Centre for Reviews and Dissemination
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Therapeutic Class Overview Irritable Bowel Syndrome Agents
Therapeutic Class Overview Irritable Bowel Syndrome Agents Therapeutic Class Overview/Summary: This review will focus on agents used for the treatment of Irritable Bowel Syndrome (IBS).1-5 IBS is a gastrointestinal syndrome characterized primarily by non-specific chronic abdominal pain, usually described as a cramp-like sensation, and abnormal bowel habits, either constipation or diarrhea, in which there is no organic cause. Other common gastrointestinal symptoms may include gastroesophageal reflux, dysphagia, early satiety, intermittent dyspepsia and nausea. Patients may also experience a wide range of non-gastrointestinal symptoms. Some notable examples include sexual dysfunction, dysmenorrhea, dyspareunia, increased urinary frequency/urgency and fibromyalgia-like symptoms.6 IBS is defined by one of four subtypes. IBS with constipation (IBS-C) is the presence of hard or lumpy stools with ≥25% of bowel movements and loose or watery stools with <25% of bowel movements. When IBS is associated with diarrhea (IBS-D) loose or watery stools are present with ≥25% of bowel movements and hard or lumpy stools are present with <25% of bowel movements. Mixed IBS (IBS-M) is defined as the presence of hard or lumpy stools with ≥25% and loose or water stools with ≥25% of bowel movements. Final subtype, or unsubtyped, is all other cases of IBS that do not fall into the other classes. Pharmacological therapy for IBS depends on subtype.7 While several over-the-counter or off-label prescription agents are used for the treatment of IBS, there are currently only two agents approved by the Food and Drug Administration (FDA) for the treatment of IBS-C and three agents approved by the FDA for IBS-D. -
Prophylactic Antiemetic Therapy with Ondansetron, Granisetron and Metoclopramide in Patients Undergoing Laparoscopic Cholecystectomy Under GA
JK SCIENCE ORIGINAL ARTICLE Prophylactic Antiemetic Therapy with Ondansetron, Granisetron and Metoclopramide in Patients Undergoing Laparoscopic Cholecystectomy Under GA Vishal Gupta, Renu Wakhloo, Anjali Mehta, Satya Dev Gupta Abstract The aim of the present study was to compare the antiemetic effect of intravenous Granisetron, Ondansetron & Metoclopramide in a randomized blinded study for prophylaxis of post operative nausea and vomiting (PONV) in patients undergoing laparoscopic cholecystectomy under general anaesthesia. 60 patients (ASA I & II) undergoing laparoscopic cholecystectomy under general anaesthesia were randomly allocated into three equal groups (n=20). Emetic episodes in first 24 hours were recorded and compared in different study groups. Results were analyzed. Minimal emetic episodes were observed in early post-operative period (1-12hrs) in patients who had received intravenous granisetron in comparison to ondansetron and metoclopramide. However, after 12 hours emesis free periods were statistically insignificant between group A and B while patients in group C had no antiemetic effect. Keywords Post Operative Nausea and Vomiting (PONV), Granisetron, Ondensetron, Metoclopramide Introduction The most common and distressing symptoms, which vascular anastomoses and increased intracranial follow anaesthesia and surgery, are pain and emesis. The pressure(4). The anaesthetic consequences are aspiration syndrome of nausea, retching and vomiting is known as pneumonitis and discomfort in recovery. For institutions 'sickness' and each part of it can be distinguished as a there is increased financial burden because of increased separate entity (1). PONV (post operative nausea and nursing care, delayed discharge from Phase I and II vomiting) has been characterized as big 'little problem(2) recovery units and unexpected admissions. Hence, and has been a common complication for both in patients prophylactic antiemetic therapy is needed for all these and out patients undergoing virtually all types of surgical patients. -

Comprehensive Pgx Report for 1 / 31 Examples of Different Levels of Evidence for Pgx Snps
Comprehensive PGx report for PERSONAL DETAILS Advanced Diagnostics Laboratory LLC CLIA:31D2149403 Phone: Fax: PATIENT DOB Address: 1030 North Kings Highway Suite 304 Cherry Hill, NJ 08034 GENDER FEMALE Website: http://advanceddiagnosticslaboratory.com/ SPECIMEN TYPE Oral Fluid LABORATORY INFORMATION ORDERING PHYSICIAN ACCESSION NUMBER 100344 FACILITY COLLECTION DATE 08/10/2020 RECEIVED DATE 08/14/2020 REPORT GENERATED 09/08/2020 LABORATORY DIRECTOR Dr. Jeanine Chiaffarano Current Patient Medication Clonidine (Catapres, Kapvay) The personalized pharmacogenomics profile of this patient reveals intermediate CYP2D6-mediated metabolism, extensive CYP1A2-mediated metabolism, and extensive CYP3A5-mediated metabolism. For further details, please find supporting evidence in this report or on websites such as www.pharmgkb.org or www.fda.gov. Losartan (Cozaar) The personalized pharmacogenomics profile of this patient reveals extensive CYP2C9-mediated metabolism, extensive CYP3A4-mediated metabolism, and extensive CYP3A5-mediated metabolism. For further details, please find supporting evidence in this report or on websites such as www.pharmgkb.org or www.fda.gov. Diltiazem (Cardizem, Tiazac) The personalized pharmacogenomics profile of this patient reveals extensive CYP3A4-mediated metabolism, intermediate CYP2C19-mediated metabolism, and extensive CYP3A5- mediated metabolism. For further details, please find supporting evidence in this report or on websites such as www.pharmgkb.org or www.fda.gov. Labetalol (Normodyne, Trandate) The personalized pharmacogenomics profile of this patient reveals intermediate CYP2D6-mediated metabolism, and intermediate CYP2C19-mediated metabolism. For further details, please find supporting evidence in this report or on websites such as www.pharmgkb.org or www.fda.gov. Mycophenolate mofetil (Myfortic, CellCept) The personalized pharmacogenomics profile of this patient reveals extensive CYP3A4-mediated metabolism, extensive CYP3A5-mediated metabolism, and extensive CYP2C8-mediated metabolism. -

5-HT3 Receptor Antagonists in Neurologic and Neuropsychiatric Disorders: the Iceberg Still Lies Beneath the Surface
1521-0081/71/3/383–412$35.00 https://doi.org/10.1124/pr.118.015487 PHARMACOLOGICAL REVIEWS Pharmacol Rev 71:383–412, July 2019 Copyright © 2019 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: JEFFREY M. WITKIN 5-HT3 Receptor Antagonists in Neurologic and Neuropsychiatric Disorders: The Iceberg Still Lies beneath the Surface Gohar Fakhfouri,1 Reza Rahimian,1 Jonas Dyhrfjeld-Johnsen, Mohammad Reza Zirak, and Jean-Martin Beaulieu Department of Psychiatry and Neuroscience, Faculty of Medicine, CERVO Brain Research Centre, Laval University, Quebec, Quebec, Canada (G.F., R.R.); Sensorion SA, Montpellier, France (J.D.-J.); Department of Pharmacodynamics and Toxicology, School of Pharmacy, Mashhad University of Medical Sciences, Mashhad, Iran (M.R.Z.); and Department of Pharmacology and Toxicology, University of Toronto, Toronto, Ontario, Canada (J.-M.B.) Abstract. ....................................................................................384 I. Introduction. ..............................................................................384 II. 5-HT3 Receptor Structure, Distribution, and Ligands.........................................384 A. 5-HT3 Receptor Agonists .................................................................385 B. 5-HT3 Receptor Antagonists. ............................................................385 Downloaded from 1. 5-HT3 Receptor Competitive Antagonists..............................................385 2. 5-HT3 Receptor -

IBS Treatment
TREATMENTS OF IBS Douglas A. Drossman, MD Co-Director UNC Center for Functional GI & Motility Disorders INTRODUCTION In recent years, there has been increased interest by physicians and the pharmaceutical industry regarding newer treatments for IBS. Before discussing these new treatments, it is important to consider the overall management strategy in IBS. This is necessary because patients with IBS exhibit a wide spectrum of symptoms of varying frequencies and degrees of severity. There is no one ideal treatment for IBS, and the newer medications may work best for only a subset of patients having this disorder. Therefore, the clinician must first apply certain general management approaches and, following this, treatment choices will depend on the nature (i.e., predominant diarrhea, constipation, or bloating, etc.) and severity (mild, moderate, severe) of the symptoms. The symptoms of IBS may have any of several underlying causes. These can include: (a) abnormal motility (uncoordinated or excessive contractions that can lead to diarrhea, constipation, bloating) (b) visceral hypersensitivity (lower pain threshold of the nerves that can produce abdominal discomfort or pain) resulting from the abnormal motility, stress or infection (c) dysfunction of the brain's ability to regulate these visceral (intestinal) activities. Treatments will vary depending on which of these possibilities are occurring. In general, milder symptoms relate primarily to abnormal motility, often in response to food, activity or stress, and/or visceral hypersensitivity. They are commonly treated symptomatically with pharmacological agents directed at the gut. However, more severe symptoms often relate to dysfunction of the brain-gut regulatory system with associated psychosocial effects, and psychological or behavioral treatments and antidepressants are frequently helpful. -
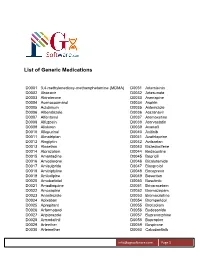
List of Generic Medications
List of Generic Medications D0001 3,4-methylenedioxy-methamphetamine (MDMA) D0031 Artemisinin D0002 Abacavir D0032 Artesunate D0003 Abiraterone D0033 Asenapine D0004 Acenocoumarol D0034 Aspirin D0005 Aclidinium D0035 Astemizole D0006 Albendazole D0036 Atazanavir D0007 Alfentanyl D0037 Atomoxetine D0008 Alfuzosin D0038 Atorvastatin D0009 Aliskiren D0039 Avanafil D0010 Allopurinol D0040 Axitinib D0011 Almotriptan D0041 Azathioprine D0012 Alogliptin D0042 Azilsartan D0013 Alosetron D0043 Bazedoxifene D0014 Alprazolam D0044 Bedaquiline D0015 Amantadine D0045 Bepridil D0016 Amiodarone D0046 Bicalutamide D0017 Amisulpride D0047 Bisoprolol D0018 Amitriptyline D0048 Boceprevir D0019 Amlodipine D0049 Bosentan D0020 Amobarbital D0050 Bosutinib D0021 Amodiaquine D0051 Brivaracetam D0022 Amoxapine D0052 Bromazepam D0023 Anastrozole D0053 Bromocriptine D0024 Apixaban D0054 Bromperidol D0025 Aprepitant D0055 Brotizolam D0026 Arformoterol D0056 Budesonide D0027 Aripiprazole D0057 Buprenorphine D0028 Armodafinil D0058 Bupropion D0029 Arteether D0059 Buspirone D0030 Artemether D0060 Cabozantinib [email protected] Page 1 List of Generic Medications D0061 Canagliflozin D0091 Clofarabine D0062 Cannabidiol (CBD) D0092 Clofibrate D0063 Cannabinol (CBN) D0093 Clomipramine D0064 Captopril D0094 Clonazepam D0065 Carbamazepine D0095 Clonidine D0066 Carisoprodol D0096 Clopidogrel D0067 Carmustine D0097 Clorazepate D0068 Carvedilol D0098 Clozapine D0069 Celecoxib D0099 Cocaine D0070 Ceritinib D0100 Codeine D0071 Cerivastatin D0101 Colchicine D0072 Cetirizine -

Efficacy of Eluxadoline in Irritable Bowel Syndrome with Diarrhea
This is a repository copy of Efficacy of Eluxadoline in Irritable Bowel Syndrome With Diarrhea. White Rose Research Online URL for this paper: http://eprints.whiterose.ac.uk/156693/ Version: Accepted Version Article: Black, CJ, Houghton, LA and Ford, AC orcid.org/0000-0001-6371-4359 (2020) Efficacy of Eluxadoline in Irritable Bowel Syndrome With Diarrhea. American Journal of Gastroenterology, 115 (3). pp. 483-484. ISSN 0002-9270 10.14309/ajg.0000000000000518 © The American College of Gastroenterology 2020. All Rights Reserved. This is an author produced version of correspondence published in The American Journal of Gastroenterology. Uploaded in accordance with the publisher's self-archiving policy. Reuse Items deposited in White Rose Research Online are protected by copyright, with all rights reserved unless indicated otherwise. They may be downloaded and/or printed for private study, or other acts as permitted by national copyright laws. The publisher or other rights holders may allow further reproduction and re-use of the full text version. This is indicated by the licence information on the White Rose Research Online record for the item. Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ Black et al Page 1 of 11 TITLE PAGE Title: Relative Efficacy of Eluxadoline in Irritable Bowel Syndrome. Authors: Christopher J. Black1, 2, Lesley A. Houghton, 2, Alexander C. Ford1, 2. 1Leeds Gastroenterology Institute, St. -

The Use of Stems in the Selection of International Nonproprietary Names (INN) for Pharmaceutical Substances
WHO/PSM/QSM/2006.3 The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances 2006 Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Medicines Policy and Standards The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -

Investigating the Pharmacology of Novel 5-HT3 Receptor Ligands; with the Potential to Treat Neuropsychiatric and Gastrointestinal Disorders
Investigating the pharmacology of novel 5-HT3 receptor ligands; with the potential to treat neuropsychiatric and gastrointestinal disorders by Alexander Roberts A thesis submitted to the University of Birmingham for the Degree of Doctor of Philosophy Institute of Clinical Sciences College of Medical and Dental Sciences University of Birmingham February 2020 University of Birmingham Research Archive e-theses repository This unpublished thesis/dissertation is copyright of the author and/or third parties. The intellectual property rights of the author or third parties in respect of this work are as defined by The Copyright Designs and Patents Act 1988 or as modified by any successor legislation. Any use made of information contained in this thesis/dissertation must be in accordance with that legislation and must be properly acknowledged. Further distribution or reproduction in any format is prohibited without the permission of the copyright holder. Abstract The 5-hydroxytryptamine (5-HT; serotonin) 5-HT3 receptor is an excitatory ligand- gated ion channel expressed in for example the brain and the gastrointestinal tract. Two major subtypes of the receptor have been studied in the most detail; the homomeric 5-HT3A receptor and the heteromeric 5-HT3AB receptor. 5-HT3 receptor antagonists are used clinically to treat chemotherapy induced and post-operative nausea and vomiting, and demonstrate symptomatic relief in diarrhoea-predominant irritable bowel syndrome (IBS-d); but unfortunately, these medications cause adverse effects such as constipation or rarely ischemic colitis in the latter condition. This study has characterised the pharmacology of two structurally distinct 5-HT3 receptor partial agonists (vortioxetine and CSTI-300); and identified the unique binding properties of the cryptic orthosteric modulator 5-chloroindole (Cl-indole) for the human (h) 5-HT3 receptor. -

Surveillance Review Proposal PDF 387 KB
National Institute for Health and Care Excellence Surveillance programme Surveillance proposal consultation document Irritable bowel syndrome NICE guideline CG61 – 8-year surveillance review Background information Guideline issue date: February 2008 3-year review (no update)* 6-year review (yes to update) *Although the 3-year review decision was no update, the findings were subsequently used to pilot the NICE’s rapid update process. Surveillance proposal for consultation We will not update the guideline at this time. Reason for the proposal New evidence We found 105 new studies in a search for randomised controlled trials (RCTs) and systematic reviews published between 01 September 2013 and 18 July 2016. We also considered studies identified by members of the guideline committee who originally worked on this guideline. Evidence identified in previous surveillance 3 years and 6 years after publication of the guideline was also considered. This included 52 studies identified by search. From all sources, 157 studies were considered to be relevant to the guideline. Surveillance proposal consultation document for Irritable bowel syndrome (2008) NICE guideline CG61 1 of 44 This included new evidence that is consistent with current recommendations on: diagnosis of irritable bowel syndrome (IBS) dietary interventions physical activity interventions drug treatments (antispasmodics, laxatives, anti-motility agents and antidepressants) psychotherapy hypnotherapy, biofeedback and relaxation therapy acupuncture and patient information. We also identified new evidence in the following areas that was inconsistent with, or not covered by, current recommendations, but the evidence was not considered to impact on the guideline: ondansetron vitamin D supplementation herbal medicines. We did not find any new evidence on reflexology, psychosocial interventions, or self-help and support groups. -

2015.09 IBS Drug Class Review.Pdf
Drug Class Review Agents Indicated in the Treatment of Irritable Bowel Syndrome 56:92 GI Drugs, Miscellaneous Alosetron (Lotronex®) Eluxadoline (Viberzi®) Linaclotide (Linzess®) Lubiprostone (Amitiza®) Tegaserod (Zelnorm®) Final Report September 2015 Review prepared by: Melissa Archer, PharmD, Clinical Pharmacist Irene Pan, PharmD Candidate 2016 Chelsey Hancock, PharmD Candidate 2016 Carin Steinvoort, PharmD, Clinical Pharmacist Gary Oderda, PharmD, MPH, Professor University of Utah College of Pharmacy Copyright © 2015 by University of Utah College of Pharmacy Salt Lake City, Utah. All rights reserved. 1 Table of Contents Executive Summary ......................................................................................................................... 3 Introduction .................................................................................................................................... 4 Table 1. Comparison of the Agents Indicated in the Treatment of IBS ................................. 5 Disease Overview ........................................................................................................................ 6 Table 2. Summary of IBS Treatment Options ........................................................................ 8 Table 3. IBS Disease Staging System .................................................................................... 11 Table 4. Most Current Clinical Practice Guidelines for the Treatment of IBS ..................... 13 Pharmacology .............................................................................................................................. -

Elite Pgx Report
Comprehensive PGx report for SANDRA HENRY PERSONAL DETAILS Redwood Lab Services LLC CLIA:45D2108203 Fax: PATIENT ENRY DOB 281-378-2116 281-466-2483 Address: 6776 Southwest Fwy Suite 600, Houston, TX 77074 GENDER Female Website: http://www.redwoodlabservices.com/ SPECIMEN TYPE Buccal Swab LABORATORY INFORMATION ORDERING PHYSICIAN - ACCESSION NUMBER 2006271582 FACILITY Elite Clinical Lab COLLECTION DATE 06/03/2020 RECEIVED DATE 07/01/2020 REPORT GENERATED 09/21/2020 LABORATORY DIRECTOR Chad Harper Current Patient Medication This patient is either not receiving any medication or may be receiving medications that are outside the scope of this report. A medication has potentially reduced ecacy, increased toxicity or the patient has a risk for the indicated condition. Guidelines exist for adjusting dosage, increased vigilance or the patient has risk for the indicated condition. The medication can be prescribed according to standard regimens or the patient's risk for the indicated condition is not increased. Comprehensive PGx report for SANDRA HENRY 1 / 29 G E NOTYP E /HAP L OTYP E /P HE NOTYP E DE TAIL Dis claimer: No patient should evaluate or use the information contained herein without the advice, consultation and supervision of a licensed healthcare professional such as a pharmacist or G ene G enotype-Haplotype P henotype physician. Laboratory-developed testing characteristics and protocols. R esults have not been reviewed or approved by the U.S . Food & Drug Administration (FDA). * This call was defaulted to the wild-type allele frequency because during review of the genotyping data, the genotype was C YP 1A2 *1A/*1A E xtensive metabolizer indeterminate.