2901121 Safer Hospitals, Safer Wards
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sprouting Pinenut September 2018
1 Numa News Sprouting Pinenut September 2018 Fallon Paiute Shoshone Tribal Newsletter www.fpst.org Volume 12 Issue 9 September 2018 1 2 Laura Ijames Tribal Secretary Report [email protected] Our department participated in the Back to School Night which was held at the Fallon Convention Center. Jolene Thomas, Secretary’s Assistant, invested her time as a volunteer for the event where many backpacks and supplies given out for the new school year. It was good to see the whole community come out and support our youth. I would like to thank the FPST Co-Ed Softball team for donating their winning plaque to the tribe. Since the tribe donated to the team, they named the team after the tribe. I am glad to see that tribal donations are enriching our young adults in a positive way. If you would like to see the plaque and picture it will be in the lobby at the administration building. A successful antelope hunt The Labor Day weekend is coming soon and I hope everyone has a safe holiday weekend. Committee Openings: Land and Water Resources– 2 vacancies Senior Committee– 1 vacancies Election Committee Alternate-1vacancy Any interested Tribal Member may submit a Committee Appointment form to the FBC Secretary 3 1 4 5 1 6 7 1 8 FPST CO-ED SLOWPITCH CHAMPIONS Congratulations to the FPST Co-Ed Softball Team on their 1st place win in the Oasis Adult Softball Association League on Tuesday, August 8, 2018. The league winners received a 1st place plague as they showed why they are the top team in the league, with a big contin- gent of them tribal members. -

Vista Comparison to the Commercial Electronic Health Record Marketplace Final Report
VistA Comparison to the Commercial Electronic Health Record Marketplace Final Report February 4, 2011 Prepared for: U.S. Department of Veterans Affairs Martin Geffen Vice President Gartner Consulting [email protected] GARTNER CONSULTING This presentation, including any supporting materials, is owned by Gartner, Inc. and/or its affiliates and is for the sole use of the intended Gartner audience or other authorized recipients. This presentation may contain information that is confidential, proprietary or otherwise legally protected, and it may not be further copied, distributed or publicly displayed without the express written permission of Gartner, Inc. or its affiliates. © 2010 Gartner, Inc. and/or its affiliates. All rights reserved. Table of Contents ■ Executive Summary ■ Project Objectives and Approach ■ Electronic Health Record Systems Marketplace ■ VistA Overall Findings ■ VistA Capability Assessment ■ Appendices © 2011 Gartner, Inc. and/or its affiliates. All rights reserved. Gartner is a registered trademark of Gartner, Inc. or its affiliates. 1 Executive Summary © 2011 Gartner, Inc. and/or its affiliates. All rights reserved. Gartner is a registered trademark of Gartner, Inc. or its affiliates. 2 Objective and Approach ■ Project Objective – The Department of Veterans Affairs (VA) engaged Gartner to develop a fact-based assessment of how VistA capabilities compare to those that are found in leading commercial off-the-shelf (COTS) Electronic Health Record (EHR) products. ■ Approach – Gartner applied an evaluation framework which is based on Gartner research, Gartner‘s definition of an EHR and methodologies (e.g., Magic Quadrant, Generations Model, Hype Cycle) to compare VistA clinical functionality to that of the EHR COTS products. – The evaluation framework compared VistA capabilities to those of COTS products in three major categories: • Core Clinical Capabilities • Support for Key Care Venues • Support for select Stakeholders © 2011 Gartner, Inc. -

AC Group's 2007 Annual Report the Digital Medical Office of the Future
AC Group’s 2007 Annual Report The Digital Medical Office of the Future Computer Systems for the Physician’s Office May 2007 Comprehensive Report on: Overview of Physician adoption The Six Levels of Physician IT Maturity Practice Management Marketplace Secured Internet Document Image Management PDA and Mobile Healthcare Electronic Medical Record Functionality Electronic Medical Health Marketplace Regional Healthcare Information Organizations Mark R. Anderson, CPHIMS, FHIMSS Healthcare IT Futurist AC Group, Inc. (v) 281-413-5572 [email protected] www.acgroup.org AC Group’s 2007 Annual Report The Digital Medical Office of the Future Computer Systems for the Physician’s Office More about the Author Mr. Anderson is one of the nation's premier IT research futurists dedicated to health care. He is one of the leading national speakers on healthcare and physician practices and has spoken at more than 350 conferences and meetings since 2000. He has spent the last 30+ years focusing on Healthcare – not just technology questions, but strategic, policy, and organizational considerations. He tracks industry trends, conducts member surveys and case studies, assesses best practices, and performs benchmarking studies. Besides serving at the CEO of AC Group, Mr. Anderson served as the interim CIO for the Taconic IPA in 2004-05 (a 500 practice, 2,300+ physician IPA located in upper New York). Prior to joining AC Group, Inc. in February of 2000, Mr. Anderson was the worldwide head and VP of healthcare for META Group, Inc., the Chief Information Officer (CIO) with West Tennessee Healthcare, the Corporate CIO for the Sisters of Charity of Nazareth Health System, the Corporate Internal IT Consultant with the Sisters of Providence (SOP) Hospitals, and the Executive Director for Management Services for Denver Health and Hospitals and Harris County Hospital District. -

Leicester, Leicestershire and Rutland (LLR) Local Digital Roadmap 2016 - 2021 Contents
Leicester, Leicestershire and Rutland (LLR) Local Digital Roadmap 2016 - 2021 Contents Foreword for Local Digital Roadmap 2 5. Capabilities 38 5.1 Paper free at Point of Care groups 1. Introduction 4 of capabilities 38 1.1 Our Journey in Delivering the 5.1.1 Records, assessments and plans 38 Five Year Forward View and Personalised 5.1.2 Transfers of care 41 Health and Care 2020 4 5.1.3 Orders and results management 43 1.2 Overview of Organisations Covered 6 5.1.4 Medicines management and optimisation 43 1.3 Sustainability and Transformation Plan 5.1.5 Decision support 45 (STP) Alignment 6 5.1.6 Remote care 46 1.3.1 Better Care Together (BCT) 7 5.1.7 Asset and resource optimisation 49 1.4 Leicester, Leicestershire and Rutland (LLR) 5.2 16/17-17/18 Universal capabilities 54 Context 8 5.3 Capabilities Delivery Plan 55 2. A vision for digitally-enabled 6. Information Sharing 56 transformation 19 6.1 Information Sharing Strategy 56 6.2 Information Governance 56 6.3 Interoperability Strategy 57 3. Baseline Position 20 3.1 Current Technology Landscape 20 7. Infrastructure 58 3.1.1 Data Sharing 20 3.1.2 Patient Access 21 3.1.3 Electronic Prescriptions 21 8. Minimising risks arising from 3.1.4 Electronic Clinical Correspondence 21 technology 63 3.1.5 Business Intelligence 21 3.1.6 System Access 22 9. Timescales and Delivery of the 3.1.7 Pathways 22 Local Digital Roadmap 64 3.1.8 Patient Focused Apps 22 2016/17 64 3.2 Rate limiting factors 23 2017/18 66 2018/19 68 4. -

Semi-Annual Market Review
Semi-Annual Market Review HEALTH IT & HEALTH INFORMATION SERVICES JULY 2019 www.hgp.com TABLE OF CONTENTS 1 Health IT Executive Summary 3 2 Health IT Market Trends 6 3 HIT M&A (Including Buyout) 9 4 Health IT Capital Raises (Non-Buyout) 14 5 Healthcare Capital Markets 15 6 Macroeconomics 19 7 Health IT Headlines 21 8 About Healthcare Growth Partners 24 9 HGP Transaction Experience 25 10 Appendix A – M&A Highlights 28 11 Appendix B – Buyout Highlights 31 12 Appendix C – Investment Highlights 34 Copyright© 2019 Healthcare Growth Partners 2 HEALTH IT EXECUTIVE SUMMARY 1 An Accumulating Backlog of Disciplined Sellers Let’s chat about fireside chats. The term first used to describe a series of evening radio addresses given by U.S. President Franklin D. Roosevelt during the Great Depression and World War II is now investment banker speak for “soft launches” of sell-side and capital raise transactions. Every company has a price, and given a market of healthy valuations, more companies are testing the waters to find out whether they can achieve that price. That process now looks a little more informal, or how you might envision a fireside chat. Price (or valuation) discovery for a company can range from a single conversation with an individual buyer to a full-blown auction with hundreds of buyers and everything in between, including a fireside chat. Given the increasing share of informal conversations, the reality is that more companies are for sale than meets the eye. While the healthy valuations publicized and press-released are encouraging more and more companies to price shop, there is a simultaneous statistical phenomenon in perceived valuations that often goes unmentioned: survivorship bias. -
Private Equity Buyouts in Healthcare: Who Wins, Who Loses? Eileen Appelbaum and Rosemary Batt Working Paper No
Private Equity Buyouts in Healthcare: Who Wins, Who Loses? Eileen Appelbaum* and Rosemary Batt† Working Paper No. 118 March 15, 2020 ABSTRACT Private equity firms have become major players in the healthcare industry. How has this happened and what are the results? What is private equity’s ‘value proposition’ to the industry and to the American people -- at a time when healthcare is under constant pressure to cut costs and prices? How can PE firms use their classic leveraged buyout model to ‘save healthcare’ while delivering ‘outsized returns’ to investors? In this paper, we bring together a wide range of sources and empirical evidence to answer these questions. Given the complexity of the sector, we focus on four segments where private equity firms have been particularly active: hospitals, outpatient care (urgent care and ambulatory surgery centers), physician staffing and emergency * Co-Director and Senior Economist, Center for Economic and Policy Research. [email protected] † Alice H. Cook Professor of Women and Work, HR Studies and Intl. & Comparative Labor ILR School, Cornell University. [email protected]. We thank Andrea Beaty, Aimee La France, and Kellie Franzblau for able research assistance. room services (surprise medical billing), and revenue cycle management (medical debt collecting). In each of these segments, private equity has taken the lead in consolidating small providers, loading them with debt, and rolling them up into large powerhouses with substantial market power before exiting with handsome returns. https://doi.org/10.36687/inetwp118 JEL Codes: I11 G23 G34 Keywords: Private Equity, Leveraged Buyouts, health care industry, financial engineering, surprise medical billing revenue cycle management, urgent care, ambulatory care. -
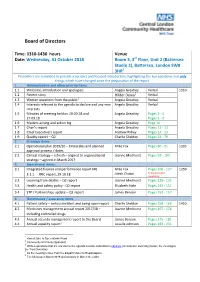
Board of Directors
Board of Directors Time: 1310-1430 hours Venue Date: Wednesday, 31 October 2018 Room 3, 3rd Floor, Unit 2 (Battersea Studio 2), Battersea, London SW8 3HR1 Presenters are reminded to provide a succinct and focused introduction, highlighting the key questions and only things which have changed since the preparation of the report 1 Administrative and other priority items 1.1 Welcome, introduction and apologies: Angela Greatley Verbal 1310 2 1.2 Patient story Hilder Dewa Verbal 1.3 Written questions from the public3 Angela Greatley Verbal 1.4 Interests relevant to the agenda to declare and any new Angela Greatley Verbal interests 1.5 Minutes of meeting held on 20.09.18 and Angela Greatley Pages 3 - 4 27.09.18 Pages 5 - 9 1.6 Matters arising and action log Angela Greatley Page 10 1.7 Chair’s report Angela Greatley Pages 11 - 13 1.8 Chief Executive’s report Andrew Ridley Pages 14 - 23 1.9 Quality report – Q2 Charlie Sheldon Pages 24 - 79 2 Strategic items 2.1 Operational plan 2019/20 – timescales and planned Mike Fox Pages 80 - 91 1335 approval process / dates 2.2 Clinical strategy – refresh – aligned to organisational Joanne Medhurst Pages 92 - 105 strategy – agreed in March 2017 3 Operational items 3.1 Integrated finance and performance report M6 Mike Fox Pages 106 - 127 1350 Jitesh Chotai To be provided 3.1.1 FRIC report, 29.10.18 separately 4 3.2 Learning from deaths – Q2 report Joanne Medhurst Pages 128 - 131 3.3 Health and safety policy - Q2 report Elizabeth Hale Pages 132 - 151 3.4 STP / Partnerships update – Q2 report James Benson Pages -
To See 2014 Health Policy Survey Results
2014 HEALTH POLICY SURVEY RESULTS Western Section American Urological Association Jeffrey M. Frankel, M.D. Chairman, Health Policy Committee An educational supplement to the WSAUA Health Policy Forum, October 26, 2014 – Grand Wailea Hotel, Maui, Hawaii 2014 Health Policy Committee Chairman: Jeffrey M. Frankel, M.D. Vice-Chairman: Eugene Rhee, M.D., MBA Robert G. Carlile, M.D., Hawaii District 1 Jeffrey M. Frankel, M.D., Washington District 2 Brian S. Shaffer, M.D., Portland District 3 Joseph R. Kuntze, M.D., Fresno District 4 Demetrios Simopoulas M.D., Sacramento District 5 Jeremy Shelton, M.D., Los Angeles District 6 Ithaar Derweesh, M.D., San Diego District 7 Micheal Darson, M.D., Scottsdale District 8 Lane Childs, M.D., Salt Lake City District 9 Aaron Spitz, M.D., Orange County District 10 Advisors: • Jeffrey E. Kaufman, MD • Amani Abou Zam-zam, MBA Copyright2014 by the Western Section American Urological Association, Inc. All rights reserved. Published by the Western Section American Urological Association, Inc. 1950 Old Tustin Avenue, Santa Ana, CA 92705. Call 714-550-9155 to order copies. Geographical Districts of the Western Section of the American Urological Association, Inc. District 1: Northwest Canadian Provinces, Alaska, Hawaii, Philippine Islands and Pacific Island Possessions of the U.S.A. District 2: Washington District 3: Oregon District 4: Northern California including Alameda and Contra Costa Counties District 5: San Francisco, San Mateo, and Santa Clara Counties and Central California District 6: Los Angeles County District -

Case Studies of Vista Implementation— United States and International
39251_CH09_223_284 11/27/06 5:26 PM Page 223 CHAPTER 9 Case Studies of VistA Implementation— United States and International “VHA’s integrated health information system, including its framework for using performance measures to improve quality, is considered one of the best in the nation.” Institute of Medicine (IOM) Report, “Leadership by Example: Coordinating Government Roles in Improving Health Care Quality, 2002” Introduction The U.S. Department of Veterans Affairs (VA) has developed and imple- mented a comprehensive health information system and EHR system known as VistA, which was built from the ground up with a clinical focus. Many of the commercial off-the-shelf (COTS) health information systems in the private sector today were designed from a financial perspective and now are being reengineered to address medical and clinical informatics requirements. The VistA system is a proven product and can be readily adapted for use in acute care, ambulatory, and long-term care settings. It has been used in public and private healthcare provider organizations across the United States and in a number of international settings. 223 39251_CH09_223_284 11/27/06 5:26 PM Page 224 224 CASE STUDIES OF VISTA IMPLEMENTATION—UNITED STATES AND INTERNATIONAL Table 9-1 VistA Software Modules VistA Software Packages Pharmacy: Inpatient Medications Health Data Systems Pharmacy: Inpatient Medications— Automated Medical Information Exchange Intravenous (IV) (AMIE) Pharmacy: Inpatient Medications— Incident Reporting Unit Dose (UD) Lexicon Utility Pharmacy: -

The World's Leading AI in Medicine Summit
The world’s leading AI in medicine summit Wednesday 5th February 2020 London, UK http://www.intelligenthealth.ai/ The mission? Intelligent Health, in partnership with NHSX, will bring the global AI and health community to London in February 2020 for a one-day event to advance discussions on how to apply AI and drive technological collaboration in healthcare. 800+ delegates will join industry leading global speakers for an in-depth look at AI within the UK health market, how it can be used to prevent and solve some of the world’s greatest healthcare problems, improve the health of the human race and set the UK AI agenda in healthcare for 2020 and beyond. What’s on? Jam-packed day of health tech goodness! Practical, real-world AI use cases, announcements from tech giants, hear from health tech transformers of tomorrow and a showcase of innovation, followed by 10 collaborative hands-on sessions tackling live digital health challenges. Be ready to think like a physician and code like a developer. Wednesday 5th February 2020 07:30 REGISTRATION Session One 09:00 – 11:00 09:00 WELCOME Inspired Minds Denise Tack, Strategy Director - Health, Inspired Minds WELCOME NHSX Tara Donnelly, CDIO, NHSX WELCOME and chairperson’s opening remarks Sameena Ali-Khan, Television Presenter, ITV 09:20 HEADLINER Leading digital change, interoperability and innovation – how the NHS will work more effectively with larger tech firms and digital health innovators Tara Donnelly, CDIO, NHSX 09:45 HEADLINER Maximising our digital infrastructure for a 21st century workforce Frank Hester, Founder and CEO, The Phoenix Partnership 10:10 HEADLINER Inside Pandora's Black Box: Understanding decision-making in diagnostic AI and its implications for clinician skills Dr. -

Management Stakeholders
Hyperglycaemia in acute coronary syndromes: management Stakeholders 15 Healthcare 2gether NHS Foundation Trust 3M Health Care UK 4Children 5 Boroughs Partnership NHS Foundation Trust A.Menarini Pharma U.K. S.R.L. Abbott Diabetes Care Abbott Diagnostics Division Abbott Diagnostics Division Abbott Laboratories Abbott Vascular Devices Abbott Vascular Devices AbbVie AbbVie Abertawe Bro Morgannwg University NHS Trust Achieving for Children Action Heart Action on Addiction Action on Hearing Loss Action on Smoking & Health Action on Smoking and Health Addaction Addenbrookes Hospital Addiction Today ADFAM Adults Strategy and Commissioning Unit Advisory Committee for Community Dentistry Advisory Council on the Misuse of Drugs Afiya Trust African Health Policy Network Aintree University Hospital NHS Foundation Trust Alcohol and Drug service Alcohol Focus Scotland Alcohol Use Disorders: Clinical Management Guideline Development Group Alcoholics Anonymous Alder Hey Children's NHS Foundation Trust Alere Alere Alere International Alere Ltd Alere Ltd Alkermes Inc All Party Parliamentary Group on Vascular Disease Allergan Ltd UK Alliance Boots plc Allocate Software PLC Alpha Medical American Medical Systems Inc. American Medical Systems Inc. American Medical Systems UK Ltd AMORE health Ltd AMORE health Ltd AMORE Studies Group AMORE Studies Group Aneurin Bevan University Health Board anglia community leisure Anglia University Anglian Community Enterprise Ark Therapeutics Ltd Arrhythmia Alliance Arrowe Park Hospital Assocation of NHS Occupational Physicians -

Organization Name Credentials Sent Date 1 REX INC 7/6/2016 1ST CHOICE MEDICAL BILLING 6/22/2016 1ST PRIORITY BILLING SOLUTIONS 6
The organization names listed below were pulled directly from the EDISS Connect registration system. If you are unaware of how your organization name may be listed, you will want to access your EDISS Connect account. Organization Name Credentials Sent Date 1 REX INC 7/6/2016 1ST CHOICE MEDICAL BILLING 6/22/2016 1ST PRIORITY BILLING SOLUTIONS 6/22/2016 808 MEDICAL BILLING LLC 6/22/2016 A & L BILLING SERVICE 6/22/2016 A PLUS MEDICAL BILLING, LLC 6/22/2016 A TOUCH OF NORSK CHIRO 8/3/2016 A&M BILLING AND CONSULTING 6/22/2016 A. B. CRISPINO & CO. INC. 8/3/2016 AAA PROFESSIONAL MEDICAL BILLING INC 6/22/2016 ABDULLAH SURGICAL CENTER LLC 8/3/2016 ABHM 8/3/2016 ABILITY 7/6/2016 ABLAZE MEDICAL BILLING 6/22/2016 ACCUPRO MEDICAL SERVICES 6/22/2016 ACCURATE MEDICAL BILLING PROFESSIONALS 6/22/2016 ACE MEDICAL PROFESSI 6/22/2016 ACTION BILLING SERVICES 6/22/2016 ACTION MEDICAL SERVICE, INC. 8/3/2016 ADA BOI INC 8/3/2016 ADAPS, INC. 7/6/2016 ADELANTE HEALTHCARE 8/3/2016 ADMINISTEP, LLC 7/6/2016 ADSLLC 6/22/2016 ADV DERMATOLOGY & SKIN SURG 8/3/2016 ADVANCED BEHAVIORAL HEALTH BILLING LLC 6/22/2016 ADVANCED BILLING AND 6/22/2016 ADVANCED BILLING SER 5/25/2016 ADVANCED BILLING SERVICES 6/22/2016 ADVANCED EYECARE 8/3/2016 ADVANCED PACIFIC MED 6/22/2016 ADVANCED PRACTICE BILLING LLC 6/22/2016 ADVANCEDMD SOFTWARE INC 6/22/2016 ADVENTIST HEALTH SYSTEMS WEST 6/22/2016 ADVENTIST HEALTH SYSTEMS WEST 6/22/2016 AERO MED CLAIMS 6/22/2016 AFFILIATED PROFESSIONAL SERVICES, INC.