Final Program
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
An Introduction to Apophysis © Clive Haynes MMXX
Apophysis Fractal Generator An Introduction Clive Haynes Fractal ‘Flames’ The type of fractals generated are known as ‘Flame Fractals’ and for the curious, I append a note about their structure, gleaned from the internet, at the end of this piece. Please don’t ask me to explain it! Where to download Apophysis: go to https://sourceforge.net/projects/apophysis/ Sorry Mac users but it’s only available for Windows. To see examples of fractal images I’ve generated using Apophysis, I’ve made an Issuu e-book and here’s the URL. https://issuu.com/fotopix/docs/ordering_kaos Getting Started There’s not a defined ‘follow this method workflow’ for generating interesting fractals. It’s really a matter of considerable experimentation and the accumulation of a knowledge-base about general principles: what the numerous presets tend to do and what various options allow. Infinite combinations of variables ensure there’s also a huge serendipity factor. I’ve included a few screen-grabs to help you. The screen-grabs are detailed and you may need to enlarge them for better viewing. Once Apophysis has loaded, it will provide a Random Batch of fractal patterns. Some will be appealing whilst many others will be less favourable. To generate another set, go to File > Random Batch (shortcut Ctrl+B). Screen-grab 1 Choose a fractal pattern from the batch and it will appear in the main window (Screen-grab 1). Depending upon the complexity of the fractal and the processing power of your computer, there will be a ‘wait time’ every time you change a parameter. -

March 31, 2021
Units Cost Market Value US Equity Index Fund US Equities 95.82% Domestic Common Stocks 10X GENOMICS INC 126 10,868 24,673 1LIFE HEALTHCARE INC 145 6,151 4,794 2U INC 101 5,298 4,209 3D SYSTEMS CORP 230 5,461 9,193 3M CO 1,076 182,991 213,726 8X8 INC 156 2,204 4,331 A O SMITH CORP 401 17,703 28,896 A10 NETWORKS INC 58 350 653 AAON INC 82 3,107 5,132 AARON'S CO INC/THE 43 636 1,376 ABBOTT LABORATORIES 3,285 156,764 380,830 ABBVIE INC 3,463 250,453 390,072 ABERCROMBIE & FITCH CO 88 2,520 4,086 ABIOMED INC 81 6,829 25,281 ABM INDUSTRIES INC 90 2,579 3,992 ACACIA RESEARCH CORP 105 1,779 710 ACADIA HEALTHCARE CO INC 158 8,583 9,915 ACADIA PHARMACEUTICALS INC 194 6,132 4,732 ACADIA REALTY TRUST 47 1,418 1,032 ACCELERATE DIAGNOSTICS INC 80 1,788 645 ACCELERON PHARMA INC 70 2,571 8,784 ACCO BRANDS CORP 187 1,685 1,614 ACCURAY INC 64 483 289 ACI WORLDWIDE INC 166 3,338 6,165 ACTIVISION BLIZZARD INC 1,394 52,457 133,043 ACUITY BRANDS INC 77 13,124 14,401 ACUSHNET HOLDINGS CORP 130 2,487 6,422 ADAPTHEALTH CORP 394 14,628 10,800 ADAPTIVE BIOTECHNOLOGIES CORP 245 11,342 10,011 ADOBE INC 891 82,407 521,805 ADT INC 117 716 1,262 ADTALEM GLOBAL EDUCATION INC 99 4,475 3,528 ADTRAN INC 102 2,202 2,106 ADVANCE AUTO PARTS INC 36 6,442 7,385 ADVANCED DRAINAGE SYSTEMS INC 116 3,153 13,522 ADVANCED ENERGY INDUSTRIES INC 64 1,704 7,213 ADVANCED MICRO DEVICES INC 2,228 43,435 209,276 ADVERUM BIOTECHNOLOGIES INC 439 8,321 1,537 AECOM 283 12,113 17,920 AERIE PHARMACEUTICALS INC 78 2,709 1,249 AERSALE CORP 2,551 30,599 31,785 AES CORP/THE 1,294 17,534 33,735 AFFILIATED -

L'institution Royale Pour L'avancement
L’INSTITUTION ROYALE POUR L’AVANCEMENT DES SCIENCES / UNIVERSITÉ McGILL ACTIONS AMÉRICAINES │ au 31 mars 2019 Actions américaines d’une valeur supérieure à 500 000 $ cotées en bourse et détenues dans des comptes distincts (en $ CAN) GRAND CANYON EDUCATION INC 2 464 502 WADDELL & REED FINANCIAL INC 838 294 VIRTU FINANCIAL INC 2 098 163 DXP ENTERPRISES INC/TX 829 531 EURONET WORLDWIDE INC 2 075 232 OSHKOSH CORP 772 848 IRIDIUM COMMUNICATIONS INC 2 021 967 CIENA CORP 748 266 MARKETAXESS HOLDINGS INC 1 969 545 SNAP‐ON INC 710 950 UNIVERSAL HEALTH SERVICES INC 1 924 707 PULTEGROUP INC 705 975 MAXIMUS INC 1 697 760 VISHAY INTERTECHNOLOGY INC 703 237 ENVESTNET INC 1 539 593 UNUM GROUP 659 850 CHARLES RIVER LABORATORIES INT 1 531 805 LEAR CORP 652 686 CHEMED CORP 1 484 619 JETBLUE AIRWAYS CORP 649 127 MARRIOTT VACATIONS WORLDWIDE C 1 442 976 AVNET INC 643 136 US SILICA HOLDINGS INC 1 434 222 AMC NETWORKS INC 636 960 ACUSHNET HOLDINGS CORP 1 352 421 HUNTINGTON INGALLS INDUSTRIES 636 660 GENTHERM INC 1 321 685 WESTROCK CO 635 298 LAUREATE EDUCATION INC 1 308 706 CIT GROUP INC 628 038 FOX FACTORY HOLDING CORP 1 274 121 DOMTAR CORP 623 501 HURON CONSULTING GROUP INC 1 242 872 REGIONS FINANCIAL CORP 614 370 INTL. FCSTONE INC 1 242 806 ARBOR REALTY TRUST INC 608 950 RE/MAX HOLDINGS INC 1 238 584 QUEST DIAGNOSTICS INC 600 643 TEMPUR SEALY INTERNATIONAL INC 1 225 928 OWENS CORNING 598 025 GLOBUS MEDICAL INC 1 212 789 GLOBAL BRASS & COPPER HOLDINGS 593 531 THERMON GROUP HOLDINGS INC 1 209 830 FEDERAL AGRICULTURAL MORTGAGE 590 253 SHUTTERSTOCK INC 1 202 -
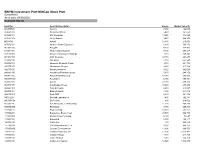
BNYM Investment Port:Midcap Stock Port (Unaudited) As of Date: 09/30/2020 Common Stocks
BNYM Investment Port:MidCap Stock Port (Unaudited) As of date: 09/30/2020 Common Stocks Identifier Security Description Shares Market Value ($) 002535300 Aaron's 7,450 422,043 00404A109 Acadia Healthcare 5,480 161,550 004498101 ACI Worldwide 13,250 346,223 00508Y102 Acuity Brands 9,470 969,255 BD845X2 Adient 12,480 216,278 00737L103 Adtalem Global Education 6,800 166,872 00766T100 AECOM 4,170 174,473 018581108 Alliance Data Systems 7,130 299,317 01973R101 Allison Transmission Holdings 7,110 249,845 00164V103 AMC Networks 10,710 264,644 023436108 Amedisys 2,760 652,547 025932104 American Financial Group 3,310 221,704 03073E105 AmerisourceBergen 2,220 215,162 042735100 Arrow Electronics 5,620 442,069 04280A100 Arrowhead Pharmaceuticals 5,670 244,150 045487105 Associated Banc-Corp 47,940 605,003 05329W102 Autonation 6,980 369,451 05368V106 Avient 23,030 609,374 053774105 Avis Budget Group 10,600 278,992 05464C101 Axon Enterprise 2,410 218,587 062540109 Bank of Hawaii 4,830 244,012 06417N103 Bank OZK 6,630 141,352 090572207 Bio-Rad Laboratories 1,480 762,881 09073M104 Bio-Techne 880 218,002 05550J101 BJs Wholesale Club Holdings 11,270 468,269 09227Q100 Blackbaud 3,750 209,363 103304101 Boyd Gaming 18,350 563,162 105368203 Brandywine Realty Trust 93,500 966,790 11120U105 Brixmor Property Group 6,300 73,647 117043109 Brunswick 8,150 480,117 12685J105 Cable One 300 565,629 127190304 CACI International, Cl. A 3,980 848,377 12769G100 Caesars Entertainment 11,890 666,553 133131102 Camden Property Trust 11,390 1,013,482 134429109 Campbell Soup 4,440 -

Bachelorarbeit Im Studiengang Audiovisuelle Medien Die
Bachelorarbeit im Studiengang Audiovisuelle Medien Die Nutzbarkeit von Fraktalen in VFX Produktionen vorgelegt von Denise Hauck an der Hochschule der Medien Stuttgart am 29.03.2019 zur Erlangung des akademischen Grades eines Bachelor of Engineering Erst-Prüferin: Prof. Katja Schmid Zweit-Prüfer: Prof. Jan Adamczyk Eidesstattliche Erklärung Name: Vorname: Hauck Denise Matrikel-Nr.: 30394 Studiengang: Audiovisuelle Medien Hiermit versichere ich, Denise Hauck, ehrenwörtlich, dass ich die vorliegende Bachelorarbeit mit dem Titel: „Die Nutzbarkeit von Fraktalen in VFX Produktionen“ selbstständig und ohne fremde Hilfe verfasst und keine anderen als die angegebenen Hilfsmittel benutzt habe. Die Stellen der Arbeit, die dem Wortlaut oder dem Sinn nach anderen Werken entnommen wurden, sind in jedem Fall unter Angabe der Quelle kenntlich gemacht. Die Arbeit ist noch nicht veröffentlicht oder in anderer Form als Prüfungsleistung vorgelegt worden. Ich habe die Bedeutung der ehrenwörtlichen Versicherung und die prüfungsrechtlichen Folgen (§26 Abs. 2 Bachelor-SPO (6 Semester), § 24 Abs. 2 Bachelor-SPO (7 Semester), § 23 Abs. 2 Master-SPO (3 Semester) bzw. § 19 Abs. 2 Master-SPO (4 Semester und berufsbegleitend) der HdM) einer unrichtigen oder unvollständigen ehrenwörtlichen Versicherung zur Kenntnis genommen. Stuttgart, den 29.03.2019 2 Kurzfassung Das Ziel dieser Bachelorarbeit ist es, ein Verständnis für die Generierung und Verwendung von Fraktalen in VFX Produktionen, zu vermitteln. Dabei bildet der Einblick in die Arten und Entstehung der Fraktale -

Apophysis :– an Intermediate User Guide
Apophysis :– An Intermediate User Guide By Carl Skepper (aka 2B2H) April 2006 Contents Introduction 3 Working with the Editor 4 Using my Metallica script 10 Falling in love with Julia (and Julia ‘n’) 15 Tiling (prepare to be disappointed) 24 Use of blur 31 Adding Colour to your flames 37 Introduction Welcome to my intermediate user guide to using the great freeware application called Apophysis , also affectionately known as ‘Apo’. I first downloaded this software on December 5 th 2005 and I have been hooked on it ever since. The variety of fractals it is able to produce is only limited by your creativity but saying that, your creativity amounts to nothing if you fail to persevere despite the lack of documentation out there. The definitive starter guides are those by Lance and for scripting, by Datagram. Links to both (and much more useful stuff) can be found at The Fractal Farm website : http://www.woosie.net/fracfan/viewtopic.php?t=15 These guides help you with the GUI and offer some basic advice on creating fractals. This guide is different. Together we will create specific flames so you can see how they are done. By doingthis I hope you will gain a better understandiing of Apo and use the knowledge to create your own fractal wonders ☺ It is not intended to teach you the basics of the GUI, those are covered in the docs linked at The Fractal Farm. It will show you a few tricks that you may not be aware of. I do not profess to be any kind of expert with the software. -

Usef-I Q2 2021
Units Cost Market Value U.S. EQUITY FUND-I U.S. Equities 88.35% Domestic Common Stocks 10X GENOMICS INC 5,585 868,056 1,093,655 1ST SOURCE CORP 249 9,322 11,569 2U INC 301 10,632 12,543 3D SYSTEMS CORP 128 1,079 5,116 3M CO 11,516 2,040,779 2,287,423 A O SMITH CORP 6,897 407,294 496,998 AARON'S CO INC/THE 472 8,022 15,099 ABBOTT LABORATORIES 24,799 2,007,619 2,874,948 ABBVIE INC 17,604 1,588,697 1,982,915 ABERCROMBIE & FITCH CO 1,021 19,690 47,405 ABIOMED INC 9,158 2,800,138 2,858,303 ABM INDUSTRIES INC 1,126 40,076 49,938 ACACIA RESEARCH CORP 1,223 7,498 8,267 ACADEMY SPORTS & OUTDOORS INC 1,036 35,982 42,725 ACADIA HEALTHCARE CO INC 2,181 67,154 136,858 ACADIA REALTY TRUST 1,390 24,572 30,524 ACCO BRANDS CORP 1,709 11,329 14,749 ACI WORLDWIDE INC 6,138 169,838 227,965 ACTIVISION BLIZZARD INC 13,175 839,968 1,257,422 ACUITY BRANDS INC 1,404 132,535 262,590 ACUSHNET HOLDINGS CORP 466 15,677 23,020 ADAPTHEALTH CORP 1,320 39,475 36,181 ADAPTIVE BIOTECHNOLOGIES CORP 18,687 644,897 763,551 ADDUS HOMECARE CORP 148 13,034 12,912 ADOBE INC 5,047 1,447,216 2,955,725 ADT INC 3,049 22,268 32,899 ADTALEM GLOBAL EDUCATION INC 846 31,161 30,151 ADTRAN INC 892 10,257 18,420 ADVANCE AUTO PARTS INC 216 34,544 44,310 ADVANCED DRAINAGE SYSTEMS INC 12,295 298,154 1,433,228 ADVANCED MICRO DEVICES INC 14,280 895,664 1,341,320 ADVANSIX INC 674 15,459 20,126 ADVANTAGE SOLUTIONS INC 1,279 14,497 13,800 ADVERUM BIOTECHNOLOGIES INC 1,840 7,030 6,440 AECOM 5,145 227,453 325,781 AEGLEA BIOTHERAPEUTICS INC 287 1,770 1,998 AEMETIS INC 498 6,023 5,563 AERSALE CORP -

Wilmington Funds Holdings Template DRAFT
Wilmington Large-Cap Strategy Fund as of 5/31/2021 (Portfolio composition is subject to change) ISSUER NAME % OF ASSETS APPLE INC 4.97% MICROSOFT CORP 4.69% AMAZON.COM INC 3.45% FACEBOOK INC 1.99% ALPHABET INC 1.80% ALPHABET INC 1.77% BERKSHIRE HATHAWAY INC 1.48% JPMORGAN CHASE & CO 1.35% TESLA INC 1.20% JOHNSON & JOHNSON 1.12% UNITEDHEALTH GROUP INC 0.98% VISA INC 0.96% NVIDIA CORP 0.96% BANK OF AMERICA CORP 0.89% HOME DEPOT INC/THE 0.87% WALT DISNEY CO/THE 0.82% MASTERCARD INC 0.80% PAYPAL HOLDINGS INC 0.77% EXXON MOBIL CORP 0.68% PROCTER & GAMBLE CO/THE 0.67% COMCAST CORP 0.66% ADOBE INC 0.62% INTEL CORP 0.59% VERIZON COMMUNICATIONS INC 0.59% CISCO SYSTEMS INC 0.57% CHEVRON CORP 0.55% PFIZER INC 0.54% NETFLIX INC 0.54% AT&T INC 0.53% SALESFORCE.COM INC 0.53% ABBOTT LABORATORIES 0.51% ABBVIE INC 0.50% MERCK & CO INC 0.48% WELLS FARGO & CO 0.48% BROADCOM INC 0.47% THERMO FISHER SCIENTIFIC INC 0.47% ACCENTURE PLC 0.46% CITIGROUP INC 0.45% MCDONALD'S CORP 0.44% TEXAS INSTRUMENTS INC 0.44% COCA-COLA CO/THE 0.44% HONEYWELL INTERNATIONAL INC 0.44% LINDE PLC 0.43% MEDTRONIC PLC 0.43% NIKE INC 0.43% ELI LILLY & CO 0.42% PEPSICO INC 0.42% UNITED PARCEL SERVICE INC 0.41% WALMART INC 0.40% DANAHER CORP 0.40% UNION PACIFIC CORP 0.40% QUALCOMM INC 0.38% BRISTOL-MYERS SQUIBB CO 0.37% ORACLE CORP 0.37% LOWE'S COS INC 0.36% BLACKROCK INC 0.35% CATERPILLAR INC 0.35% AMGEN INC 0.35% BOEING CO/THE 0.35% MORGAN STANLEY 0.35% COSTCO WHOLESALE CORP 0.35% RAYTHEON TECHNOLOGIES CORP 0.34% STARBUCKS CORP 0.34% GOLDMAN SACHS GROUP INC/THE 0.34% GENERAL ELECTRIC -

UNITED STATES BANKRUPTCY COURT SOUTHERN DISTRICT of FLORIDA Miami Division in Re: MIAMI INTERNATIONAL MEDI
Case 18-12741-LMI Doc 97 Filed 04/03/18 Page 1 of 23 UNITED STATES BANKRUPTCY COURT SOUTHERN DISTRICT OF FLORIDA Miami Division www.flsb.uscourts.gov In re: MIAMI INTERNATIONAL MEDICAL CENTER, LLC1 Case No. 18-12741-LMI d/b/a THE MIAMI MEDICAL CENTER, Chapter 11 Debtor. / SUPPLEMENTAL CERTIFICATE OF SERVICE I HEREBY CERTIFY that a true and correct copy of the Debtor’s Motion for Entry of (A) an Order Approving Bidding Procedures, (B) Approving Certain Protections to Stalking Horse Purchaser, (C) Approving Notice Procedures, and (D) an Order (I) Approving the Asset Purchase Agreement, (II) Authorizing the Sale of all or Substantially all of the Assets of the Debtor Free and Clear of all Liens, Claims, Encumbrances and Other Interests, (III) Authorizing the Assumption and Assignment of Certain Executory Contracts and Unexpired Leases, (IV) Scheduling Dates to Conduct Auction and Hearing to Consider Final Approval of Sale, and (V) Granting Related Relief [ECF No. 84] was served via Regular U.S. Mail on April 2, 2018, on all REMAINDER OF PAGE LEFT INTENTIONALLY BLANK 1The Debtor’s current mailing address is 5959 NW 7 St, Miami, FL 33126 and its EIN ends 4362. 1 LAW OFFICES OF MELAND RUSSIN & BUDWICK, P.A. 3200 SOUTHEAST FINANCIAL CENTER, 200 SOUTH BISCAYNE BOULEVARD, MIAMI, FLORIDA 33131 • TELEPHONE (305) 358-6363 Case 18-12741-LMI Doc 97 Filed 04/03/18 Page 2 of 23 parties listed on the Court’s Matrix attached hereto as Exhibit 12, and to all parties listed on the Patients Matrix which was filed under seal pursuant to Court Order [ECF No. -

1St Quarter 2014 FINAL BOOK
SCOTT-MACON HEALTHCARE REVIEW: FIRST QUARTER 2014 Healthcare Overview, Mean Revenue Multiples 2 Healthcare Overview, Mean EBITDA Multiples 4 Analysis of Selected Healthcare 6 Merger and Acquisition Transactions January 1—March 31, 2014 Analysis of Selected 22 CONTENTS Publicly-Traded Healthcare Companies SCOTT-MACON Healthcare Investment Banking 2 FIRST QUARTER 2014 HEALTHCARE REVIEW Dear Clients and Friends, Scott-Macon is pleased to present our quar- quisition of an Oklahoma health insurer by an invest- terly Healthcare Review covering the first quarter of ment firm, perhaps indicating that the perceived op- 2014. If you haven’t done so already, please email me portunities in this sector are now more significant at [email protected] to automatically con- than the potential pitfalls now that the Affordable tinue receiving our publications in the future as we Care Act is in full swing. Turning to Technology, are transitioning to digital publishing with email dis- once again we are seeing an incredibly diverse group tribution. of acquirors attracted to Healthcare Technology com- Pages four and five represent a visual snapshot panies—international companies, medical equipment of the average multiples for all of the healthcare, makers, private equity/investment firms and their medical and pharmaceutical transactions that either portfolio companies, and of course other Healthcare closed or were announced during the first quarter, (as well as Non-Healthcare) Technology companies, along with the average multiples for the major pub- both publicly-traded and privately-held. Outsourcing licly-traded healthcare, medical and pharmaceutical companies witnessed one of the busiest quarters we companies. have ever seen for this segment, a perennial favorite due to the inherent growth characteristics of the in- In the Insurance sector, there were two deals of dustry and the opportunities to create efficiencies for note in the First Quarter: the merger of two of the providers, payors and product companies as well. -

Michael Angelo Gomez – Exegesis
CCA1103 – Creativity: Theory, Practice, and History 1 CCA1103 – Creativity: Theory, Practice, and History Fractal Imaging: A Mini Exegesis by Michael Angelo Gomez 10445917 CCA1103 – Creativity: Theory, Practice, and History Project Exegesis Christopher Mason 2 CCA1103 – Creativity: Theory, Practice, and History Table of Contents I. Introduction ......................................................................................................................... 4 II. Purpose and Application.................................................................................................... 4 III. Theoretical Context .......................................................................................................... 6 IV. The Creative Process ..................................................................................................... 10 V. Conclusion ....................................................................................................................... 18 VI. Appendices ..................................................................................................................... 19 VII. References .................................................................................................................... 21 3 CCA1103 – Creativity: Theory, Practice, and History I. Introduction Upon the completion of my proposed creative project, a number of insights have been unearthed in light of the perception of my work now that it has reached its final stage of presentation and display. This reflection -

Furniture Design Inspired from Fractals
169 Rania Mosaad Saad Furniture design inspired from fractals. Dr. Rania Mosaad Saad Assistant Professor, Interior Design and Furniture Department, Faculty of Applied Arts, Helwan University, Cairo, Egypt Abstract: Keywords: Fractals are a new branch of mathematics and art. But what are they really?, How Fractals can they affect on Furniture design?, How to benefit from the formation values and Mandelbrot Set properties of fractals in Furniture Design?, these were the research problem . Julia Sets This research consists of two axis .The first axe describes the most famous fractals IFS fractals were created, studies the Fractals structure, explains the most important fractal L-system fractals properties and their reflections on furniture design. The second axe applying Fractal flame functional and aesthetic values of deferent Fractals formations in furniture design Newton fractals inspired from them to achieve the research objectives. Furniture Design The research follows the descriptive methodology to describe the fractals kinds and properties, and applied methodology in furniture design inspired from fractals. Paper received 12th July 2016, Accepted 22th September 2016 , Published 15st of October 2016 nearly identical starting positions, and have real Introduction: world applications in nature and human creations. Nature is the artist's inspiring since the beginning Some architectures and interior designers turn to of creation. Despite the different artistic trends draw inspiration from the decorative formations, across different eras- ancient and modern- and the geometric and dynamic properties of fractals in artists perception of reality, but that all of these their designs which enriched the field of trends were united in the basic inspiration (the architecture and interior design, and benefited nature).