Diagnosis & Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

External Link Teacher Pack
Episode 32 Questions for discussion 13th November 2018 US Midterm Elections 1. Briefly summarise the BTN US Midterm Elections story. 2. What are the midterm elections? 3. How many seats are in the House of Representatives? 4. How many of these seats went up for re-election? 5. What are the names of the major political parties in the US? 6. What words would you use to describe their campaigns? 7. The midterm elections can decide which party has the power in ____________. 8. Before the midterms President Trump had control over both the houses. True or false? 9. About how many people vote in the US President elections? a. 15% b. 55% c. 90% 10. What do you understand more clearly since watching the BTN story? Write a message about the story and post it in the comments section on the story page. WWF Living Planet Report 1. In pairs, discuss the WWF Living Planet Report story and record the main points of the discussion. 2. Why are scientists calling the period since the mid-1900s The Great Acceleration? 3. What is happening to biodiversity? 4. Biodiversity includes… a. Plants b. Animals c. Bacteria d. All of the above 5. What percentage of the planet’s animals have been lost over the last 40 years? 6. What do humans depend on healthy ecosystems for? 7. What organisation released the report? 8. What does the report say we need to do to help the situation? 9. How did this story make you feel? 10. What did you learn watching the BTN story? Check out the WWF Living Planet Report resource on the Teachers page. -

The Human Planet
INTRODUCTION: THE HUMAN PLANET our and a half billion years ago, out of the dirty halo of cosmic dust left over from the creation of our sun, a spinning clump of minerals F coalesced. Earth was born, the third rock from the sun. Soon after, a big rock crashed into our planet, shaving a huge chunk off, forming the moon and knocking our world on to a tilted axis. The tilt gave us seasons and currents and the moon brought ocean tides. These helped provide the conditions for life, which first emerged some 4 billion years ago. Over the next 3.5 billion years, the planet swung in and out of extreme glaciations. When the last of these ended, there was an explosion of complex multicellular life forms. The rest is history, tattooed into the planet’s skin in three-dimensional fossil portraits of fantastical creatures, such as long-necked dinosaurs and lizard birds, huge insects and alien fish. The emergence of life on Earth fundamentally changed the physics of the planet.1 Plants sped up the slow 1 429HH_tx.indd 1 17/09/2014 08:22 ADVENTURES IN THE ANTHROPOCENE breakdown of rocks with their roots, helping erode channels down which rainfall coursed, creating rivers. Photosynthesis transformed the chemistry of the atmosphere and oceans, imbued the Earth system with chemical energy, and altered the global climate. Animals ate the plants, modifying again the Earth’s chemistry. In return, the physical planet dictated the biology of Earth. Life evolves in response to geological, physical and chemical conditions. In the past 500 million years, there have been five mass extinctions triggered by supervolcanic erup- tions, asteroid impacts and other enormous planetary events that dramatically altered the climate.2 After each of these, the survivors regrouped, proliferated and evolved. -

The Columbian Exchange: a History of Disease, Food, and Ideas
Journal of Economic Perspectives—Volume 24, Number 2—Spring 2010—Pages 163–188 The Columbian Exchange: A History of Disease, Food, and Ideas Nathan Nunn and Nancy Qian hhee CColumbianolumbian ExchangeExchange refersrefers toto thethe exchangeexchange ofof diseases,diseases, ideas,ideas, foodfood ccrops,rops, aandnd populationspopulations betweenbetween thethe NewNew WorldWorld andand thethe OldOld WWorldorld T ffollowingollowing thethe voyagevoyage ttoo tthehe AAmericasmericas bbyy ChristoChristo ppherher CColumbusolumbus inin 1492.1492. TThehe OldOld WWorld—byorld—by wwhichhich wwee mmeanean nnotot jjustust EEurope,urope, bbutut tthehe eentirentire EEasternastern HHemisphere—gainedemisphere—gained fromfrom tthehe CColumbianolumbian EExchangexchange iinn a nnumberumber ooff wways.ays. DDiscov-iscov- eeriesries ooff nnewew ssuppliesupplies ofof metalsmetals areare perhapsperhaps thethe bestbest kknown.nown. BButut thethe OldOld WWorldorld aalsolso ggainedained newnew staplestaple ccrops,rops, ssuchuch asas potatoes,potatoes, sweetsweet potatoes,potatoes, maize,maize, andand cassava.cassava. LessLess ccalorie-intensivealorie-intensive ffoods,oods, suchsuch asas tomatoes,tomatoes, chilichili peppers,peppers, cacao,cacao, peanuts,peanuts, andand pineap-pineap- pplesles wwereere aalsolso iintroduced,ntroduced, andand areare nownow culinaryculinary centerpiecescenterpieces inin manymany OldOld WorldWorld ccountries,ountries, namelynamely IItaly,taly, GGreece,reece, andand otherother MediterraneanMediterranean countriescountries (tomatoes),(tomatoes), -
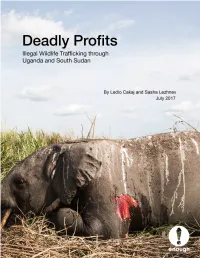
Deadly Profits: Illegal Wildlife Trafficking Through Uganda And
Cover: The carcass of an elephant killed by militarized poachers. Garamba National Park, DRC, April 2016. Photo: African Parks Deadly Profits Illegal Wildlife Trafficking through Uganda and South Sudan By Ledio Cakaj and Sasha Lezhnev July 2017 Executive Summary Countries that act as transit hubs for international wildlife trafficking are a critical, highly profitable part of the illegal wildlife smuggling supply chain, but are frequently overlooked. While considerable attention is paid to stopping illegal poaching at the chain’s origins in national parks and changing end-user demand (e.g., in China), countries that act as midpoints in the supply chain are critical to stopping global wildlife trafficking. They are needed way stations for traffickers who generate considerable profits, thereby driving the market for poaching. This is starting to change, as U.S., European, and some African policymakers increasingly recognize the problem, but more is needed to combat these key trafficking hubs. In East and Central Africa, South Sudan and Uganda act as critical waypoints for elephant tusks, pangolin scales, hippo teeth, and other wildlife, as field research done for this report reveals. Kenya and Tanzania are also key hubs but have received more attention. The wildlife going through Uganda and South Sudan is largely illegally poached at alarming rates from Garamba National Park in the Democratic Republic of Congo, South Sudan, points in West Africa, and to a lesser extent Uganda, as it makes its way mainly to East Asia. Worryingly, the elephant -

Global Impacts of the Illegal Wildlife Trade Global Impacts of the Illegal Wildlife Trade
Global Impacts of the Illegal Wildlife Trade Trade Global Impacts of the Illegal Wildlife Global Impacts of the Illegal Wildlife Trade The Costs of Crime, Insecurity and Institutional Erosion Katherine Lawson and Alex Vines Katherine Lawson and Alex Vines February 2014 Chatham House, 10 St James’s Square, London SW1Y 4LE T: +44 (0)20 7957 5700 E: [email protected] F: +44 (0)20 7957 5710 www.chathamhouse.org Charity Registration Number: 208223 Global Impacts of the Illegal Wildlife Trade The Costs of Crime, Insecurity and Institutional Erosion Katherine Lawson and Alex Vines February 2014 © The Royal Institute of International Affairs, 2014 Chatham House (The Royal Institute of International Affairs) is an independent body which promotes the rigorous study of international questions and does not express opinions of its own. The opinions expressed in this publication are the responsibility of the authors. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical including photocopying, recording or any information storage or retrieval system, without the prior written permission of the copyright holder. Please direct all enquiries to the publishers. Chatham House 10 St James’s Square London SW1Y 4LE T: +44 (0) 20 7957 5700 F: + 44 (0) 20 7957 5710 www.chathamhouse.org Charity Registration No. 208223 ISBN 978 1 78413 004 6 A catalogue record for this title is available from the British Library. Cover image: © US Fish and Wildlife Service. Six tonnes of ivory were crushed by the Obama administration in November 2013. Designed and typeset by Soapbox Communications Limited www.soapbox.co.uk Printed and bound in Great Britain by Latimer Trend and Co Ltd The material selected for the printing of this report is manufactured from 100% genuine de-inked post-consumer waste by an ISO 14001 certified mill and is Process Chlorine Free. -

On the Trail of the Perfect Wildlife Film Natural History Cameraman Graham Macfarlane on How the Varicam Lt Meets the Challenges of Shooting in the Wild
PROFESSIONAL CAMERA ON THE TRAIL OF THE PERFECT WILDLIFE FILM NATURAL HISTORY CAMERAMAN GRAHAM MACFARLANE ON HOW THE VARICAM LT MEETS THE CHALLENGES OF SHOOTING IN THE WILD Freelance cameraman Graham Macfarlane has Graham paired the camera with a Canon CN7 lens for the "It's a real headache to focus in 4K these days so I was been lucky enough to travel the world in the majority of the shoot, with the occasional addition of a CN20 spending a lot of time using it, and it was one of the first long lens, when working at more of a distance. things I liked - it's clear and very usable. It's the first pursuit of his passion for wildlife camera for a few years that I've thought about buying cinematography. From chimps to cheetahs, Filming primarily at 800 ISO, he was able to make use of the myself." VariCam LT's dual native 5000 ISO setting a handful of times, he's seen it all and put cameras through their such as at sunset. Graham has also put the VariCam LT through its paces in a paces. Now based in Japan, the Bristolian is forthcoming series following chimpanzees in the one of the BBC Natural History Unit's main Out on the Kenyan plains during the day, however, there was Cameroonian jungle. The choice to go with the VariCam came usually more than enough light. Two separate shoots saw the contributors and has worked on series such as about due to the darkened environment created by the thick crew spending a total of around eight weeks out on location. -

Unit 2 Copycat Animals
Unit 2 Copycat Animals In this unit, I will . • describe animal features. • describe how animals protect themselves. • talk about ways animals imitate others. • write a paragraph of classification. Check T for True and F for False. 1. This is a plant. T F 2. It is very soft. T F 3. It is very small. T F 4. It has sharp teeth. T F Allied cowrie, Papua New Guinea 20 21 11691_u02_ptg01_hr_020-035.indd 20-21 13/06/13 3:10 PM 1 Listen and read. TR: A10 2 Listen and repeat. TR: A11 Some animals can look like other animals or even like a plant! These copycats are trying to hide from or trick a hungry predator. They can look like another more dangerous animal or like another animal the predator doesn’t like to eat. spots a predator prey These butterflies are not the same species, but they resemble each This cheetah’s black spots act as camouflage. other. The top one tastes bad. The This way, the cheetah doesn’t frighten its prey other one copies its shape and when it’s time to hunt. colors, and tastes bad, too. 3 Work with a partner. What did you a stripe learn? Ask and answer. This colorful frog has stripes on its skin. How do some frogs show The bright colors tell they are poisonous? They have bright colors. hungry predators that the frog is poisonous. This insect is as green as a leaf. It imitates the characteristics of color and shape of leaves to help it hide from predators. -

2015 Southeast Alaska Discovery Center Spring Schedule 2015 Southeast Alaska Discovery Center Spring Schedule
2015 Southeast Alaska Discovery Center Spring Schedule 2015 Southeast Alaska Discovery Center Spring Schedule The Southeast Alaska Discovery Cen ter January 2, 2015 operated by the US Forest Service January 23, 2015 February 13, 2015 is excited to announce our Spring 2015 12:15 Film: Frozen Planet Ends of the Earth 12:30 Film: National Parks America’s Best Idea 12:30 Film: National Parks America’s Best winter events schedule. 1:15 Film: Theodore Roosevelt Idea Great Nature American Experience Going Home All programs are free and open to 2:30 Film: Salmon Running the Gaunt let 5:30 Film: America’s Deadly Volcano Katami 2:30 Film: Life on Fire The Surprise Salm on the public. 3:30 Film: The West Fight No More Forever 6:30 Film: The West The People 3:30 Film: The West Speck of Future 5:30 Film: Leave it to Beaver 5:30 Film: The Greely Expedition Schedule is subject to change. 7:00 Speaker: Paleolimnology Lake Harriet 7:00 Speaker: Ketchikan High School Oce an Additional events may be oered January 9, 2015 Hunt and Water Quality with Science Bowl Competition with Julie throughout the winter. Christopher Done r Landwehr Visit our website http://alaskacenters.gov/ 12:30 Film: John Muir in the New World January 30, 2015 February 20, 2015 ketchikan.cfm or request ema-il updates by 2:00 Film: Life on Fire: Volcanoes Doctors contacting [email protected] 3:00 Film: The West the People 12:30 Film: 60 Degrees Nort h 12:30 Film: The National Parks America’s Best 4:45 Film: Your Inner Fish 2:00 Film: Braving Alaska Idea Morning of Creation 5:30 Film: Becoming Human First Steps Education box check in/out, information 3:30 Film: The West Death Runs Riot 2:30 Film: The Greely Expedition 7:00 Speaker: A day in the Life of Ketchikan requests, eld trips and map sales will be 3:30 Film: The West Geography of Hope with Susan Hoyt 5:30 Film: Your Inner Monkey oered during our business hours: 7:00 Film: Tracing Roots with Dolores 5:45 Film: Great Migrations Born to Mo ve Fridays Noon to 8 p.m. -

Geography Super Curriculum Year 7
Geography Super Curriculum Year 7 Map Skills Extreme China Ecosystems Rivers Environments School library section 551, School library section 551 School library section 951 School library section School library section 912 Extreme Earth, Visual Travel Through China, 574.5/581 Planet Habitats, 551.48 Mapping Britain’s Mapping Britain’s Explorers 551.2 Come on a journey of Louise & Richard Spilsbury Landscapes, Rivers, by Landscapes, Coasts, by Geography Fact Files, discovery by Lynn Huggins- (581) Horrible Geography: Barbara Taylor (551.48) Barbara Taylor (551.4) Deserts by Anna Cooper (951) Chinese Bloomin’ Rainforest Geography Fact Files, Mapping Britain’s Claybourne (551.41) Focus, Changing China, by Rivers by Mandy Ross Landscapes, Rivers, by Horrible Geography - Marta Block (551.48) Horrible Barbara Taylor (551.48) Bloomin' Rainforests Geography - Raging Rivers Children’s Atlas (912) Harry (2001) (2000) Potter, (Marauder's Map) JRR Tolkien’s Lord of the Rings (map of Middle Earth) Master and commander Plant Earth – Deserts, Supersized Earth – Episode Ecosystems class clips, BBC BBC Human PlanetFriend (2003) Mountains, From Pole to 2 Bridge Building Mulan http://www.bbc.co.uk/ or foe? Lord of the rings (2001) Pole. (1998) education/ topics/ Supersized Earth, episode BBC Human Planet: Arctic ztgw2hv/ resources/1 3, Food, Fire and Water – Life in the deep freeze. BBC Human Planet – Jungles. (Water) Deserts – Life in the Planet Earth, Jungles Avatar Into the wild (2007) Planet furnace (2009) Madagascar (2005) Earth, Fresh Water Mountains – life in the air The history of maps. When, How to plants adapt to Choose one animal that is Research and create fact files Research about the past, why and how did the OS map living in threatened by China’s for 5 of the world’s main present and future plans begin? When and why did deserts/rainforests/pol ar development. -

Frozen Kingdom
Frozen Kingdom Welcome to the planet’s coldest lands… vast wilds, hostile territories, incredibly beautiful yet often deadly. Take shelter from the elements or fall prey to icy winds and deepest chill. Trek bravely and valiantly across treacherous terrain to the ends of the Earth, treading deep in snow or pulled by a team of mighty sled dogs. Be alert, for magnificent mammals roam these lands, sometimes hungry or fresh for a fight. Perhaps a hungry polar bear or an arctic fox; hunting rodents and swift as the wind. Key facts Key Vocabulary Fungi-plants that have no flowers, leaves, or green colouring, such as a There are no land-dwelling mammals in the Antarctic although mushroom or a toadstool. Other types of fungus such as mould are extremely small and look like a fine powder. the Arctic has many land-dwelling mammals include musk ox, reindeer, caribou, fox, hare, wolf, lemming and bears. Mushroom-fungi that you can eat Toadstool-a fungus that you cannot eat because it is poisonous The seas of the Antarctic and the Arctic both have marine Fermentation-a chemical change that happens in vegetable and animal mammals. substances. Above the Arctic Circle, there is all-day sunshine in the summer Microbe-a very small living thing, which you can only see if you use for at least one day a year (and there’s a full 24 hours of a microscope. darkness on at least one day too!) Bacteria-very small organisms. Some bacteria can cause disease. Climate change is the polar bears’ biggest threat. -

The South Africa – Viet Nam Rhino Horn Trade Nexus
Executive Summary of The South Africa – Viet Nam Rhino Horn Trade Nexus: A deadly combination of institutional lapses, corrupt wildlife industry professionals and Asian crime syndicates By Tom Milliken and Jo Shaw with contributions from Richard H. Emslie, Russell D. Taylor and Chris Turton A TRAFFIC REPORT THE SITUATION AT THE SOURCE SOUTH AFRICA outh Africa, a vast country spanning the bot- tom of the African continent, unquestionably has the world’s most successful conservation record for rhinos. In 2011, this country alone Sconserved 83% of Africa’s rhinos and nearly three-quarters of all wild rhinos worldwide. As one of the most biologically diverse nations glob- ally, South Africa has long promoted biodiversity con- servation through the sustainable use of natural resources. In fact, the country’s constitution enshrines these principles, calling for: “a prosperous, environ- mentally conscious nation, whose people are in har- monious coexistence with the natural environment, and which derives lasting benefits from the conserva- tion and sustainable use of its rich biological diversity”. With such an enabling environment, it is not sur- prising that, since the 1960s, there has been a marked shift to wildlife-based land-use amongst private land- owners, and today game ranches in South Africa cover an area nearly three times the collective size of all national and provincial protected areas on State land. Wildlife in general, but rhinos in particular, have ben- efitted tremendously from these visionary natural resource policies. But the country’s superlative conser- vation record of more than a century is under threat. Ironically, the fate of South Africa’s rhinos is now inextricably linked with market forces in Viet Nam, a country that recently saw its own rhino population slip into ignominious extinction. -

New Exclusive Animal Experiences Now Available
NEW EXCLUSIVE ANIMAL EXPERIENCES NOW AVAILABLE Visit the Zoo before the crowds arrive, feed an unusual hero, groom a goat, dive with sharks or go behind-the-scenes of the Pacific Seas Aquarium FOR IMMEDIATE RELEASE: Oct. 5, 2020 TACOMA, Wash.—Point Defiance Zoo & Aquarium is expanding its Zoo for You exclusive animal experiences with two new premier adventures. In addition to grooming goats, diving with sharks and a behind-the-scenes tour of the Pacific Seas Aquarium, households can now book a private tour of the Zoo before it opens or get up close and personal with the Zoo’s own superheroes- HeroRATs! These experiences make for excellent family bonding, birthday or holiday gifts, and are both a safe and fun way to get out of the house during uncertain times. Wild Zoo Tour Mornings at the Zoo are a special time: you can see the sunrise over the sound and in the quiet hours before guests arrive, you may hear the siamangs singing (listen for their duets of booms, barks and hoots), the walruses whistling and the wolves howling. The keepers are busy feeding breakfast to the animals and transitioning them from their overnight bedrooms to their outdoor habitats. Now, for the first time ever, guests have a chance to be there and enjoy those intimate early morning hours at the Zoo. Over 1.5 hours, visit selected areas of the zoo with a knowledgeable guide, without the crowds. This unique experience culminates with a special one-on-one surprise animal encounter at the Wild Wonders Outdoor Theater.