The Role of Laminins in Cartilaginous Tissues: from Development to Regeneration
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
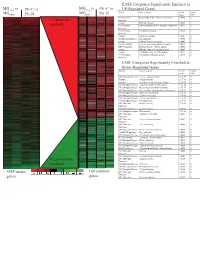
Supplement 1 Microarray Studies
EASE Categories Significantly Enriched in vs MG vs vs MGC4-2 Pt1-C vs C4-2 Pt1-C UP-Regulated Genes MG System Gene Category EASE Global MGRWV Pt1-N RWV Pt1-N Score FDR GO Molecular Extracellular matrix cellular construction 0.0008 0 110 genes up- Function Interpro EGF-like domain 0.0009 0 regulated GO Molecular Oxidoreductase activity\ acting on single dono 0.0015 0 Function GO Molecular Calcium ion binding 0.0018 0 Function Interpro Laminin-G domain 0.0025 0 GO Biological Process Cell Adhesion 0.0045 0 Interpro Collagen Triple helix repeat 0.0047 0 KEGG pathway Complement and coagulation cascades 0.0053 0 KEGG pathway Immune System – Homo sapiens 0.0053 0 Interpro Fibrillar collagen C-terminal domain 0.0062 0 Interpro Calcium-binding EGF-like domain 0.0077 0 GO Molecular Cell adhesion molecule activity 0.0105 0 Function EASE Categories Significantly Enriched in Down-Regulated Genes System Gene Category EASE Global Score FDR GO Biological Process Copper ion homeostasis 2.5E-09 0 Interpro Metallothionein 6.1E-08 0 Interpro Vertebrate metallothionein, Family 1 6.1E-08 0 GO Biological Process Transition metal ion homeostasis 8.5E-08 0 GO Biological Process Heavy metal sensitivity/resistance 1.9E-07 0 GO Biological Process Di-, tri-valent inorganic cation homeostasis 6.3E-07 0 GO Biological Process Metal ion homeostasis 6.3E-07 0 GO Biological Process Cation homeostasis 2.1E-06 0 GO Biological Process Cell ion homeostasis 2.1E-06 0 GO Biological Process Ion homeostasis 2.1E-06 0 GO Molecular Helicase activity 2.3E-06 0 Function GO Biological -

Collagen VI-Related Myopathy
Collagen VI-related myopathy Description Collagen VI-related myopathy is a group of disorders that affect skeletal muscles (which are the muscles used for movement) and connective tissue (which provides strength and flexibility to the skin, joints, and other structures throughout the body). Most affected individuals have muscle weakness and joint deformities called contractures that restrict movement of the affected joints and worsen over time. Researchers have described several forms of collagen VI-related myopathy, which range in severity: Bethlem myopathy is the mildest, an intermediate form is moderate in severity, and Ullrich congenital muscular dystrophy is the most severe. People with Bethlem myopathy usually have loose joints (joint laxity) and weak muscle tone (hypotonia) in infancy, but they develop contractures during childhood, typically in their fingers, wrists, elbows, and ankles. Muscle weakness can begin at any age but often appears in childhood to early adulthood. The muscle weakness is slowly progressive, with about two-thirds of affected individuals over age 50 needing walking assistance. Older individuals may develop weakness in respiratory muscles, which can cause breathing problems. Some people with this mild form of collagen VI-related myopathy have skin abnormalities, including small bumps called follicular hyperkeratosis on the arms and legs; soft, velvety skin on the palms of the hands and soles of the feet; and abnormal wound healing that creates shallow scars. The intermediate form of collagen VI-related myopathy is characterized by muscle weakness that begins in infancy. Affected children are able to walk, although walking becomes increasingly difficult starting in early adulthood. They develop contractures in the ankles, elbows, knees, and spine in childhood. -

The Beneficial Regulation of Extracellular Matrix
cosmetics Article The Beneficial Regulation of Extracellular Matrix and Heat Shock Proteins, and the Inhibition of Cellular Oxidative Stress Effects and Inflammatory Cytokines by 1α, 25 dihydroxyvitaminD3 in Non-Irradiated and Ultraviolet Radiated Dermal Fibroblasts Neena Philips *, Xinxing Ding, Pranathi Kandalai, Ilonka Marte, Hunter Krawczyk and Richard Richardson School of Natural Sciences, Fairleigh Dickinson University, Teaneck, NJ 07601, USA * Correspondence: [email protected] or [email protected] Received: 30 June 2019; Accepted: 20 July 2019; Published: 1 August 2019 Abstract: Intrinsic skin aging and photoaging, from exposure to ultraviolet (UV) radiation, are associated with altered regulation of genes associated with the extracellular matrix (ECM) and inflammation, as well as cellular damage from oxidative stress. The regulatory properties of 1α, 25dihydroxyvitamin D3 (vitamin D) include endocrine, ECM regulation, cell differentiation, photoprotection, and anti-inflammation. The goal of this research was to identify the beneficial effects of vitamin D in preventing intrinsic skin aging and photoaging, through its direct effects as well as its effects on the ECM, associated heat shock proteins (HSP-47, and -70), cellular oxidative stress effects, and inflammatory cytokines [interleukin (IL)-1 and IL-8] in non-irradiated, UVA-radiated, UVB-radiated dermal fibroblasts. With regard to the ECM, vitamin D stimulated type I collagen and inhibited cellular elastase activity in non-irradiated fibroblasts; and stimulated type I collagen and HSP-47, and inhibited elastin expression and elastase activity in UVA-radiated dermal fibroblasts. With regard to cellular protection, vitamin D inhibited oxidative damage to DNA, RNA, and lipids in non-irradiated, UVA-radiated and UVB-radiated fibroblasts, and, in addition, increased cell viability of UVB-radiated cells. -

Binding of Recombinant Human Cytokeratin 19 to Laminin
CELL STRUCTURE AND FUNCTION 25: 171–175 (2000) © 2000 by Japan Society for Cell Biology Binding of Recombinant Human Cytokeratin 19 to Laminin: A Possible Role in Interaction between Intermediate Filament Derived from Epithelial Cells and Extracellular Matrixes Naomi Dobashi1, Jiro Fujita1,*, Masayuki Murota2, Yuji Ohtsuki3, Shuji Bandoh1, Yutaka Ueda1, Kazutaka Dohmoto1, Satoko Hojo1, Mikio Nishioka2, Toshihiko Ishida, and Jiro Takahara1 1First Department of Internal Medicine, Kagawa Medical University, Kagawa 2Third Department of Internal Medicine, Kagawa Medical University, Kagawa 3Department of Pathology, Kochi Medical School, Kochi, Japan ABSTRACT. Cytokeratin 8 (CK8) and cytokeratin 19 (CK19) is a specific cytoskeletal component of simple epi- thelia, including bronchial epithelial cells. We hypothesized that CK8 or CK19 released from epithelial cells may bind to and cause damage to extracellular matrixes through binding of anti-CK8 or anti-CK19 autoantibodies. In the present study, bindings of recombinant human CK8 and CK19 to laminin (both derived from mouse sarcoma cells and human), collagen, gelatin, and fibronectin were evaluated by a modified enzyme-linked immunosorbent assay (ELISA). In addition, binding of CK19 to laminin was also confirmed by inhibition assay. As a result, CK19 strongly bound to mouse laminin as well as human laminin. Pretreatment with laminin significantly reduced the binding of CK19 to laminin. However, binding of recombinant CK19 to laminin was not demonstrated by Western immunoblot, suggesting that SDS treatment of laminin diminished the binding. These results suggest that released CK19 from epithelial cells may have played a role in the damage of basement membrane by accumulation of an immune complex composed by CK19 and anti-CK19 autoantibody. -

Dietary Protein Restriction Rapidly Reduces Transforming Growth Factor
Proc. Natl. Acad. Sci. USA Vol. 88, pp. 9765-9769, November 1991 Medical Sciences Dietary protein restriction rapidly reduces transforming growth factor p1 expression in experimental glomerulonephritis (extraceliular matrix/transforming growth factor 8/glomerulonephritis) SEIYA OKUDA*, TAKAMICHI NAKAMURA*, TATSUO YAMAMOTO*, ERKKI RUOSLAHTIt, AND WAYNE A. BORDER*t *Division of Nephrology, University of Utah School of Medicine, Salt Lake City, UT 84132; and tCancer Research Center, La Jolla Cancer Research Foundation, La Jolla, CA 92037 Communicated by Eugene Roberts, August 19, 1991 (receivedfor review April 29, 1991) ABSTRACT Dietary protein restriction has been shown to TGF-/31 on both cell types is to regulate the synthesis of two slow the rate of loss of kidney function in humans with chondroitin/dermatan sulfate proteoglycans, biglycan and progressive glomerulosclerosis due to glomerulonephritis or decorin, both of which can bind TGF-P1 (23). In an experi- diabetes mellitus. A central feature of glomerulosclerosis is the mental model ofglomerulonephritis in the rat, we have found pathological accumulation of extracellular matrix within the a close association between elevated expression of the diseased glomeruli. Transforming growth factor j1 (TGF-.81) TGF-131 gene and the development of glomerulonephritis is known to have widespread regulatory effects on extracellular (10). Seven days after glomerular injury, at the time of matrix and has been implicated as a major cause of increased significant extracellular matrix accumulation, the glomeruli extracellular matrix synthesis and buildup of pathological showed a 5-fold increase in TGF-f31 mRNA and a nearly matrix within glomeruli in experimental glomerulonephritis. 50-fold increase in production ofbiglycan and decorin. -

Congenital Muscular Dystrophy Due to Laminin Α2 (Merosin) Deficiency (MDC1A) in an Ethnic Malay Girl 1MK Thong, 3Sofiah Ali,4 YE Park, 5DS Kim, 6KJ Goh, 2KT Wong
Neurology Asia 2017; 22(2) : 155 – 159 Congenital muscular dystrophy due to laminin α2 (merosin) deficiency (MDC1A) in an ethnic Malay girl 1MK Thong, 3Sofiah Ali, 4YE Park, 5DS Kim, 6KJ Goh, 2KT Wong 1Departments of Paediatrics, 2Pathology and 6Medicine, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia; 3Sime Darby Medical Centre, Subang Jaya, Selangor, Malaysia; 4Department of Neurology and Biomedical Research Institute, Pusan National University Hospital, Busan, Korea; 5Department of Neurology, Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea Abstract We report the first known ethnic Malay patient with laminin alpha-2 (merosin) deficiency (MDC1A), a subtype of congenital muscular dystrophy (CMD)as a result of novel LAMA2 gene mutations. The 21-month-old female presented with hypotonia at birth and gross motor delay of her distal lower limbs. Physical examination showed generalised hypotonia, hyporeflexia and myopathic facies but good cognitive functions. Serum creatine kinase was elevated and white matter changes were detected in the brain MRI. Muscle biopsy showed dystrophic changes with complete laminin α2 deficiency by immunohistochemistry. Mutation analysis of LAMA2 showed compound heterozygote at exon 21, c.2888delG(p.Gly963Alafs*111) and exon 34, c.4886dupC(p.Pro1629Profs*40) leading to premature stop codon for each of the frameshift mutations. Patient review at seven years of age showed satisfactory cognitive functions despite having contractures and weakness. Genetic testing of LAMA2 related muscular dystrophy facilitated the earlier diagnosis of MDC1A and genetic counselling for this family. Keywords: laminin alpha-2 deficiency; merosin deficiency. LAMA2, Malaysia, congenital muscular dystrophy, MDC1A INTRODUCTION mutations in the laminin alpha-2 (LAMA2)gene. -

Extracellular Matrix Grafts: from Preparation to Application (Review)
INTERNATIONAL JOURNAL OF MOleCular meDICine 47: 463-474, 2021 Extracellular matrix grafts: From preparation to application (Review) YONGSHENG JIANG1*, RUI LI1,2*, CHUNCHAN HAN1 and LIJIANG HUANG1 1Science and Education Management Center, The Affiliated Xiangshan Hospital of Wenzhou Medical University, Ningbo, Zhejiang 315700; 2School of Chemistry, Sun Yat-sen University, Guangzhou, Guangdong 510275, P.R. China Received July 30, 2020; Accepted December 3, 2020 DOI: 10.3892/ijmm.2020.4818 Abstract. Recently, the increasing emergency of traffic acci- Contents dents and the unsatisfactory outcome of surgical intervention are driving research to seek a novel technology to repair trau- 1. Introduction matic soft tissue injury. From this perspective, decellularized 2. ECM-G characterization matrix grafts (ECM-G) including natural ECM materials, and 3. Methods of decellularization treatments their prepared hydrogels and bioscaffolds, have emerged as 4. Removal of residual cellular components and chemicals possible alternatives for tissue engineering and regenerative 5. Application of ECM-P in regenerative medicine medicine. Over the past decades, several physical and chemical 6. Challenges and future outlook on ECM-P decellularization methods have been used extensively to deal 7. Conclusions with different tissues/organs in an attempt to carefully remove cellular antigens while maintaining the non-immunogenic ECM components. It is anticipated that when the decellular- 1. Introduction ized biomaterials are seeded with cells in vitro or incorporated into irregularly shaped defects in vivo, they can provide the The extracellular matrix (ECM) derived from organs/tissues is appropriate biomechanical and biochemical conditions for a complex, highly organized assembly of macromolecules with directing cell behavior and tissue remodeling. -

Blood Vitronectin Is a Major Activator of LIF and IL-6 in the Brain Through Integrin–FAK and Upar Signaling Matthew P
© 2018. Published by The Company of Biologists Ltd | Journal of Cell Science (2018) 131, jcs202580. doi:10.1242/jcs.202580 RESEARCH ARTICLE Blood vitronectin is a major activator of LIF and IL-6 in the brain through integrin–FAK and uPAR signaling Matthew P. Keasey1, Cuihong Jia1, Lylyan F. Pimentel1,2, Richard R. Sante1, Chiharu Lovins1 and Theo Hagg1,* ABSTRACT Microglia and astrocytes express the VTN receptors αvβ3 and α β We defined how blood-derived vitronectin (VTN) rapidly and potently v 5 integrin (Herrera-Molina et al., 2012; Kang et al., 2008; activates leukemia inhibitory factor (LIF) and pro-inflammatory Milner, 2009; Welser-Alves et al., 2011). Microglia and astrocytes, interleukin 6 (IL-6) in vitro and after vascular injury in the brain. as well as endothelial cells, are major producers of pro- α in vitro Treatment with VTN (but not fibrinogen, fibronectin, laminin-111 or inflammatory cytokines, such as IL-6 and TNF , and collagen-I) substantially increased LIF and IL-6 within 4 h in after traumatic or ischemic injury to the brain (Banner et al., 1997; C6-astroglioma cells, while VTN−/− mouse plasma was less effective Erta et al., 2012; Lau and Yu, 2001) or upon self-induction by IL-6 than that from wild-type mice. LIF and IL-6 were induced by (Van Wagoner and Benveniste, 1999). IL-6 is a major regulator of a intracerebral injection of recombinant human (rh)VTN in mice, but variety of inflammatory disorders and a target for therapies (Hunter induction seen upon intracerebral hemorrhage was less in VTN−/− and Jones, 2015). -

Effects of Collagen-Derived Bioactive Peptides and Natural Antioxidant
www.nature.com/scientificreports OPEN Efects of collagen-derived bioactive peptides and natural antioxidant compounds on Received: 29 December 2017 Accepted: 19 June 2018 proliferation and matrix protein Published: xx xx xxxx synthesis by cultured normal human dermal fbroblasts Suzanne Edgar1, Blake Hopley1, Licia Genovese2, Sara Sibilla2, David Laight1 & Janis Shute1 Nutraceuticals containing collagen peptides, vitamins, minerals and antioxidants are innovative functional food supplements that have been clinically shown to have positive efects on skin hydration and elasticity in vivo. In this study, we investigated the interactions between collagen peptides (0.3–8 kDa) and other constituents present in liquid collagen-based nutraceuticals on normal primary dermal fbroblast function in a novel, physiologically relevant, cell culture model crowded with macromolecular dextran sulphate. Collagen peptides signifcantly increased fbroblast elastin synthesis, while signifcantly inhibiting release of MMP-1 and MMP-3 and elastin degradation. The positive efects of the collagen peptides on these responses and on fbroblast proliferation were enhanced in the presence of the antioxidant constituents of the products. These data provide a scientifc, cell-based, rationale for the positive efects of these collagen-based nutraceutical supplements on skin properties, suggesting that enhanced formation of stable dermal fbroblast-derived extracellular matrices may follow their oral consumption. Te biophysical properties of the skin are determined by the interactions between cells, cytokines and growth fac- tors within a network of extracellular matrix (ECM) proteins1. Te fbril-forming collagen type I is the predomi- nant collagen in the skin where it accounts for 90% of the total and plays a major role in structural organisation, integrity and strength2. -

Tendon Extracellular Matrix Remodeling and Defective Cell Polarization in the Presence of Collagen VI Mutations
cells Article Tendon Extracellular Matrix Remodeling and Defective Cell Polarization in the Presence of Collagen VI Mutations Manuela Antoniel 1,2, Francesco Traina 3,4, Luciano Merlini 5 , Davide Andrenacci 1,2, Domenico Tigani 6, Spartaco Santi 1,2, Vittoria Cenni 1,2, Patrizia Sabatelli 1,2,*, Cesare Faldini 7 and Stefano Squarzoni 1,2 1 CNR-Institute of Molecular Genetics “Luigi Luca Cavalli-Sforza”-Unit of Bologna, 40136 Bologna, Italy; [email protected] (M.A.); [email protected] (D.A.); [email protected] (S.S.); [email protected] (V.C.); [email protected] (S.S.) 2 IRCCS Istituto Ortopedico Rizzoli, 40136 Bologna, Italy 3 Ortopedia-Traumatologia e Chirurgia Protesica e dei Reimpianti d’Anca e di Ginocchio, Istituto Ortopedico Rizzoli di Bologna, 40136 Bologna, Italy; [email protected] 4 Dipartimento di Scienze Biomediche, Odontoiatriche e delle Immagini Morfologiche e Funzionali, Università Degli Studi Di Messina, 98122 Messina, Italy 5 Department of Biomedical and Neuromotor Sciences, University of Bologna, 40123 Bologna, Italy; [email protected] 6 Department of Orthopedic and Trauma Surgery, Ospedale Maggiore, 40133 Bologna, Italy; [email protected] 7 1st Orthopaedic and Traumatologic Clinic, IRCCS Istituto Ortopedico Rizzoli, 40136 Bologna, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-051-6366755; Fax: +39-051-4689922 Received: 20 December 2019; Accepted: 7 February 2020; Published: 11 February 2020 Abstract: Mutations in collagen VI genes cause two major clinical myopathies, Bethlem myopathy (BM) and Ullrich congenital muscular dystrophy (UCMD), and the rarer myosclerosis myopathy. In addition to congenital muscle weakness, patients affected by collagen VI-related myopathies show axial and proximal joint contractures, and distal joint hypermobility, which suggest the involvement of tendon function. -

LAMA2-Related Muscular Dystrophy
LAMA2-related muscular dystrophy Description LAMA2-related muscular dystrophy is a disorder that causes weakness and wasting ( atrophy) of muscles used for movement (skeletal muscles). This condition varies in severity, from a severe, early-onset type to a milder, late-onset form. Early-onset LAMA2-related muscular dystrophy is apparent at birth or within the first few months of life. It is considered part of a class of muscle disorders called congenital muscular dystrophies and is sometimes called congenital muscular dystrophy type 1A. Affected infants may have severe muscle weakness, lack of muscle tone (hypotonia), little spontaneous movement, and joint deformities (contractures). Weakness of the muscles in the face and throat can result in feeding difficulties and an inability to grow and gain weight at the expected rate. Respiratory insufficiency, which occurs when muscles in the chest are weakened, causes a weak cry and breathing problems that can lead to frequent, potentially life-threatening lung infections. As affected children grow, they often develop an abnormal, gradually worsening side-to- side curvature of the spine (scoliosis) and inward curvature of the back (lordosis). Children with early-onset LAMA2-related muscular dystrophy often do not develop the ability to walk. Difficulty with speech may result from weakness of the facial muscles and an enlarged tongue. Seizures occur in about a third of individuals with early-onset LAMA2-related muscular dystrophy; rarely, heart complications occur in this form of the disorder. Symptoms of late-onset LAMA2-related muscular dystrophy become evident later in childhood or adulthood, and are similar to those of a group of muscle disorders classified as limb-girdle muscular dystrophies. -

A Dual Laminin/Collagen Receptor Acts in Peripheral Nerve Regeneration (Extracellular Matrix/Integrin) B
Proc. Nati. Acad. Sci. USA Vol. 87, pp. 1319-1322, February 1990 Neurobiology A dual laminin/collagen receptor acts in peripheral nerve regeneration (extracellular matrix/integrin) B. TOYOTA, S. CARBONETTO, AND S. DAVID Centre for Research in Neuroscience, McGill University, Montreal General Hospital Research Institute, 1650 Cedar Avenue, Montreal, PQ H3G 1A4, Canada Communicated by Richard L. Sidman, November 28, 1989 (receivedfor review July 5, 1989) ABSTRACT A regeneration chamber was created in vivo extracts not only ofPC12 cells but also ofembryonic rat neural by suturing a synthetic tube sealed at its distal end onto the tissues (26). We show here that (i) laminin coated onto the nerve proximal stump of a severed rat sciatic nerve. Nerves regen- tubes enhances sciatic nerve regeneration and (ii) mAb 3A3 erated into tubes coated with laminin at a rate of 0.33 mm/day inhibits regeneration. These data suggest that the laminin/ after a lag of about 2 days. At 25 days, regenerating nerves had collagen integrin recognized by this antibody functions in re- extended 23% farther into laminin-coated tubes as compared generation in vivo. with uncoated ones. Monoclonal antibody 3A3, which func- tionally interferes with a dual lanminin/collagen receptor, MATERIALS AND METHODS inhibited nerve regeneration into laminin-coated tubes by 32%. Cell Culture. Cultures of dissociated chicken dorsal root In contrast, monoclonal antibody JG22, which inhibits chicken ganglia were prepared as described (27). Briefly, ganglia were matrix receptors, had no significant effect on regeneration. removed from 9-day-old chicken embryos treated with trypsin Immunohistochemical studies of teased adult rat sciatic nerves (0.025%) for 20 min at 37°C.