrast media (ICM) is estimated to be 1:170 000, that is, 0.05%-0.1% of patients undergoing radiologic studies with ICM (more than 75 million examinations per year worldwide). -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Review Article Contrast Media Viscosity Versus Osmolality in Kidney Injury: Lessons from Animal Studies
Hindawi Publishing Corporation BioMed Research International Volume 2014, Article ID 358136, 15 pages http://dx.doi.org/10.1155/2014/358136 Review Article Contrast Media Viscosity versus Osmolality in Kidney Injury: Lessons from Animal Studies Erdmann Seeliger, Diana C. Lenhard, and Pontus B. Persson Institute of Physiology and Center for Cardiovascular Research, Charite-University´ Medicine Berlin, Campus Mitte, Hessische Straße 3-4, 10115 Berlin, Germany Correspondence should be addressed to Erdmann Seeliger; [email protected] Received 18 October 2013; Accepted 29 December 2013; Published 23 February 2014 Academic Editor: Richard Solomon Copyright © 2014 Erdmann Seeliger et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Iodinated contrast media (CM) can induce acute kidney injury (AKI). CM share common iodine-related cytotoxic features but differ considerably with regard to osmolality and viscosity. Meta-analyses of clinical trials generally failed to reveal renal safety differences of modern CM with regard to these physicochemical properties. While most trials’ reliance on serum creatinine as outcome measure contributes to this lack of clinical evidence, it largely relies on the nature of prospective clinical trials: effective prophylaxis by ample hydration must be employed. In everyday life, patients are often not well hydrated; here we lack clinical data. However, preclinical studies that directly measured glomerular filtration rate, intrarenal perfusion and oxygenation, and various markers of AKI have shown that the viscosity of CM is of vast importance. In the renal tubules, CM become enriched, as water is reabsorbed, but CM are not. -

Proceedings of the Fifty-Eighth Annual Meeting of the American Society for Clinical Investigation, Inc., Held in Atlantic City, N.J., May 2, 1966: Abstracts
Proceedings of the Fifty-Eighth Annual Meeting of the American Society for Clinical Investigation, Inc., Held in Atlantic City, N.J., May 2, 1966: Abstracts J Clin Invest. 1966;45(6):980-1037. https://doi.org/10.1172/JCI105414. Research Article Find the latest version: https://jci.me/105414/pdf ABSTRACTS Comparison of Effects of Alpha Adrenergic Blockade luminescence. Inhibition of ATPase activities by ouabain, on Resistance and Capacitance Vessels. FRANCOIS parachloromercuribenzoate (PCMB), and parachloro- M. ABBOUD * AND JOHN W. ECKSTEIN,* Iowa City, mercuribenzenesulfonate (PCMBS) was studied. ¶1 Mem- Iowa. brane ATPase of osmotically prepared platelet "ghosts" A foreleg of each of 20 dogs was perfused with blood is composed of Na+-K+-Mg++-dependent ATPase (15 to at a constant rate through the brachial artery. The 30%) and Mg++-activated ATPase (60 to 85%o). Ouabain nerves of the brachial plexus were transected, and an (10' M), which inhibits the Na+-K--dependent ATPase electrode was applied to their distal ends. Pressures were activity and produces a resultant loss of cellular K+, gain recorded simultaneously from the brachial artery and of Na+, and cell swelling, does not inhibit either ADP cephalic vein and from a small artery and small vein in aggregation or clot retraction. ¶f PCMB, an organic the paw. Pressor responses to injections of nor- mercurial compound that diffuses into cells, totally inacti- epinephrine (1, 2, and 4 /.tg) into the brachial artery and vates both ATPase activities in the ghost preparations to nerve stimulation (3, 6, and 12 cps) were measured and in the intact platelet. -

Evaluation Report Radiocontrast Agents
Evaluation report Radiocontrast agents Report No. 187 Within the strategy aimed at reducing micro-pollutant inputs originating from ur- ban and industrial waste water, evaluation reports are being drafted for 10 groups of substances targeted at summarizing scientifi c and technical facts and at pointing out gaps of knowledge. Also, the evaluation reports present a variety of possible mea- sures at the source (e.g. registration of substances, limitation of uses) and technical measures in crucial wastewater treatment plants (e.g. introducing a further treatment stage). The “Conclusions” of the evaluation reports list the most effi cient measures to be further investigated into within a holistic ICPR strategy. However, these measures are no recommendations the ICPR addresses to its member states. Measures listed in this chapter will be integrated into a survey report of all measures in order to be able to take into account eventual synergetic effects of measures (effects of measures on different groups of substances) when proceeding with the fi nal evaluation. Based on the fi nal evaluation of all measures the ICPR will determine recommendations for the Member States Imprint Publisher: International Commission for the Protection of the Rhine (ICPR) Kaiserin-Augusta-Anlagen 15, D 56068 Koblenz P.O. box 20 02 53, D 56002 Koblenz Telephone +49-(0)261-94252-0, Fax +49-(0)261-94252-52 Email: [email protected] www.iksr.org ISBN 935324-53-7 © IKSR-CIPR-ICBR 2010 IKSR CIPR ICBR Evaluation report Radiocontrast agents 1. Introduction Radiocontrast agents are used for diagnostic purposes, as they absorb X-rays to a greater extent than human soft tissue and thus visualize these tissues. -
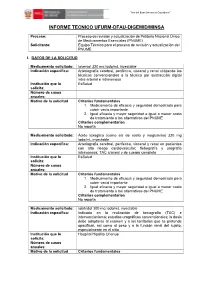
Informe Tecnico Ufurm-Dfau-Digemid/Minsa
“Año del Buen Servicio al Ciudadano” ” INFORME TECNICO UFURM-DFAU-DIGEMID/MINSA Proceso: Proceso de revisión y actualización de Petitorio Nacional Único de Medicamentos Esenciales (PNUME) Solicitante: Equipo Técnico para el proceso de revisión y actualización del PNUME I. DATOS DE LA SOLICITUD Medicamento solicitado: Ioversol 320 mg Iodo/mL inyectable Indicación específica: Arteriografía cerebral, periférica, visceral y renal utilizando las técnicas convencionales o la técnica por sustracción digital intra-arterial e intravenosa Institución que lo EsSalud solicita: Número de casos anuales: Motivo de la solicitud Criterios fundamentales 1. Medicamento de eficacia y seguridad demostrada para cubrir vacío importante. 2. Igual eficacia y mayor seguridad e igual o menor costo de tratamiento a las alternativas del PNUME Criterios complementarios No reporta Medicamento solicitado: Ácido ioxaglico (como sal de sodio y meglumina) 320 mg Iodo/mL inyectable Indicación específica: Arteriografia cerebral, periferica, visceral y renal en pacientes con alto riesgo cardiovascular; flebografía y urografía intravenosa; TAC craneal y de cuerpo completo Institución que lo EsSalud solicita: Número de casos anuales: Motivo de la solicitud Criterios fundamentales 1. Medicamento de eficacia y seguridad demostrada para cubrir vació importante. 2. Igual eficacia y mayor seguridad e igual o menor costo de tratamiento a las alternativas del PNUME Criterios complementarios No reporta Medicamento solicitado: Iobitridol 300 mg Iodo/mL inyectable Indicación específica: Indicado en la realización de tomografía (TAC) e intervencionismo; estudios urográficos convencionales; la dosis debe adaptarse al examen y a los territorios que se pretende opacificar, asi como al peso y a la función renal del sujeto, especialmente en el niño Institución que lo Hospital Hipólito Unanue solicita: Número de casos anuales: Motivo de la solicitud Criterios fundamentales “Año del Buen Servicio al Ciudadano” ” 1. -

EUROPEAN PHARMACOPOEIA 10.0 Index 1. General Notices
EUROPEAN PHARMACOPOEIA 10.0 Index 1. General notices......................................................................... 3 2.2.66. Detection and measurement of radioactivity........... 119 2.1. Apparatus ............................................................................. 15 2.2.7. Optical rotation................................................................ 26 2.1.1. Droppers ........................................................................... 15 2.2.8. Viscosity ............................................................................ 27 2.1.2. Comparative table of porosity of sintered-glass filters.. 15 2.2.9. Capillary viscometer method ......................................... 27 2.1.3. Ultraviolet ray lamps for analytical purposes............... 15 2.3. Identification...................................................................... 129 2.1.4. Sieves ................................................................................. 16 2.3.1. Identification reactions of ions and functional 2.1.5. Tubes for comparative tests ............................................ 17 groups ...................................................................................... 129 2.1.6. Gas detector tubes............................................................ 17 2.3.2. Identification of fatty oils by thin-layer 2.2. Physical and physico-chemical methods.......................... 21 chromatography...................................................................... 132 2.2.1. Clarity and degree of opalescence of -

Radiocontrast Agent Diatrizoic Acid Induces Mitophagy and Oxidative Stress Via Calcium Dysregulation
International Journal of Molecular Sciences Article Radiocontrast Agent Diatrizoic Acid Induces Mitophagy and Oxidative Stress via Calcium Dysregulation Dakota B. Ward, Kathleen C. Brown and Monica A. Valentovic * Department of Biomedical Sciences, Toxicology Research Cluster, Joan C. Edwards School of Medicine, Marshall University, 1 Marshall Drive, Huntington, WV 25755, USA * Correspondence: [email protected]; Tel.: +1-304-696-7332; Fax: +1-304-696-7391 Received: 20 May 2019; Accepted: 18 August 2019; Published: 21 August 2019 Abstract: Contrast-induced acute kidney injury (CI-AKI) is the third most common cause of hospital associated kidney damage. Potential mechanisms of CI-AKI may involve diminished renal hemodynamics, inflammatory responses, and direct cytotoxicity. The hypothesis for this study is that diatrizoic acid (DA) induces direct cytotoxicity to human proximal tubule (HK-2) cells via calcium dysregulation, mitochondrial dysfunction, and oxidative stress. HK-2 cells were exposed to 0–30 mg I/mL DA or vehicle for 2–24 h. Conversion of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) and trypan blue exclusion indicated a decrease in mitochondrial and cell viability within 2 and 24 h, respectively. Mitochondrial dysfunction was apparent within 8 h post exposure to 15 mg I/mL DA as shown by Seahorse XF cell mito and Glycolysis Stress tests. Mitophagy was increased at 8 h by 15 mg I/mL DA as confirmed by elevated LC3BII/I expression ratio. HK-2 cells pretreated with calcium level modulators BAPTA-AM, EGTA, or 2-aminophenyl borinate abrogated DA-induced mitochondrial damage. DA increased oxidative stress biomarkers of protein carbonylation and 4-hydroxynonenol (4HNE) adduct formation. -

The Risk of Contrast Media-Induced Ventricular Fibrillation Is Low in Canine Coronary Arteriography with Ioxilan
FULL PAPER Surgery The Risk of Contrast Media-Induced Ventricular Fibrillation is Low in Canine Coronary Arteriography with Ioxilan Kazuhiro MISUMI, Oki TATENO, Makoto FUJIKI, Naoki MIURA and Hiroshi SAKAMOTO Department of Veterinary Medicine, Kagoshima University, 21–24 Korimoto 1-chome, Kagoshima 890–0065, Japan (Received 5 August 1999/Accepted 28 December 1999) ABSTRACT. Previous studies have proposed that sodium supplement to nonionic contrast media (CM) can decrease the risk of ventricular fibrillation (VF). This study was designed to compare the occurence of VF induced by ioxilan (containing 9 mmol/LNa+) with other nonionic CMs. After wedging a catheter in the right coronary artery, test solutions including ioxilan, ioversol, iomeprol, and iopromide were infused for 30 sec at the rate of 0.4 ml/sec or until VF occurred. Then, incidence of VF, contact time (i.e. the time required to produce VF), and QTc were measured. Also, the CMs other than ioxilan were investigated at sodium levels adjusted to 9 and 20 mmol/L Na+. The incidence of VF with ioxilan (0% ) was the lowest of all. In the other CMs, the incidence decreased in accordance with increase of sodium. Iomeprol and iopromide showed significant reduction of VF incidence at the sodium level of 20 mmol/L. The higher sodium supplements also prolonged the contact times. The increase of QTc was the greatest in ioxilan. Ioxilan has the least arrythmogenic property among the current low-osmolality nonionic CMs. This property might be attributable to an optimal sodium concentration of 9 mmol/L in the CM.—KEY WORDS: contrast media, coronary arteriography, ioxilan, ventricular fibrillation. -

Alphabetical Listing of ATC Drugs & Codes
Alphabetical Listing of ATC drugs & codes. Introduction This file is an alphabetical listing of ATC codes as supplied to us in November 1999. It is supplied free as a service to those who care about good medicine use by mSupply support. To get an overview of the ATC system, use the “ATC categories.pdf” document also alvailable from www.msupply.org.nz Thanks to the WHO collaborating centre for Drug Statistics & Methodology, Norway, for supplying the raw data. I have intentionally supplied these files as PDFs so that they are not quite so easily manipulated and redistributed. I am told there is no copyright on the files, but it still seems polite to ask before using other people’s work, so please contact <[email protected]> for permission before asking us for text files. mSupply support also distributes mSupply software for inventory control, which has an inbuilt system for reporting on medicine usage using the ATC system You can download a full working version from www.msupply.org.nz Craig Drown, mSupply Support <[email protected]> April 2000 A (2-benzhydryloxyethyl)diethyl-methylammonium iodide A03AB16 0.3 g O 2-(4-chlorphenoxy)-ethanol D01AE06 4-dimethylaminophenol V03AB27 Abciximab B01AC13 25 mg P Absorbable gelatin sponge B02BC01 Acadesine C01EB13 Acamprosate V03AA03 2 g O Acarbose A10BF01 0.3 g O Acebutolol C07AB04 0.4 g O,P Acebutolol and thiazides C07BB04 Aceclidine S01EB08 Aceclidine, combinations S01EB58 Aceclofenac M01AB16 0.2 g O Acefylline piperazine R03DA09 Acemetacin M01AB11 Acenocoumarol B01AA07 5 mg O Acepromazine N05AA04 -

Delayed Adverse Reaction to Contrast-Enhanced CT: CONSTRAST MEDIA
Note: This copy is for your personal, non-commercial use only. To order presentation-ready copies for distribution to your colleagues or clients, contact us at www.rsna.org/rsnarights. Delayed Adverse Reaction to Contrast-enhanced CT: CONSTRAST MEDIA n A Prospective Single-Center Study Comparison to Control Group without Enhancement 1 ORIGINAL RESEARCH Shaun Loh , MD , MBA Purpose: To prospectively assess the incidence of delayed adverse Sepideh Bagheri , MD reactions (DARs) in patients undergoing contrast material– Richard W. Katzberg , MD enhanced computed tomography (CT) with the low osmo- Maxwell A. Fung , MD lar nonionic contrast agent iohexol and compare with the Chin-Shang Li , PhD incidence of DARs in patients undergoing unenhanced CT as control subjects. Materials and Institutional review board approval and informed written Methods: consent for this prospective study were obtained. The study was HIPAA compliant. Patients undergoing CT for routine indications were enrolled from a random next-available scheduling template by an on-site clinical trials monitor. All subjects received a questionnaire asking them to indicate any DAR occurring later than 1 hour after their examina- tion. Sixteen manifestations were listed and included rash, skin redness, skin swelling, nausea, vomiting, and dizziness, among others. To ensure maximal surveillance, a clinical tri- als coordinator initiated direct telephone contact for further assessment. Patients suspected of having moderately severe cutaneous reactions were invited to return for a complete dermatologic clinical assessment including skin biopsy, if in- dicated. Statistical analysis was performed by using a two- sided Wilcoxon-Mann-Whitney test, a logistic regression utilizing a x 2 test to adjust for sex and age, and a two-sided Fisher exact test.