Transforming Our Communities Consultation Document (Full Version) July 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Trade Directories 1822-23 & 1833-4 North Yorkshire, Surnames
Trade Directories 1822-23 & 1833-4 North Yorkshire, surnames beginning with P-Q DATE SNAME FNAME / STATUS OCCUPATIONS ADDITIONAL ITEMS PLACE PARISH or PAROCHIAL CHAPELRY 1822-1823 Page Thomas farmer Cowton North Gilling 1822-1823 Page William victualler 'The Anchor' Bellmangate Guisborough 1822-1823 Page William wood turner & line wheel maker Bellmangate Guisborough 1833-1834 Page William victualler 'The Anchor' Bellmangate Guisborough 1833-1834 Page Nicholas butcher attending Market Richmond 1822-1823 Page William Sagon attorney & notary agent (insurance) Newbrough Street Scarborough 1822-1823 Page brewer & maltster Tanner Street Scarborough 1822-1823 Paley Edmund, Reverend AM vicar Easingwold Easingwold 1833-1834 Paley Henry tallow chandler Middleham Middleham 1822-1823 Palliser Richard farmer Kilvington South Kilvington South 1822-1823 Palliser Thomas farmer Kilvington South Kilvington South 1822-1823 Palliser William farmer Pickhill cum Roxby Pickhill 1822-1823 Palliser William lodging house Huntriss Row Scarborough 1822-1823 Palliser Charles bricklayer Sowerby Thirsk 1833-1834 Palliser Charles bricklayer Sowerby Thirsk 1833-1834 Palliser Henry grocery & sundries dealer Ingram Gate Thirsk 1822-1823 Palliser James bricklayer Sowerby Thirsk 1833-1834 Palliser James bricklayer Sowerby Thirsk 1822-1823 Palliser John jnr engraver Finkle Street Thirsk 1822-1823 Palliser John snr clock & watch maker Finkle Street Thirsk 1822-1823 Palliser Michael whitesmith Kirkgate Jackson's Yard Thirsk 1833-1834 Palliser Robert watch & clock maker Finkle -
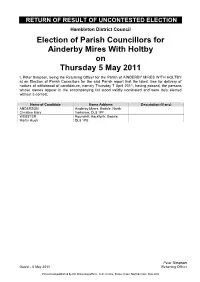
Return of Result of Uncontested Election
RETURN OF RESULT OF UNCONTESTED ELECTION Hambleton District Council Election of Parish Councillors for Ainderby Mires With Holtby on Thursday 5 May 2011 I, Peter Simpson, being the Returning Officer for the Parish of AINDERBY MIRES WITH HOLTBY at an Election of Parish Councillors for the said Parish report that the latest time for delivery of notices of withdrawal of candidature, namely Thursday 7 April 2011, having passed, the persons whose names appear in the accompanying list stood validly nominated and were duly elected without a contest. Name of Candidate Home Address Description (if any) ANDERSON Ainderby Myers, Bedale, North Christine Mary Yorkshire, DL8 1PF WEBSTER Roundhill, Hackforth, Bedale, Martin Hugh DL8 1PB Dated Friday 5 September 2014 Peter Simpson Dated – 5 May 2011 Returning Officer Printed and published by the Returning Officer, Civic Centre, Stone Cross, Northallerton, DL6 2UU RETURN OF RESULT OF UNCONTESTED ELECTION Hambleton District Council Election of Parish Councillors for Aiskew - Aiskew on Thursday 5 May 2011 I, Peter Simpson, being the Returning Officer for the Parish Ward of AISKEW - AISKEW at an Election of Parish Councillors for the said Parish Ward report that the latest time for delivery of notices of withdrawal of candidature, namely Thursday 7 April 2011, having passed, the persons whose names appear in the accompanying list stood validly nominated and were duly elected without a contest. Name of Candidate Home Address Description (if any) LES Forest Lodge, 94 Bedale Road, Carl Anthony Aiskew, Bedale -

CHAPTER 1 Arrowheads
THE MILLENNIUM BOOK OF TOPCLIFFE John M. Graham The MILLENNIUM BOOK OF TOPCLIFFE John M. Graham This book was sponsored by Topcliffe Parish Council who provided the official village focus group around which the various contributors worked and from which an application was made for a lottery grant. It has been printed and collated with the assistance of a grant from the Millennium Festival Awards for All Committee to Topcliffe Parish Council from the Heritage Lottery Fund. First published 2000 Reprinted May 2000 Reprinted September 2000 Reprinted February 2001 Reprinted September 2001 Copyright John M. Graham 2000 Published by John M. Graham Poppleton House, Front Street Topcliffe, Thirsk, North Yorkshire YQ7 3NZ ISBN 0-9538045-0-X Printed by Kall Kwik, Kall Kwik Centre 1235 134 Marton Road Middlesbrough TS1 2ED Other Books by the same Author: Voice from Earth, Published by Robert Hale 1972 History of Thornton Le Moor, Self Published 1983 Inside the Cortex, Published by Minerva 1996 Introduction The inspiration for writing "The Millennium Book of Topcliffe" came out of many discussions, which I had with Malcolm Morley about Topcliffe's past. The original idea was to pull together lots of old photographs and postcards and publish a Topcliffe scrapbook. However, it seemed to me to be also an opportunity to have another look at the history of Topcliffe and try to dig a little further into the knowledge than had been written in other histories. This then is the latest in a line of Topcliffe's histories produced by such people as J. B. Jefferson in his history of Thirsk in 1821, Edmund Bogg in his various histories of the Vale of Mowbray and Mary Watson in her Topcliffe Book in the late 1970s. -

Parish Profile 16-05-13
The Benefice of Harton The Benefice of Harton Parish Profiles St. Michael’s - Crambe St. Botolph’s - Bossall St. John’s - Buttercrambe St. Lawrence - Flaxton All Saints - Foston St. Mary’s - Gate Helmsley St. Mary’s - Sand Hutton St. John’s - Howsham St. Peter’s - Upper Helmsley St. Mary’s - Sand Hutton St. John’s - Whitwell The Benefice of Harton 2 The Benefice of Harton Contents Page Introduction 4 St Botolph’s – Bossall 10 St Lawrence – Flaxton 12 St John’s – Howsham 14 St John’s – Whitwell 18 Map of Benefice showing individual parishes 20 All Saints – Foston 22 Foston Primary School 24 St Michael’s – Crambe 25 St Peter’s – Upper Helmsley 28 St Mary’s – Sand Hutton 30 Vicarage – Sand Hutton 32 Sand Hutton Primary School 33 St Mary’s – Gate Helmsley 34 St John’s – Buttercrambe 36 Local Authority Data 38 Some Local Data 39 3 The Benefice of Harton Parish Profiles Introduction We are proud to present this document which describes the Benefice of Harton, with its 8 parishes, now structured within a Joint PCC. The setting The Benefice is situated in North Yorkshire, eight to ten miles to the north east of the historic city of York. Its constituent communities are dispersed along the A64 and A166 trunk roads, which lead respectively to Scarborough and Bridlington. The setting is rural and idyllic, attracting many tourists; some of the parishes contain areas of special scientific interest, others areas of outstanding natural beauty. The nearby city of York encompasses history, academe (two Universities, a Law College and a Medical School), culture, the arts, music and theatre. -

Hambleton Sustainability Appraisal Agenda Supplement for Cabinet, 02
Public Document Pack AGENDA Page No 6. LOCAL PLAN PUBLICATION CONSULTATION 1 - 234 This report seeks approval of the Hambleton Local Plan: Publication Draft and Policies Map, attached at Annex 1 and 2 of the report, for formal publication, representations and submission to the Secretary of State for public examination. It also seeks approval for publication of the Local Development Scheme. In accepting the recommendations, Cabinet will approve and recommend to Council that the Hambleton Local Development Scheme is published; the Hambleton Local Plan: Publication Draft as attached at Annex 1 and the Policies Map at Annex 2 of the report are approved for the purpose of publication for representations to be made commencing on or around the 23rd July 2019; the Sustainability Appraisal and Infrastructure Delivery Plan are published for consultation; the Director of Planning and Economy be authorised to make minor amendments and graphical improvements that (taken together) do not materially affect the policies set out in the Local Plan prior to publication; in the event of modifications being required to the Hambleton Local Plan: Publication Draft or supporting documentation prior to its submission, the Director of Economy and Planning in consultation with the Portfolio Holder for Economy and Planning be authorised to make these changes and undertake any necessary pre- submission consultation; and following the period of representation the Hambleton Local Plan: Publication Draft and Policies Map, proposed minor modifications and all relevant -

Station Travel Plan Thirsk
Station Travel Plan Thirsk ____________________________________________________________________________________________________________________________________________________________ TransPennine Express. Station Travel Plan. Thirsk. Version 1.1. Published 31/03/2017. Author: Charlie French, Transport Integration Manager TransPennine Express Station Travel Plans have been produced in line with guidance issued by the Association of Train Operators (ATOC). All information contained within the Station Travel Plan is correct as of the date of publishing. Station Travel Plans will be updated and republished on the anniversary of the publishing date above. Station Travel Plan Thirsk ______________________________________________________________________________________________ Introduction What is a Station Travel Plan? The Department for Transport defines as Station Travel Plan as: ‘A strategy for managing the travel generated by your organisation, with the aim of reducing its environmental impact, typically involving support for walking, cycling, public transport and car sharing’ Over the next two years, TransPennine Express is undertaking Station Travel Plans for the 19 stations where they are currently the Station Facility Owner (SFO). Why Develop a Station Travel Plan? Demand for rail is growing. More people are choosing to travel by rail and demand has risen to its highest point since 1920, and it is set to keep on rising, with predictions that demand will more than double within the next 30 years. This increase means that more and more people are travelling to and from our stations, with cars often being the number one choice for getting to/from the station, either parked up or for drop off/pick up. All of this meaning that car parking and suitable infrastructure for drop off/pick up is becoming a major issue for our customers. -

Areas Designated As 'Rural' for Right to Buy Purposes
Areas designated as 'Rural' for right to buy purposes Region District Designated areas Date designated East Rutland the parishes of Ashwell, Ayston, Barleythorpe, Barrow, 17 March Midlands Barrowden, Beaumont Chase, Belton, Bisbrooke, Braunston, 2004 Brooke, Burley, Caldecott, Clipsham, Cottesmore, Edith SI 2004/418 Weston, Egleton, Empingham, Essendine, Exton, Glaston, Great Casterton, Greetham, Gunthorpe, Hambelton, Horn, Ketton, Langham, Leighfield, Little Casterton, Lyddington, Lyndon, Manton, Market Overton, Martinsthorpe, Morcott, Normanton, North Luffenham, Pickworth, Pilton, Preston, Ridlington, Ryhall, Seaton, South Luffenham, Stoke Dry, Stretton, Teigh, Thistleton, Thorpe by Water, Tickencote, Tinwell, Tixover, Wardley, Whissendine, Whitwell, Wing. East of North Norfolk the whole district, with the exception of the parishes of 15 February England Cromer, Fakenham, Holt, North Walsham and Sheringham 1982 SI 1982/21 East of Kings Lynn and the parishes of Anmer, Bagthorpe with Barmer, Barton 17 March England West Norfolk Bendish, Barwick, Bawsey, Bircham, Boughton, Brancaster, 2004 Burnham Market, Burnham Norton, Burnham Overy, SI 2004/418 Burnham Thorpe, Castle Acre, Castle Rising, Choseley, Clenchwarton, Congham, Crimplesham, Denver, Docking, Downham West, East Rudham, East Walton, East Winch, Emneth, Feltwell, Fincham, Flitcham cum Appleton, Fordham, Fring, Gayton, Great Massingham, Grimston, Harpley, Hilgay, Hillington, Hockwold-Cum-Wilton, Holme- Next-The-Sea, Houghton, Ingoldisthorpe, Leziate, Little Massingham, Marham, Marshland -

Yorkshire Swale Flood History 2013
Yorkshire Swale flood history 2013 Sources The greater part of the information for the River Swale comes from a comprehensive PhD thesis by Hugh Bowen Willliams to the University of Leeds in 1957.He in turn has derived his information from newspaper reports, diaries, local topographic descriptions, minutes of Local Authority and Highway Board and, further back in time, from Quarter Sessions bridge accounts. The information is supplemented by various conversations which Williams had with farmers who owned land adjacent to the river. Where possible the height of the flood at the nearest cross- section of the place referred to in the notes is given. This has either been levelled or estimated from the available data. Together with the level above Ordnance Datum (feet) and the section in question there is given (in brackets) the height of the flood above normal water level. Information is also included from the neighbouring dales (mainly Wensleydale and Teesdale) as this gives some indication of conditions in Swaledale. Williams indicates that this is by no means a complete list, but probably contains most of the major floods in the last 200 years, together with some of the smaller ones in the last 70 years. Date and Rainfall Description sources 11 Sep 1673 Spate carried away dwelling house at Brompton-on-Swale. Burnsell Bridge on the Wharfe was washed away. North Riding Selseth Bridge in the Parish of Ranbaldkirke became ruinous by reason of the late great storm. Quarter Sessions (NRQS) ? Jul 1682 Late Brompton Bridge by the late great floods has fallen down. NRQS Speight(1891) Bridge at Brompton-on-Swale was damaged. -

Rolston House, Sandhutton, YO7 4RW Guide Price
Rolston House, Sandhutton, YO7 4RW Guide price £335,000 www.joplings.com We are delighted to welcome to the market this attractive three bedroomed country cottage situated the popular village of Sandutton. Rolston House is beautifully presented throughout and offers an excellent living accommodation. The village of Sandhutton is approximately 5 miles from the market town of Thirsk and offers easy access to Northallerton, A1 and A19. Accommodation comprises: entrance hall, kitchen, dining area, utility, cloakroom, lounge, study/ sitting room, three bedrooms and house bathroom. There is a private walled garden to the rear and off road parking. Viewing is highly recommended. CHAIN FREE. www.joplings.com DIRECTIONS UTILITY BEDROOM THREE From Thirsk, follow the A61 through the village Composite door to rear. UPVC windows to rear Two UPVC windows to the front and side. of Carlton Miniott turning right onto Sandhutton and side. Range of hand painted base units with Radiator. Lane. Follow this road through the village and solid wood work surfaces. Belfast sink with mixer Rolston House is located on the right hand side tap. Recessed lighting. Extractor fan. Radiator. HOUSE BATHROOM approximately 40 yards from the junction. Space for tumble dryer. Space for American fridge Two opaque UPVC windows to side and rear. A freezer. white bathroom suite which comprises: roll top ENTRANCE PORCH bath with hand held shower, shower cubicle, W.C. Entry to the home is through a glazed timber door. CLOAKROOM Pedestal sink. Part panelled walls. Towel radiator. Windows to three aspects and a glazed door to the High level W.C. Hand wash basin. -

(& Stanwick St. John & Caldwell) Ampleforth Appleton Wiske Ar
Monumental Inscriptions. The Centre for Local Studies, at Darlington Library has an extensive collection of Monumental Inscriptions compiled by the Cleveland, South Durham and North Yorkshire Family History Society. Acklam (Middlesbrough) Ainderby Steeple Aislaby Aldborough (& Stanwick St. John & Caldwell) Ampleforth Appleton Wiske Arkendale Arkengarthdale Arkletown, Wesleyan Chapel & St. Mary, Langthwaite Arkengarthdale (Yrks) Askrigg Auckland Auckland, St Andrew Auckland, St Andrew Extension Auckland, St Andrew (fiche) Aucklandshire and Weardale (Hearth Tax 1666) Aycliffe (see also School Aycliffe & U429AYCb LHOS Stephenson Way) Aysgarth Bagby Bainbridge Bainbridge and Carperby Baldersby Barnard Castle (St Mary/Roman Catholic/Victoria Road) Barningham Barton Bedale Bellerby Billingham Bilsdale Bilsdale Midcable Birkby Bishop Middleham Bishopton Boltby Bolton on Swale Boosbeck Bowes Bransdale (& Carlton) Brignall 13/07/2015 Brompton (near Northallerton) Brompton Cemetery (near Northallerton) Brotton Burneston Carlbury Carlton Miniott Carton in Cleveland Castle Eden Castleton Catterick Cleasby Coatham Cockfield Cold Kirby Commondale Coniscliffe (Carlbury) Carlbury (see Coniscliffe) Cornforth Cotherstone Coverham Cowesby Cowton (See East Cowton/South Cowton) Croxdale, St Bartholomew Coxwold Crakehall Crathorne Croft on Tees Cundall Dalby Dalton in Topcliffe Danby Danby Wiske Darlington Deaf Hill Deighton Denton Dinsdale Dishforth Downholme Easby Easington East Cowton (See Cowton) East Harsley (East) Loftus East Rounton East Witton 13/07/2015 -

Heritage at Risk Register 2015, Yorkshire
Yorkshire Register 2015 HERITAGE AT RISK 2015 / YORKSHIRE Contents Heritage at Risk III The Register VII Content and criteria VII Criteria for inclusion on the Register IX Reducing the risks XI Key statistics XIV Publications and guidance XV Key to the entries XVII Entries on the Register by local planning XIX authority Cumbria 1 Yorkshire Dales (NP) 1 East Riding of Yorkshire (UA) 1 Kingston upon Hull, City of (UA) 23 North East Lincolnshire (UA) 23 North Lincolnshire (UA) 25 North Yorkshire 27 Craven 27 Hambleton 28 Harrogate 33 North York Moors (NP) 37 Richmondshire 45 Ryedale 48 Scarborough 64 Selby 67 Yorkshire Dales (NP) 71 South Yorkshire 74 Barnsley 74 Doncaster 76 Peak District (NP) 79 Rotherham 80 Sheffield 83 West Yorkshire 86 Bradford 86 Calderdale 91 Kirklees 96 Leeds 101 Wakefield 107 York (UA) 110 II Yorkshire Summary 2015 e have 694 entries on the 2015 Heritage at Risk Register for Yorkshire, making up 12.7% of the national total of 5,478 entries. The Register provides an Wannual snapshot of historic sites known to be at risk from neglect, decay or inappropriate development. Nationally, there are more barrows on the Register than any other type of site. The main risk to their survival is ploughing. The good news is that since 2014 we have reduced the number of barrows at risk by over 130, by working with owners and, in particular, Natural England to improve their management. This picture is repeated in Yorkshire, where the greatest concentration of barrows at risk is in the rich farmland of the Wolds. -

Prospectus-Sandhutton.Pdf
Sand Hutton Church of England Primary School Sand Hutton York YO41 1LB Tel: 01904 468308 Email: [email protected] Headteacher: Mrs. Beverley Pawson WELCOME TO SAND HUTTON SCHOOL At Sand Hutton Staff and governors aim to provide a stimulating and challenging environment in which every child is able to achieve their full potential. We see the successful education of every child as being very much a partnership between home and school. Please remember that you are very welcome to talk to us at any time, particularly if you have any concerns. Good communication between us starts here. Throughout your child’s education here at Sand Hutton School we will keep you up to date and informed of their progress and development. If you are considering sending your child to our school, you are very welcome to look round. Please telephone to make an appointment. In the meantime, do not hesitate to contact us if you have any questions. Best wishes B.Pawson Beverley Pawson Headteacher Sand Hutton Church of England (V.C.) Primary School Prospectus Contents: Page no: 3. Mission Statement, Rationale 4. Our School, What our children say about their school 5. Statement of Aims and Value 6. Members of staff 7. Governing Body 8. School Hours, Organisation 9. Admissions, Starting School 10. Starting School continued 11. Pastoral Care 12. School Curriculum, Assessment 13. The curriculum subjects, English, Mathematics 14. Science, History, Geography; D &T, Art & Craft, Music 15. Religious Education, ICT 16. French, Physical Education/Sporting Activities; 17. SEN, Collective Worship 18. PSHCE, Homework 19.