A Method for Estimating Intracellular Sodium Concentration And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Ideal-Gas Mixtures and Real-Gas Mixtures
Thermodynamics: An Engineering Approach, 6th Edition Yunus A. Cengel, Michael A. Boles McGraw-Hill, 2008 Chapter 13 GAS MIXTURES Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Objectives • Develop rules for determining nonreacting gas mixture properties from knowledge of mixture composition and the properties of the individual components. • Define the quantities used to describe the composition of a mixture, such as mass fraction, mole fraction, and volume fraction. • Apply the rules for determining mixture properties to ideal-gas mixtures and real-gas mixtures. • Predict the P-v-T behavior of gas mixtures based on Dalton’s law of additive pressures and Amagat’s law of additive volumes. • Perform energy and exergy analysis of mixing processes. 2 COMPOSITION OF A GAS MIXTURE: MASS AND MOLE FRACTIONS To determine the properties of a mixture, we need to know the composition of the mixture as well as the properties of the individual components. There are two ways to describe the composition of a mixture: Molar analysis: specifying the number of moles of each component Gravimetric analysis: specifying the mass of each component The mass of a mixture is equal to the sum of the masses of its components. Mass fraction Mole The number of moles of a nonreacting mixture fraction is equal to the sum of the number of moles of its components. 3 Apparent (or average) molar mass The sum of the mass and mole fractions of a mixture is equal to 1. Gas constant The molar mass of a mixture Mass and mole fractions of a mixture are related by The sum of the mole fractions of a mixture is equal to 1. -

An Empirical Model Predicting the Viscosity of Highly Concentrated
Rheol Acta &2001) 40: 434±440 Ó Springer-Verlag 2001 ORIGINAL CONTRIBUTION Burkhardt Dames An empirical model predicting the viscosity Bradley Ron Morrison Norbert Willenbacher of highly concentrated, bimodal dispersions with colloidal interactions Abstract The relationship between the particles. Starting from a limiting Received: 7 June 2000 Accepted: 12 February 2001 particle size distribution and viscos- value of 2 for non-interacting either ity of concentrated dispersions is of colloidal or non-colloidal particles, great industrial importance, since it e generally increases strongly with is the key to get high solids disper- decreasing particle size. For a given sions or suspensions. The problem is particle system it then can be treated here experimentally as well expressed as a function of the num- as theoretically for the special case ber average particle diameter. As a of strongly interacting colloidal consequence, the viscosity of bimo- particles. An empirical model based dal dispersions varies not only with on a generalized Quemada equation the size ratio of large to small ~ / Àe g g 1 À / is used to describe particles, but also depends on the g as a functionmax of volume fraction absolute particle size going through for mono- as well as multimodal a minimum as the size ratio increas- dispersions. The pre-factor g~ ac- es. Furthermore, the well-known counts for the shear rate dependence viscosity minimum for bimodal dis- of g and does not aect the shape of persions with volumetric mixing the g vs / curves. It is shown here ratios of around 30/70 of small to for the ®rst time that colloidal large particles is shown to vanish if interactions do not show up in the colloidal interactions contribute maximum packing parameter and signi®cantly. -
Colloidal Suspensions
Chapter 9 Colloidal suspensions 9.1 Introduction So far we have discussed the motion of one single Brownian particle in a surrounding fluid and eventually in an extaernal potential. There are many practical applications of colloidal suspensions where several interacting Brownian particles are dissolved in a fluid. Colloid science has a long history startying with the observations by Robert Brown in 1828. The colloidal state was identified by Thomas Graham in 1861. In the first decade of last century studies of colloids played a central role in the development of statistical physics. The experiments of Perrin 1910, combined with Einstein's theory of Brownian motion from 1905, not only provided a determination of Avogadro's number but also laid to rest remaining doubts about the molecular composition of matter. An important event in the development of a quantitative description of colloidal systems was the derivation of effective pair potentials of charged colloidal particles. Much subsequent work, largely in the domain of chemistry, dealt with the stability of charged colloids and their aggregation under the influence of van der Waals attractions when the Coulombic repulsion is screened strongly by the addition of electrolyte. Synthetic colloidal spheres were first made in the 1940's. In the last twenty years the availability of several such reasonably well characterised "model" colloidal systems has attracted physicists to the field once more. The study, both theoretical and experimental, of the structure and dynamics of colloidal suspensions is now a vigorous and growing subject which spans chemistry, chemical engineering and physics. A colloidal dispersion is a heterogeneous system in which particles of solid or droplets of liquid are dispersed in a liquid medium. -

Lecture 3. the Basic Properties of the Natural Atmosphere 1. Composition
Lecture 3. The basic properties of the natural atmosphere Objectives: 1. Composition of air. 2. Pressure. 3. Temperature. 4. Density. 5. Concentration. Mole. Mixing ratio. 6. Gas laws. 7. Dry air and moist air. Readings: Turco: p.11-27, 38-43, 366-367, 490-492; Brimblecombe: p. 1-5 1. Composition of air. The word atmosphere derives from the Greek atmo (vapor) and spherios (sphere). The Earth’s atmosphere is a mixture of gases that we call air. Air usually contains a number of small particles (atmospheric aerosols), clouds of condensed water, and ice cloud. NOTE : The atmosphere is a thin veil of gases; if our planet were the size of an apple, its atmosphere would be thick as the apple peel. Some 80% of the mass of the atmosphere is within 10 km of the surface of the Earth, which has a diameter of about 12,742 km. The Earth’s atmosphere as a mixture of gases is characterized by pressure, temperature, and density which vary with altitude (will be discussed in Lecture 4). The atmosphere below about 100 km is called Homosphere. This part of the atmosphere consists of uniform mixtures of gases as illustrated in Table 3.1. 1 Table 3.1. The composition of air. Gases Fraction of air Constant gases Nitrogen, N2 78.08% Oxygen, O2 20.95% Argon, Ar 0.93% Neon, Ne 0.0018% Helium, He 0.0005% Krypton, Kr 0.00011% Xenon, Xe 0.000009% Variable gases Water vapor, H2O 4.0% (maximum, in the tropics) 0.00001% (minimum, at the South Pole) Carbon dioxide, CO2 0.0365% (increasing ~0.4% per year) Methane, CH4 ~0.00018% (increases due to agriculture) Hydrogen, H2 ~0.00006% Nitrous oxide, N2O ~0.00003% Carbon monoxide, CO ~0.000009% Ozone, O3 ~0.000001% - 0.0004% Fluorocarbon 12, CF2Cl2 ~0.00000005% Other gases 1% Oxygen 21% Nitrogen 78% 2 • Some gases in Table 3.1 are called constant gases because the ratio of the number of molecules for each gas and the total number of molecules of air do not change substantially from time to time or place to place. -

X-Nuclei MRI on a 7T MAGNETOM Terra: Initial Experiences
MAGNETOM Flash (76) 1/2020 Neurology · Research X-Nuclei MRI on a 7T MAGNETOM Terra: Initial Experiences Tobias Wilferth1; Lena V. Gast1,2; Sebastian Lachner1; Nicolas G. R. Behl3; Manuel Schmidt4; Arnd Dörfler4; Michael Uder1; Armin M. Nagel1,2,5 1 Institute of Radiology, University Hospital Erlangen, Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), Erlangen, Germany 2Institute of Medical Physics, Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), Erlangen, Germany 3Siemens Healthcare GmbH, Erlangen, Germany 4Department of Neuroradiology, University Hospital Erlangen, Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), Erlangen, Germany 5Division of Medical Physics in Radiology, German Cancer Research Center (DKFZ), Heidelberg, Germany Introduction However, X-nuclei imaging is challenging for several rea- sons. First of all, the signal-to-noise ratio (SNR) is several Ions such as sodium (Na+), potassium (K+) and chlorine (Cl-) orders of magnitude lower compared to proton (1H) MRI. play a vital role in many cellular processes. Healthy tissue In most situations relevant for human imaging, noise is contains very little extracellular K+ ([K+] = 2.5–3.5 mM) e dominated by the sample. And for low frequencies, which but a large amount of intracellular K+ ([K+] = 140 mM). i is usually the case for X-nuclei MRI, a linear noise model The Na+ gradient is reversed and a little less pronounced can be assumed. In this case, the SNR depends on the ([Na+] = 10–15 mM; [Na+] = 145 mM). Cl- is the most i e concentration c, the magnetic spin moment I and the gyro- abundant anion in the human body. magnetic ratio γ of the nucleus as given in Equation 1 [17]: Cellular exchange processes, such as the Na+/K+-ATPase pump [1] maintain chemical and electrical gradients across the cell membrane – essential for regulating cell volume, Equation 1 energy production and consumption, as well as excitation SNR ∝ c ∙ I ( I + 1 ) ∙ γ2 of muscle or neuronal cells. -

Distribution of Brain Sodium Long and Short Relaxation Times And
Distribution of brain sodium long and short relaxation times and concentrations: a multi-echo ultra-high field 23Na MRI study Ben Ridley, Armin Nagel, Mark Bydder, Adil Maarouf, Jan-Patrick Stellmann, Soraya Gherib, Jérémy Verneuil, Patrick Viout, Maxime Guye, Jean-Philippe Ranjeva, et al. To cite this version: Ben Ridley, Armin Nagel, Mark Bydder, Adil Maarouf, Jan-Patrick Stellmann, et al.. Distribution of brain sodium long and short relaxation times and concentrations: a multi-echo ultra-high field 23Na MRI study. Scientific Reports, Nature Publishing Group, 2018, 8 (1), 10.1038/s41598-018-22711-0. hal-02065574 HAL Id: hal-02065574 https://hal-amu.archives-ouvertes.fr/hal-02065574 Submitted on 12 Mar 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Distributed under a Creative Commons Attribution| 4.0 International License www.nature.com/scientificreports OPEN Distribution of brain sodium long and short relaxation times and concentrations: a multi-echo ultra- Received: 22 November 2017 23 Accepted: 23 February 2018 high feld Na MRI study Published: xx xx xxxx Ben Ridley1,2, Armin M. Nagel3,4, Mark Bydder1,2, Adil Maarouf1,2, Jan-Patrick Stellmann1,2, Soraya Gherib1,2, Jeremy Verneuil1,2, Patrick Viout1,2, Maxime Guye1,2, Jean-Philippe Ranjeva 1,2 & Wafaa Zaaraoui1,2 Sodium (23Na) MRI profers the possibility of novel information for neurological research but also particular challenges. -

Gp-Cpc-01 Units – Composition – Basic Ideas
GP-CPC-01 UNITS – BASIC IDEAS – COMPOSITION 11-06-2020 Prof.G.Prabhakar Chem Engg, SVU GP-CPC-01 UNITS – CONVERSION (1) ➢ A two term system is followed. A base unit is chosen and the number of base units that represent the quantity is added ahead of the base unit. Number Base unit Eg : 2 kg, 4 meters , 60 seconds ➢ Manipulations Possible : • If the nature & base unit are the same, direct addition / subtraction is permitted 2 m + 4 m = 6m ; 5 kg – 2.5 kg = 2.5 kg • If the nature is the same but the base unit is different , say, 1 m + 10 c m both m and the cm are length units but do not represent identical quantity, Equivalence considered 2 options are available. 1 m is equivalent to 100 cm So, 100 cm + 10 cm = 110 cm 0.01 m is equivalent to 1 cm 1 m + 10 (0.01) m = 1. 1 m • If the nature of the quantity is different, addition / subtraction is NOT possible. Factors used to check equivalence are known as Conversion Factors. GP-CPC-01 UNITS – CONVERSION (2) • For multiplication / division, there are no such restrictions. They give rise to a set called derived units Even if there is divergence in the nature, multiplication / division can be carried out. Eg : Velocity ( length divided by time ) Mass flow rate (Mass divided by time) Mass Flux ( Mass divided by area (Length 2) – time). Force (Mass * Acceleration = Mass * Length / time 2) In derived units, each unit is to be individually converted to suit the requirement Density = 500 kg / m3 . -

Solutions Mole Fraction of Component a = Xa Mass Fraction of Component a = Ma Volume Fraction of Component a = Φa Typically We
Solutions Mole fraction of component A = xA Mass Fraction of component A = mA Volume Fraction of component A = fA Typically we make a binary blend, A + B, with mass fraction, m A, and want volume fraction, fA, or mole fraction , xA. fA = (mA/rA)/((mA/rA) + (m B/rB)) xA = (mA/MWA)/((mA/MWA) + (m B/MWB)) 1 Solutions Three ways to get entropy and free energy of mixing A) Isothermal free energy expression, pressure expression B) Isothermal volume expansion approach, volume expression C) From statistical thermodynamics 2 Mix two ideal gasses, A and B p = pA + pB pA is the partial pressure pA = xAp For single component molar G = µ µ 0 is at p0,A = 1 bar At pressure pA for a pure component µ A = µ0,A + RT ln(p/p0,A) = µ0,A + RT ln(p) For a mixture of A and B with a total pressure ptot = p0,A = 1 bar and pA = xA ptot For component A in a binary mixture µ A(xA) = µ0.A + RT xAln (xA ptot/p0,A) = µ0.A + xART ln (xA) Notice that xA must be less than or equal to 1, so ln xA must be negative or 0 So the chemical potential has to drop in the solution for a solution to exist. Ideal gasses only have entropy so entropy drives mixing in this case. This can be written, xA = exp((µ A(xA) - µ 0.A)/RT) Which indicates that xA is the Boltzmann probability of finding A 3 Mix two real gasses, A and B µ A* = µ 0.A if p = 1 4 Ideal Gas Mixing For isothermal DU = CV dT = 0 Q = W = -pdV For ideal gas Q = W = nRTln(V f/Vi) Q = DS/T DS = nRln(V f/Vi) Consider a process of expansion of a gas from VA to V tot The change in entropy is DSA = nARln(V tot/VA) = - nARln(VA/V tot) Consider an isochoric mixing process of ideal gasses A and B. -

Calculation of Steam Volume Fraction in Subcooled Boiling
AE-28G UDC 535.248.2 CD 00 CN UJ < Calculation of Steam Volume Fraction in Subcooled Boiling S. Z. Rouhani AKTIEBOLAGET ATOMENERGI STOCKHOLM, SWEDEN 1967 AE -286 CALCULATION OF STEAM VOLUME FRACTION IN SUBCOOLED BOILING by S. Z . Rouhani SUMMARY An analysis of subcooled boiling is presented. It is assumed that he at is removed by vapor generation, heating of the liquid that replaces the detached bubbles, and to some extent by single phase heat transfer. Two regions of subcooled boiling are considered and a criterion is provided for obtaining the limiting value of subcooling between the two regions. Condensation of vapor in the subcooled liquid is analysed and the relative velocity of vapor with respect to the liquid is neglected in these regions. The theoretical arguments result in some equations for the calculation of steam volume frac tion and true liquid subcooling. Printed and distributed in June 1 967. LIST OF CONTENTS Page Introduction 3 Literature Survey 3 Theory 4 Assumptions and the Derivation of the Basic Equations 4 Remarks on the Liquid Subcooling 6 The integrated Equation of Subcooled Void 7 Estimation of the Rate of Bubble Condensation 9 Effects of Void and Channel Geometry on cp and cp^ 1 0 Effect of Subcooling on cp^ and cp^ 1 0 Effects of Mass Velocity, Heat Flux, and Physical Properties on cpj and cp,, 12 The Limiting Value of Subcooling in the First Region 1 3 Resume of Calculation Procedure 14 Calculations of a in the First Region 14 Calculation of O' in the Second Region 1 4 Steam Quality in Subcooled Boiling 1 5 Comparison with Experimental Data 1 5 Conclusion 15 Nomenclature 18 Greek Letters 20 References 22 Figure Captions 23 - 3 - INTRODUCTION The intensity of subcooled boiling depends on many factors, among which the degree of subcooling, surface heat flux, mass veloc ity, and physical properties of the liquid and its vapor. -

Greek Letters
Seader_44460_fm.qxd 8/30/05 5:15 PM Page xxvi xxvi Nomenclature Xm mole fraction of functional group m in y mole fraction in vapor phase; distance; mass UNIFAC method fraction in extract; mass fraction in overflow x mole fraction in liquid phase; mole fraction in y vector of mole fractions in vapor phase any phase; distance; mass fraction in raffinate; Z compressibility factor = Pv/RT; total mass; mass fraction in underflow; mass fraction of height particles Z froth height on a tray C f = / x normalized mole fraction xi xj 1 ZL length of liquid flow path across a tray j=1 Z¯ lattice coordination number in UNIQUAC and x vector of mole fractions in liquid phase UNIFAC equations xn fraction of crystals of size smaller than L z mole fraction in any phase; overall mole frac- Y mole or mass ratio; mass ratio of soluble mate- tion in combined phases; distance; overall mole rial to solvent in overflow; pressure-drop fraction in feed; dimensionless crystal size; factor for packed columns defined by (6-102); length of liquid flow path across tray concentration of solute in solvent; parameter z vector of mole fractions in overall mixture in (9-34) Greek Letters ␣ thermal diffusivity, k/CP ; relative volatility; ij binary interaction parameter in Wilson equation surface area per adsorbed molecule mV/L; radiation wavelength ␣∗ ideal separation factor for a membrane +, − limiting ionic conductances of cation and ␣ij relative volatility of component i with respect anion, respectively to component j for vapor-liquid equilibria; ij energy of interaction -

Compressed Sensing Reconstruction of 7 Tesla 23Na Multi-Channel Breast
Magnetic Resonance Imaging 60 (2019) 145–156 Contents lists available at ScienceDirect Magnetic Resonance Imaging journal homepage: www.elsevier.com/locate/mri Original contribution Compressed sensing reconstruction of 7 Tesla 23Na multi-channel breast T data using 1H MRI constraint ⁎ Sebastian Lachnera, , Olgica Zaricb, Matthias Utzschneidera, Lenka Minarikovab, Štefan Zbýňb,c, Bernhard Henseld, Siegfried Trattnigb, Michael Udera, Armin M. Nagela,e,f a Institute of Radiology, University Hospital Erlangen, Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), Erlangen, Germany b High Field MR Center, Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Vienna, Austria c Center for Magnetic Resonance Research, Department of Radiology, University of Minnesota, Minneapolis, MN, USA d Center for Medical Physics and Engineering, Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), Erlangen, Germany e Division of Medical Physics in Radiology, German Cancer Research Centre (DKFZ), Heidelberg, Germany f Institute of Medical Physics, Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), Erlangen, Germany ARTICLE INFO ABSTRACT Keywords: Purpose: To reduce acquisition time and to improve image quality in sodium magnetic resonance imaging (23Na 23 Sodium ( Na) breast MRI MRI) using an iterative reconstruction algorithm for multi-channel data sets based on compressed sensing (CS) 7 Tesla with anatomical 1H prior knowledge. Iterative reconstruction Methods: An iterative reconstruction for 23Na MRI with -
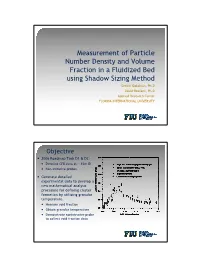
Measurement of Particle Number Density and Volume Fraction in A
Measurement of Particle Number Density and Volume Fraction in a Fluidized Bed using Shadow Sizing Method Seckin Gokaltun, Ph.D David Roelant, Ph.D Applied Research Center FLORIDA INTERNATIONAL UNIVERSITY Objective y 2006 Roadmap Task D1 & D2: y Detailed CFB data at ~.15m ID y Non-intrusive probes y Generate detailed experimental data to develop a new mathematical analysis procedure for defining cluster formation by utilizing granular temperature. y Measure void fraction y Obtain granular temperature y Demonstrate nonintrusive probe to collect void fraction data Granular Temperature Granular theory Kinetic theory y From the ideal gas law: y Assumptions: y Very large number of PV = NkBT particles (for valid statistical treatment) where kB is the Boltzmann y Distance among particles much larger than molecular constant and the absolute size temperature, thus: y Random particle motion with 2 constant speeds PV = NkBT = Nmvrms / 3 2 y Elastic particle-particle and T = mvrms / 3kB particle-walls collisions (no n loss of energy) v 2 = v 2 y Molecules obey Newton Laws rms ∑ i i =1 is the root-mean-square velocity Granular Temperature y From velocity 1 θ = ()σ 2 + σ 2 + σ 2 3 θ r z 2 2 where: σ z = ()u z − u y uz is particle velocity u is the average particle velocity y From voidage for dilute flows 2 3 θ ∝ ε s y From voidage for dense flows 2 θ ∝1 ε s 6 Glass beads imaged at FIU 2008 Volume Fraction y Solids volume fraction: nV ε = p s Ah y n : the number of particles y Vp : is the volume of single particle y A : the view area y h : the depth of view (Lecuona et al., Meas.