Rabies CASES IMMEDIATELY (Also Known As Hydrophobia and Lyssa)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Most Effective Tool to Prevent Human Brucellosis
Chapter 13 Control of Animal Brucellosis — The Most Effective Tool to Prevent Human Brucellosis Marta Pérez-Sancho, Teresa García-Seco, Lucas Domínguez and Julio Álvarez Additional information is available at the end of the chapter http://dx.doi.org/10.5772/61222 Abstract The World Health Organization classifies brucellosis as one of the seven neglected en‐ demic zoonosis which contribute to the perpetuation of poverty in developing coun‐ tries. Although most of the developed countries are free from this important zoonosis, brucellosis has still a widespread distribution in the Mediterranean region, the Middle East, Central Asia, and parts of Latin America, making it a global problem. Nearly half a million of new cases of human brucellosis are reported each year around the world, in which animals (or products of animal origin) are the most likely source of infection. Brucella melitensis, the main etiologic agent of small ruminant brucellosis, is the most prevalent specie involved in cases of human disease in most parts of the world. Additionally, Brucella abortus (main responsible of bovine brucellosis) and Bru‐ cella suis (the most common etiological agent of porcine brucellosis) are often associat‐ ed with human brucellosis. In animal production, brucellosis has a strong economic impact due not only to its direct consequences (e.g., reproductive failures) but also to indirect loses (e.g., trade restrictions). The problem of brucellosis could be considered a clear example of the need for a “One World, One Health” strategy, given that the only approach to achieve its control and subsequent eradication is the cooperation be‐ tween public and animal health authorities. -

Humanitarian Assistance for Wild Animals
Thoughts Humanitarian Assistance for Wild Animals Kyle Johannsen argues that most wild animals live bad lives, and we should intervene in nature to improve their wellbeing When you read the title of this paper, what ergy, and attract the attention of predators, likely comes to mind is images of Koala by singing for prolonged periods of time. bears being rescued from bush fires, or of Being encumbered isn’t good for peacocks, injured raccoons and deer, being rehabili- and exposing themselves to danger isn’t tated after a hurricane. These are examples good for songbirds. Rather, the function of of humanitarian assistance for wild animals, heavy feathers and prolonged singing, is to but they’re not what this paper is primar- protect the birds’ genes by attracting mates. ily about. The need for humanitarian as- Mating, and reproducing, may be enjoy- sistance in the wild far exceeds the damage able for these animals, but surely evolution caused by natural disasters. Severe suffering would have facilitated these goals some oth- is pervasive in nature. It’s built into natural er way if the purpose of evolved traits were processes, and thus it’s the norm rather than to benefit the animals who have them. the exception. Since the purpose of evolution is to protect genes, you’d think that a parent’s evolved traits at least function to benefit Severe suffering is her children. Unfortunately, protecting an pervasive in nature animals’ genes doesn’t always benefit her children either. After all, many animals are r-strategists: they protect their genes Many people think that evolution is an by producing large numbers of offspring. -

Using Cross-Species Vaccination Approaches to Counter Emerging
PERSPECTIVES adjuvant combinations to inform ‘go’ or ‘no- go’ decisions with regard to subsequent Using cross- species vaccination development of promising vaccine candidates (Fig. 1). approaches to counter emerging Most human infectious diseases have an animal origin, with more than 70% of infectious diseases emerging infectious diseases that affect humans initially crossing over from 8 George M. Warimwe , Michael J. Francis , Thomas A. Bowden, animals . Generating wider knowledge of how pathogens behave in animals can Samuel M. Thumbi and Bryan Charleston give indications of how to develop control Abstract | Since the initial use of vaccination in the eighteenth century, our strategies for human diseases, and vice understanding of human and animal immunology has greatly advanced and a wide versa. ‘One Health vaccinology’, a concept in which synergies in human and veterinary range of vaccine technologies and delivery systems have been developed. The immunology are identified and exploited COVID-19 pandemic response leveraged these innovations to enable rapid for vaccine development, could transform development of candidate vaccines within weeks of the viral genetic sequence our ability to control such emerging being made available. The development of vaccines to tackle emerging infectious infectious diseases. Due to similarities in diseases is a priority for the World Health Organization and other global entities. host–pathogen interactions, the natural More than 70% of emerging infectious diseases are acquired from animals, with animal hosts of a zoonotic infection may be the most appropriate model to study the some causing illness and death in both humans and the respective animal host. Yet disease and evaluate vaccine performance9. -
Professional Guidance for Animal Bites and Rabies Control
December 6, 2004 MEMORANDUM TO: State Public Health Veterinarians State Epidemiologists State Veterinarians Other Parties Interested in Rabies Prevention and Control FROM: Mira J. Leslie, D.V.M., M.P.H, Co-Chair Compendium of Animal Rabies Prevention and Control Committee SUBJECT: Compendium of Animal Rabies Prevention and Control, 2005 The National Association of State Public Health Veterinarians (NASPHV) is pleased to provide the 2005 revision of the Compendium of Animal Rabies Prevention and Control for your use and for distribution to practicing veterinarians and officials in animal control, public health, wildlife management and agriculture in your state. This cover memo summarizes the changes that were made to the document this year. COMPENDIUM CHANGES The section Principles of Rabies Prevention and Control (formerly Part II) is now Part I of the document and Recommendations for Parenteral Rabies Vaccination Procedures is Part II. Part III: Rabies Vaccines Licensed and Marketed in the U.S., 2005 has been updated. The following feline combination vaccine products are no longer available: IMRAB 3 + Feline 3; IMRAB 3 +Feline 4; PUREVAX Feline 3/ Rabies+LEUCAT; ECLIPSE 3 + FeLV/R; ECLIPSE 4+FeLV/R; Fel-O-Guard 3+ FeLV/R; and Fel-O-Guard 4+FeLV/R. The definition of a rabies exposure in Part I.A.1. has been clarified and a new sentence is added to direct questions concerning possible rabies exposures to local and state public health authorities. During 2004, there were two recognized importations of rabid dogs into the United States, one from Puerto Rico (mongoose rabies variant that is readily transmitted dog-to-dog) and one from Thailand (canine rabies virus variant). -
SEARG Report 2001
W. H. O. PROCEEDINGS OF THE SOUTHERN AND EASTERN AFRICAN RABIES GROUP / WORLD HEALTH ORGANIZATION MEETING SUDAN ERITREA ETHIOPIA UGANDA RWANDA KENYA BURUNDI TANZANIA MALAWI ZAMBIA MOZAMBIQUE ZIMBABWE MADAGASCAR BOTSWANA NAMIBIA SWAZILAND LESOTHO SOUTH AFRICA LILONGWE, MALAWI – 18-22 JUNE 2001 Sixth SEARG meeting, Lilongwe 18-21 June 2001 Official opening CONTENTS OFFICIAL OPENING PROGRAMME OF THE MEETING .............................................................................................................................. 4 Southern and Eastern African Rabies Group conference Lilongwe MALAWI: 18 to 21 June 2001 ................... 4 OPENING SPEECH................................................................................................................................................... 7 OPENING SPEECH................................................................................................................................................... 9 OPENING SPEECH................................................................................................................................................. 10 COUNTRY REPORTS RABIES IN BOTSWANA......................................................................................................................................... 13 RABIES IN BURUNDI IN 1999 AND 2000............................................................................................................... 17 RABIES IN ERITREA ............................................................................................................................................ -

1 WORLD SMALL ANIMAL VETERINARY ASSOCIATION 2015 VACCINATION GUIDELINES for the OWNERS and BREEDERS of DOGS and CATS WSAVA Vacci
WORLD SMALL ANIMAL VETERINARY ASSOCIATION 2015 VACCINATION GUIDELINES FOR THE OWNERS AND BREEDERS OF DOGS AND CATS WSAVA Vaccination Guidelines Group M.J. Day (Chairman) School of Veterinary Sciences University of Bristol, United Kingdom M.C. Horzinek (Formerly) Department of Microbiology, Virology Division University of Utrecht, the Netherlands R.D. Schultz Department of Pathobiological Sciences University of Wisconsin-Madison, United States of America R. A. Squires James Cook University, Queensland, Australia 1 CONTENTS Introduction.......................................................................................3 Major infectious diseases of the dog and cat....................................5 The immune response......................................................................21 The principle of vaccination..............................................................29 Types of vaccine...............................................................................32 Drivers for change in vaccination protocols......................................35 Canine vaccination guidelines..........................................................37 Feline vaccination guidelines…………………………………………..46 Reporting of adverse reactions.........................................................51 Glossary of terms..............................................................................57 2 INTRODUCTION Vaccination of dogs and cats protects them from infections that may be lethal or cause serious disease. Vaccination is a safe and efficacious -

Chapter 12 RABIES and CONTINUED MILITARY CONCERNS
Rabies and Continued Military Concerns Chapter 12 RABIES AND CONTINUED MILITARY CONCERNS NICOLE CHEVALIER, DVM, MPH,* AND KARYN HAVAS, DVM, PhD† INTRODUCTION A Historical Perspective The US Military’s Involvement ETIOLOGY AND EPIDEMIOLOGY Rabies Virus Variants and Distribution Rabies-free Definition and Areas Rabies Transmission Process and Conditions CLINICAL REVIEW Clinical Signs of Rabies in Animals Diagnosis of Rabies in Animals Animal Management After Bites from Rabies Suspects Human Postexposure Treatment for Rabies PREVENTION AND CONTROL Animal Vaccination Human Vaccination Military Animal Bite Reports Surveillance RABIES IN AN OPERATIONAL ENVIRONMENT Difficulties Posed by Certain Animal Populations Stray Animal Control Efforts in Afghanistan and Iraq Global Lessons Learned About Stray Animal Control Measures INTERNATIONALLY SUPPORTED RABIES CONTROL PROGRAMS Rabies Surveillance Mass Parenteral Vaccination Oral Vaccination Population Management Euthanasia Human Preexposure Vaccination Human Postexposure Prophylaxis RABIES CONTROL IN FUTURE CONTIGENCY OPERATIONS SUMMARY *Lieutenant Colonel, Veterinary Corps, US Army; Veterinary Capabilities Developer, Directorate of Combat and Doctrine Development, 2377Greeley Road, Building 4011, Joint Base San Antonio-Fort Sam Houston, Texas 78234 †Major, Veterinary Corps, US Army; Veterinary Epidemiologist, US Army Public Health Command, Armed Forces Health Surveillance Center, 503 Robert Grant Avenue, Silver Spring, Maryland 20910 345 Military Veterinary Services INTRODUCTION A Historical Perspective -

Interim Clinical Considerations for North American Companion-Animal Vaccination Practice During the COVID-19 Pandemic Richard B
Interim clinical considerations for North American companion-animal vaccination practice during the COVID-19 pandemic Richard B. Ford, DVM, MS, DACVIM, DACVPM (Hon), lead editor, 2017 AAHA Canine Vaccination Guidelines Link V. Welborn, DVM, DABVP, CCRT, chair, 2017 AAHA Canine Vaccination Guidelines Laurie J. Larson, DVM, task force member, 2017 AAHA Canine Vaccination Guidelines Amy Stone, DVM, PhD, chair, 2020 AAHA/AAFP Feline Vaccination Guidelines In the face of the global coronavirus pandemic, and as emphasis on social distancing and sheltering-in- place continue to limit client and patient access to routine veterinary care, the following considerations have been developed to address vaccination protocols for dogs and cats seen in clinical practice. At the time of this writing, it is not possible to predict when exposure risk for humans to the novel coronavirus SARS-CoV-2 will end. Therefore, it is the responsibility of the individual veterinarian to determine when conventional vaccination schedules can be reinstated for the population of patients seen in the practice. If pets are presented for vaccinations that are deemed a priority, other wellness care, including additional vaccinations as appropriate, could be provided as long as there is not an increased risk of coronavirus exposure for people. General considerations • The health and safety of veterinary personnel and clientele during the course of the COVID-19 pandemic is a priority. Therefore, amended vaccination schedules for dogs and cats should be considered. • The impact of social distancing and self-imposed travel restrictions on exposure risk of dogs and cats to infectious disease is not known. However, it can be assumed that certain groups, based on age, geography, and/or environment, do have sustained risk that justifies priority consideration for vaccination (see tables below). -
Section IV: Preventive Medicine and Public Health Services
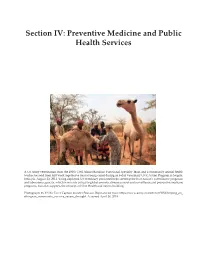
Veterinary Support in the Irregular Warfare Environment Section IV: Preventive Medicine and Public Health Services A US Army veterinarian from the 490th Civil Affairs Battalion Functional Specialty Team and a community animal health worker (second from left) work together to treat a young camel during an 8-day Veterinary Civic Action Program in Negele, Ethiopia, August 23, 2011. Using deployed US veterinary personnel helps develop the host nation’s surveillance programs and laboratory capacity, which is not only critical to global zoonotic disease control and surveillance and preventive medicine programs, but also supports the concepts of One Health and nation-building. Photograph: by US Air Force Captain Jennifer Pearson. Reproduced from: https://www.army.mil/article/65682/helping_an_ ethiopian_community_survive_severe_drought. Accessed April 26, 2018. 273 Military Veterinary Services 274 Zoonotic and Animal Diseases of Military Importance Chapter 11 ZOONOTIC AND ANIMAL DISEASES OF MILITARY IMPORTANCE RONALD L. BURKE, DVM, DRPH; TAYLOR B. CHANCE, DVM; KARYN A. HAVAS, DVM, PHD; SAMUEL YINGST, DVM, PhD; PAUL R. FACEMIRE, DVM; SHELLEY P. HONNOLD, DVM, PhD; ERIN M. LONG, DVM; BRETT J. TAYLOR, DVM, MPH; REBECCA I. EVANS, DVM, MPH; ROBIN L. BURKE, DVM, MPH; CONNIE W. SCHMITT, DVM; STEPHANIE E. FONSECA, DVM; REBECCA L. BAXTER, DVM; MICHAEL E. MCCOWN, DVM, MPH; A. RICK ALLEMAN, DVM, PhD; KATHERINE A. SAYLER; LARA S. COTTE, DVM; CLAIRE A. CORNELIUS, DVM, PhD; AUDREY C. MCMILLAN-COLE, DVM, MPVM; KARIN HAMILTON, DVM, MPH; AND KELLY G. VEST, DVM, -

Human Rabies Encephalitis Prevention and Treatment: Progress Since Pasteur’S Discovery Laurent Dacheux, Olivier Delmas, Hervé Bourhy
Human rabies encephalitis prevention and treatment: progress since Pasteur’s discovery Laurent Dacheux, Olivier Delmas, Hervé Bourhy To cite this version: Laurent Dacheux, Olivier Delmas, Hervé Bourhy. Human rabies encephalitis prevention and treat- ment: progress since Pasteur’s discovery. Infectious Disorders - Drug Targets, Bentham Science Publishers, 2011, 11 (3), pp.251–299. 10.2174/187152611795768079. pasteur-01491353 HAL Id: pasteur-01491353 https://hal-pasteur.archives-ouvertes.fr/pasteur-01491353 Submitted on 21 Apr 2017 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Distributed under a Creative Commons Attribution - NonCommercial - ShareAlike| 4.0 International License TITLE Human Rabies Encephalitis Prevention and Treatment: Progress Since Pasteur’s Discovery RUNNING TITLE Prevention and Treatment of Human Rabies Received 3 November 2010; revised 24 December 2010; accepted 10 January 2011. 1/115 ABSTRACT Rabies remains one of the most ancient and deadly of human infectious diseases. This viral zoonosis is transmitted principally by the saliva of infected dogs, inducing a form of encephalomyelitis that is almost invariably fatal. Since the first implementation, by Louis Pasteur in 1885, of an efficient preventive post-exposure treatment, more effective protocols and safer products have been developed, providing almost 100% protection if administered early enough. -

Concern for Wild Animal Suffering and Environmental Ethics: What Are the Limits of the Disagreement? Oscar Horta
Document generated on 09/30/2021 11:09 p.m. Les ateliers de l'éthique The Ethics Forum CONCERN FOR WILD ANIMAL SUFFERING AND ENVIRONMENTAL ETHICS: WHAT ARE THE LIMITS OF THE DISAGREEMENT? OSCAR HORTA Volume 13, Number 1, Winter 2018 Article abstract This paper examines the extent of the opposition between environmentalists URI: https://id.erudit.org/iderudit/1055119ar and those concerned with wild-animal suffering and considers whether there DOI: https://doi.org/10.7202/1055119ar are any points they may agree on. The paper starts by presenting the reasons to conclude that suffering and premature death prevail over positive well-being See table of contents in nature. It then explains several ways to intervene in order to aid animals and prevent the harms they suffer, and claims that we should support them. In particular, the paper argues in favour of carrying out more research to learn Publisher(s) the best ways to intervene without causing more harm to other animals and to intervene first in areas significantly transformed by human action. It then Centre de recherche en éthique de l’Université de Montréal examines what positions environmentalist views can have towards intervention in nature for the sake of animals. It claims that, while ecocentric ISSN and naturocentric views will strongly oppose intervention in certain circumstances, they should not do so in other cases in which the values they 1718-9977 (digital) promote are not at stake or might be outweighed. The paper then argues that, contrary to what it might seem at first, biocentric views should strongly Explore this journal support intervention. -

Compendium of Animal Rabies Prevention and Control, 2016
Public Veterinary Medicine: Public Health Compendium of Animal Rabies Prevention and Control, 2016 National Association From the Massachusetts Department of Public Health, 305 South St, Jamaica Plain, of State Public Health Veterinarians MA 02130 (Brown); the New York City Department of Health and Mental Hygiene, Compendium of Animal Rabies Prevention 2 Gotham Center, CN# 22A, 42-09 28th St, Queens, NY 11101 (Slavinski); the New and Control Committee Mexico Department of Health, 1190 St Francis Dr, Room N-1350, Santa Fe, NM 87502 (Ettestad); and the Texas Department of State Health Services, PO Box 149347, MC Catherine M. Brown DVM, MSc, MPH (Co-Chair) 1956, Austin, TX 78714 (Sidwa). Sally Slavinski DVM, MPH (Co-Chair) Consultants to the Committee: Jesse Blanton, PhD (CDC, 1600 Clifton Rd, Mailstop G-33, Atlanta, GA 30333); Richard B. Chipman, MS, MBA (USDA APHIS Wildlife Paul Ettestad DVM, MS Services, 59 Chenell Dr, Ste 2, Concord, NH 03301); Rolan D. Davis, MS (Kansas State Tom J. Sidwa DVM, MPH University, Room 1016 Research Park, Manhattan, KS 66506); Cathleen A. Hanlon, VMD, PhD (Retired); Jamie McAloon Lampman (McKamey Animal Center, 4500 N Access Faye E. Sorhage VMD, MPH Rd, Chattanooga, TN 37415 [representing the National Animal Care and Control Association]); Joanne L. Maki, DVM, PhD (Merial a Sanofi Co, 115 Trans Tech Dr, Athens, GA 30601 [representing the Animal Health Institute]); Michael C. Moore, DVM, MPH (Kansas State University, Room 1016 Research Park, Manhattan, KS 66506); Jim Powell, MS (Wisconsin State Laboratory of Hygiene, 465 Henry Mall, Madison, WI 53706 [representing the Association of Public Health Laboratories]); Charles E.