Quarterly Monitoring Report- Haryana
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

STATISTICAL REPORT GENERAL ELECTIONS, 2004 the 14Th LOK SABHA
STATISTICAL REPORT ON GENERAL ELECTIONS, 2004 TO THE 14th LOK SABHA VOLUME III (DETAILS FOR ASSEMBLY SEGMENTS OF PARLIAMENTARY CONSTITUENCIES) ELECTION COMMISSION OF INDIA NEW DELHI Election Commission of India – General Elections, 2004 (14th LOK SABHA) STATISCAL REPORT – VOLUME III (National and State Abstracts & Detailed Results) CONTENTS SUBJECT Page No. Part – I 1. List of Participating Political Parties 1 - 6 2. Details for Assembly Segments of Parliamentary Constituencies 7 - 1332 Election Commission of India, General Elections, 2004 (14th LOK SABHA) LIST OF PARTICIPATING POLITICAL PARTIES PARTYTYPE ABBREVIATION PARTY NATIONAL PARTIES 1 . BJP Bharatiya Janata Party 2 . BSP Bahujan Samaj Party 3 . CPI Communist Party of India 4 . CPM Communist Party of India (Marxist) 5 . INC Indian National Congress 6 . NCP Nationalist Congress Party STATE PARTIES 7 . AC Arunachal Congress 8 . ADMK All India Anna Dravida Munnetra Kazhagam 9 . AGP Asom Gana Parishad 10 . AIFB All India Forward Bloc 11 . AITC All India Trinamool Congress 12 . BJD Biju Janata Dal 13 . CPI(ML)(L) Communist Party of India (Marxist-Leninist) (Liberation) 14 . DMK Dravida Munnetra Kazhagam 15 . FPM Federal Party of Manipur 16 . INLD Indian National Lok Dal 17 . JD(S) Janata Dal (Secular) 18 . JD(U) Janata Dal (United) 19 . JKN Jammu & Kashmir National Conference 20 . JKNPP Jammu & Kashmir National Panthers Party 21 . JKPDP Jammu & Kashmir Peoples Democratic Party 22 . JMM Jharkhand Mukti Morcha 23 . KEC Kerala Congress 24 . KEC(M) Kerala Congress (M) 25 . MAG Maharashtrawadi Gomantak 26 . MDMK Marumalarchi Dravida Munnetra Kazhagam 27 . MNF Mizo National Front 28 . MPP Manipur People's Party 29 . MUL Muslim League Kerala State Committee 30 . -
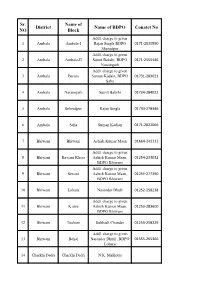
Sr. NO District Name of Block Name of BDPO Conatct No
Sr. Name of District Name of BDPO Conatct No NO Block Addl. charge to given 1 Ambala Ambala-I Rajan Singla BDPO 0171-2530550 Shazadpur Addl. charge to given 2 Ambala Ambala-II Sumit Bakshi, BDPO 0171-2555446 Naraingarh Addl. charge to given 3 Ambala Barara Suman Kadain, BDPO 01731-283021 Saha 4 Ambala Naraingarh Sumit Bakshi 01734-284022 5 Ambala Sehzadpur Rajan Singla 01734-278346 6 Ambala Saha Suman Kadian 0171-2822066 7 Bhiwani Bhiwani Ashish Kumar Maan 01664-242212 Addl. charge to given 8 Bhiwani Bawani Khera Ashish Kumar Maan, 01254-233032 BDPO Bhiwani Addl. charge to given 9 Bhiwani Siwani Ashish Kumar Maan, 01255-277390 BDPO Bhiwani 10 Bhiwani Loharu Narender Dhull 01252-258238 Addl. charge to given 11 Bhiwani K airu Ashish Kumar Maan, 01253-283600 BDPO Bhiwani 12 Bhiwani Tosham Subhash Chander 01253-258229 Addl. charge to given 13 Bhiwani Behal Narender Dhull , BDPO 01555-265366 Loharu 14 Charkhi Dadri Charkhi Dadri N.K. Malhotra Addl. charge to given 15 Charkhi Dadri Bond Narender Singh, BDPO 01252-220071 Charkhi Dadri Addl. charge to given 16 Charkhi Dadri Jhoju Ashok Kumar Chikara, 01250-220053 BDPO Badhra 17 Charkhi Dadri Badhra Jitender Kumar 01252-253295 18 Faridabad Faridabad Pardeep -I (ESM) 0129-4077237 19 Faridabad Ballabgarh Pooja Sharma 0129-2242244 Addl. charge to given 20 Faridabad Tigaon Pardeep-I, BDPO 9991188187/land line not av Faridabad Addl. charge to given 21 Faridabad Prithla Pooja Sharma, BDPO 01275-262386 Ballabgarh 22 Fatehabad Fatehabad Sombir 01667-220018 Addl. charge to given 23 Fatehabad Ratia Ravinder Kumar, BDPO 01697-250052 Bhuna 24 Fatehabad Tohana Narender Singh 01692-230064 Addl. -

Annexure-V State/Circle Wise List of Post Offices Modernised/Upgraded
State/Circle wise list of Post Offices modernised/upgraded for Automatic Teller Machine (ATM) Annexure-V Sl No. State/UT Circle Office Regional Office Divisional Office Name of Operational Post Office ATMs Pin 1 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA PRAKASAM Addanki SO 523201 2 Andhra Pradesh ANDHRA PRADESH KURNOOL KURNOOL Adoni H.O 518301 3 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM AMALAPURAM Amalapuram H.O 533201 4 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Anantapur H.O 515001 5 Andhra Pradesh ANDHRA PRADESH Vijayawada Machilipatnam Avanigadda H.O 521121 6 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA TENALI Bapatla H.O 522101 7 Andhra Pradesh ANDHRA PRADESH Vijayawada Bhimavaram Bhimavaram H.O 534201 8 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA VIJAYAWADA Buckinghampet H.O 520002 9 Andhra Pradesh ANDHRA PRADESH KURNOOL TIRUPATI Chandragiri H.O 517101 10 Andhra Pradesh ANDHRA PRADESH Vijayawada Prakasam Chirala H.O 523155 11 Andhra Pradesh ANDHRA PRADESH KURNOOL CHITTOOR Chittoor H.O 517001 12 Andhra Pradesh ANDHRA PRADESH KURNOOL CUDDAPAH Cuddapah H.O 516001 13 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM VISAKHAPATNAM Dabagardens S.O 530020 14 Andhra Pradesh ANDHRA PRADESH KURNOOL HINDUPUR Dharmavaram H.O 515671 15 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA ELURU Eluru H.O 534001 16 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudivada Gudivada H.O 521301 17 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudur Gudur H.O 524101 18 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Guntakal H.O 515801 19 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA -
DISTRICT MAP JIND a Padarath Khera Hansdehar
76.093252 76.262509 76.431766 76.601023 76.770280 B Dhandoli DISTRICT MAP JIND A Padarath Khera Hansdehar J Dhanoury Rewar N Datasinghwala U P Naraingarh Garhi Dubal L/ Dr Pipaltha L Nepewala i K Koel n oe k r l L D /D B l uba R. Dhabi Teksingh a D r w K ura a r Li l nk a D R.. isty Dhamtan D K ® o e l Rasidan r S e u d b e M e Ujhana F r Ujhana . n a 0 4.5 9 18 27 w l a k r. M Kharal l ra Kalwan a . h 1 K o l K n e a Kilometers lw Dhamtan Sahib r n a D 1 n 1 n 9 S a 9 8 u n 8 a b 7 a Ambarsar 7 h M 8 r jh 8 6 . 6 . C U K 9 9 k 2 2 n i . L r n D a t a Gurusar A h m k a r h r a Loan o l D in e M B di Hamirgarh ro I ha Sulehra Julehra D D Belrakha Bhana Brahmanan T Harnampura s e Sheogarh urf Surajkhera ic rv e Phulian Kalan S H r A te Rajgarh Dhobi a W r Phulian Khurd u p Karamgarh m a Dharodi Gurthali d A Lohchab2 A ch n B Kanha Khera Mohalkhera ra B Bidhrana sa r ir Hatho L Khanpur de S ee . F r Amargarh rh r M ga sa al in Khararwal oh S A M w I e Nehra sm N a Ismailpur ilp u Singwal Narwana r Narwana M Sisar Frain Kalan r. -

District Wise List of Registered and Un-Registered Gaushalas of Haryana State Alongwith Number of Animals Kept in the Gaushalas. AMBALA S.No
District wise List of Registered and Un-Registered Gaushalas of Haryana State alongwith number of Animals kept in the Gaushalas. AMBALA S.No. Distt. Name of Gaushala Haryana Regn. No. No. of Animals Sr. No. 1 1 Shri Rambag Gaushala, Rambag road, 607 412 Ambala Cantt. 2 2 Shri Kewal Krishan Miglani Gaushala 560 462 Samiti, Purani Gaas Mandi, Ambala City 3 3 Gaushala Trust Society,Spatu Road Ambala 1860 444 City 4 4 Gori Shanker Gau Raksha Samiti, Kalpi, 371 215 Near Power House, Saha, Distt. Ambala 5 5 Shri Govind Gaushala Samiti,Barara, Distt. 128 546 Ambala. 6 6 Shri Krishan Gaushala Samiti, Yamkeshwar 1035 939 Tirth Huseni, Naraingarh, Distt. Ambala. 7 7 Gurcharan Gaushalas Sanstha, Vill Bhunni, 40 25 P.O. Sonta, Distt. Ambala 8 8 Shri Radha Madhav Gaudham, Vill Mokha 642 94 Majra, Distt. Ambala. Total number of Animals 3137 BHIWANI 9 1 Shri Gaushala Trust, Bhiwani, Distt. 11 3890 Bhiwani. 10 2 Shri Shiv Dharmarth Gaushala, Dhuleri, 277 609 Distt. Bhiwani. 11 3 Shri Krishan Gaushala, Bamla 256 70 12 4 Shri Shyam Gaushala Trust, Mandana, 2800 234 Distt. Bhiwani. 13 5 Shri Rishi Kul Gaushala, Nimbriwali, Tehsil 40 277 & Distt. Bhiwani 14 6 Shri Gomath Gaushala, Leghan, Distt. 981 323 Bhiwani 15 7 Shri Shiv Muni Gaushala, Jitwawas, Post 436 488 office Leghan, Distt. Bhiwani 16 8 Shri Krishan Sudama Maitri Gaushala 3030 420 Society, V.P.O. Kharak Kalan , Distt. Bhiwani. 17 9 Shri Baba Dhuniwala Gau-Sewa Trust, 359 2803 Dinod, Distt. Bhiwani 18 10 Shri Krishan Gaushala,Tosham Road, 727 2205 Siwani Mandi, Distt. -
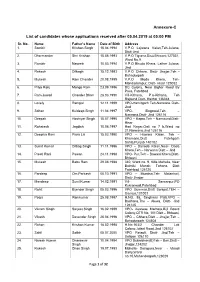
Annexure-C List of Candidates Whose Applications Received After 05.04
Annexure-C List of candidates whose applications received after 05.04.2019 at 05:00 PM Sr. No. Name Father’s Name Date of Birth Address 1. Sombir Krishan Singh 15.04.1994 V.P.O Lajwana Kalan,Teh-Julana, Distt-Jind 2. Dharmender Shri Krishan 15.08.1993 V.P.O Tigrana,Distt Bhiwani,127031, Ward No.9 3. Rambir Naseeb 10.03.1994 V.P.O Bhuda Khera, Lather Julana, Jind 4. Rakesh Dilbagh 15.12.1993 V.P.O Chhara, Distt- Jhajjar,Teh - Bahadurgarh 5. Mukesh Ram Chander 20.08.1995 V.P.O Moda Khera, Teh- Mandadampur, Distt- Hisar 125052 6. Priya Ranj Mange Ram 23.09.1996 DC Colony, Near Bighar Road By Pass, Fatehbad 7. Ram Juwari Chander Bhan 28.03.1990 Vill-Kithana, P.o-Kithana, Teh Rajaund,Distt- Kaithal 136044 8. Lovely Rampal 12.11.1999 VPO-Hamirgarh Teh-Narwana Distt- Jind 9. Sohan Kuldeep Singh 11.04.1997 VPO- Singowal,Teh – Narwana,Distt- Jind 126116 10. Deepak Hoshiyar Singh 15.07.1995 VPO – Kapro,Teh – Narnaund,Distt- Hisar 11. Rohatash Jagdish 10.06.1997 Hari Nagar,Gali no 7 b,Ward no 21,Narwana,Jind 126116 12. Deepika Rani Piara Lal 15.03.1990 VPO – Hawara Kalan, Teh – Khamano,Distt Fatehgarh Sahib,Punjab 140102 13. Sumit Kumar Dilbag Singh 11.11.1996 VPO – Danoda Kalan,Near- Dada Khera,Teh – Narwana Distt – Jind 14. Preeti Rani Pawan 24.11.1998 VPO- Pur,Teh – Bawani Khera,Distt- Bhiwani 15. Mukesh Babu Ram 29.08.1988 340, Ward no. 9, Killa Mohalla, Near Balmiki Mandir, Tohana, Distt Fatehbad 125120 16. -
Flood Control Order-2021 District Jind
Flood Control Order-2021 District Jind Flood Control Order-2013 (First Edition) Flood Control Order-2014 (Second Edition) Flood Control Order-2015 (Third Edition) Flood Control Order-2016 (Fourth Edition) Flood Control Order-2017 (Fifth Edition) Flood Control Order-2018 (Sixth Edition) Flood Control Order-2019 (Seventh Edition) Flood Control Order-2020 (Eighth Edition) Flood Control Order-2021 (Ninth Edition) 1 | Page Preface Flood impact is one of the most significant disasters occur in every where. Causes of floods are due to natural factors such as heavy rainfall, high floods and high tides, etc, and human factors such as blocking of channels or aggravation of drainage channels, improper land use, deforestation in headwater regions, etc as a result losses of life and damage of properties occur. Flood loss prevention and mitigation includes structural flood control measures such as constitution of dams or river dikes and Non-structural measure includes flood forecasting and Dr. Aditya Dahiya, I.A.S, Deputy Commissioner, warning, flood hazard and risk management. Jind. These papers describe concepts taken by District administration policy, plan and operation on integrated flood disaster. District administration is well prepared to tackle any eventuality due to flood or heavy down pour. Keeping in view a thorough inspection of drains, canals and pump houses was done. Drain and canals are being cleared to contain and carry more water during the rainy season; Pump Houses are made fully operative to drain out excess water in the time of need. All front line departments have already established their flood control room along with smooth working condition of all resources inventory of their own. -

Officewise Postal Addresses of Public Health Engineering Deptt. Haryana
Officewise Postal Addresses of Public Health Engineering Deptt. Haryana Sr. Office Type Office Name Postal Address Email-ID Telephone No No. 1 Head Office Head Office Public Health Engineering Department, Bay No. 13 [email protected] 0172-2561672 -18, Sector 4, Panchkula, 134112, Haryana 2 Circle Ambala Circle 28, Park road, Ambala Cantt [email protected]. 0171-2601273 in 3 Division Ambala PHED 28, PARK ROAD,AMBALA CANTT. [email protected] 0171-2601208 4 Sub-Division Ambala Cantt. PHESD No. 2 28, PARK ROAD AMBALA CANTT. [email protected] 0171-2641062 5 Sub-Division Ambala Cantt. PHESD No. 4 28, PARK ROAD, AMBALA CANTT. [email protected] 0171-2633661 6 Sub-Division Ambala City PHESD No. 1 MODEL TOWN, AMBALA CITY [email protected] 0171-2601208 7 Division Ambala City PHED MODEL TOWN, AMBALA CITY NEAR SHARDA [email protected] 0171-2521121 RANJAN HOSPITAL OPP. PARK 8 Sub-Division Ambala City PHESD No. 3 MODEL TOWN, AMBALA CITY [email protected] 0171-2521121 9 Sub-Division Ambala City PHESD No. 5 MODEL TOWN, AMBALA CITY. [email protected] 0171-2521121 10 Sub-Division Ambala City PHESD No. 6 28, PARK ROAD, AMBALA CANTT. [email protected] 0171-2521121 11 Division Yamuna Nagar PHED No. 1 Executive engineer, Public health engineering [email protected] 01732-266050 division-1, behind Meat and fruit market, Industrial area Yamunanagar. 12 Sub-Division Chhachhrouli PHESD Near Community centre Chhachhrouli. [email protected] 01735276104 13 Sub-Division Jagadhri PHESD No. -
Uchana Kalan Assembly Haryana Factbook
Editor & Director Dr. R.K. Thukral Research Editor Dr. Shafeeq Rahman Compiled, Researched and Published by Datanet India Pvt. Ltd. D-100, 1st Floor, Okhla Industrial Area, Phase-I, New Delhi- 110020. Ph.: 91-11- 43580781, 26810964-65-66 Email : [email protected] Website : www.electionsinindia.com Online Book Store : www.datanetindia-ebooks.com Report No. : AFB/HR-37-0118 ISBN : 978-93-5293-551-2 First Edition : January, 2018 Third Updated Edition : June, 2019 Price : Rs. 11500/- US$ 310 © Datanet India Pvt. Ltd. All rights reserved. No part of this book may be reproduced, stored in a retrieval system or transmitted in any form or by any means, mechanical photocopying, photographing, scanning, recording or otherwise without the prior written permission of the publisher. Please refer to Disclaimer at page no. 139 for the use of this publication. Printed in India No. Particulars Page No. Introduction 1 Assembly Constituency at a Glance | Features of Assembly as per 1-2 Delimitation Commission of India (2008) Location and Political Maps 2 Location Map | Boundaries of Assembly Constituency in District | Boundaries 3-9 of Assembly Constituency under Parliamentary Constituency | Town & Village-wise Winner Parties- 2014-PE, 2014-AE, 2009-PE and 2009-AE Administrative Setup 3 District | Sub-district | Towns | Villages | Inhabited Villages | Uninhabited 10-14 Villages | Village Panchayat | Intermediate Panchayat Demographics 4 Population | Households | Rural/Urban Population | Towns and Villages by 15-16 Population Size | Sex Ratio -

Har Ryana a Go Overn Nment T Gaz Zette
Haryana Government Gazette EXTRAORDINARY Published by Authority © Govt. of Haryana No. 111–2021/Ext.] CHANDIGARH, MONDAY, JULY 12, 2021 (ASADHA 21, 1943 SAKA) gfj;k.kk ljdkj uxj rFkk xzke vk;kstuk foHkkx rFkk ’kgjh LFkkuh; fudk; foHkkx vf/klwpuk fnukad 12 tqykbZ] 2021 la[;k lh-lh-ih- ¼,u-lh-vkj-½@Mh-Mh-ih-&2041@mpkuk@2021@1039-& gfj;k.kk uxjikfydk vf/kfu;e] 1973] ¼1973 dk 24½ dh /kkjk 203 x dh mi&/kkjk ¼5½ rFkk gfj;k.kk vuqlwfpr lM+d rFkk fu;fU=r {ks= vfu;fer fodkl fucZUèku vfèkfu;e] 1963 ¼1963 dk iatkc vfèkfu;e 41½] dh èkkjk 5 dh mi&èkkjk ¼4½ }kjk iznÙk 'kfDr;ksa dk iz;ksx djrs gq,] gfj;k.kk ds jkT;iky] blds }kjk] vuwca/k ^[k^ esa fofufnZ"V fu;fU=r {ks=ksa dks ykxw fd, tkus okys izzLrkfor vkSj vuqca/k d rFkk [k esa fn, x, fucZU/kuksa rFkk 'krkZsa lfgr fu;fU=r {ks= mpkuk ftyk than ds fy, fuEufyf[kr izk:i fodkl ;kstuk] 2041 bZLoh izdkf'kr djrs gSaaA blds }kjk] uksfVl fn;k tkrk gS fd izk:i ;kstuk ds jkti= esa izdk'ku dh frfFk ls rhl fnu dh vof/k dh lekfIr ij vFkok blds i'pkr~ ljdkj] izk:i ij] ,sls vk{ksiks rFkk lq>kokas] ;fn dksbZ gksa] lfgr tks funs'kd] 'kgjh LFkkuh; fudk; foHkkx] gfj;k.kk] ,l-lh-vks- la[;k 11&14] lsDVj 4] iapdwyk] ¼uxjikfydk dh lhekvksa ds Hkhrj iM+us okys {ks= ds fy,½ rFkk funs'kd] uxj rFkk xzke vk;kstuk foHkkx] gfj;k.kk] eq[; la;kstd ;kstukdkj ¼,u-lh-vkj-½] IykWV la[;k 3] lsDVj 18 ,] e/;ekxZ] paMhx<+ ¼uxjikfydk dh lhekvksa ds ckgj iM+us okys {ks= ds fy,½ dks fdlh O;fDr ls fyf[kr esa izk:i fodkl ;kstuk ds laca/k esa bl izdkj fofufnZ"V vof/k dh lekfIr ls iwoZ izkIr fd;s tk,a] ij fopkj djsxhA MªªkbZax 1- fo|eku Hkwfe mi;ksx -

RAPID ASSESSMENT Facility Readiness for Essential Newborn Care & Resuscitation (ENC/R)
P a g e | 1 RAPID ASSESSMENT Facility Readiness for Essential Newborn Care & Resuscitation (ENC/R) 13th to 18th May, 2013 District Jind Child Health Division, NRHM Haryana in technical collaboration with Objectives: 1. Qualitative and quantitative assessment of readiness of health facilities in district Jind for essential newborn care and resuscitation. 2. To assess the quality of essential newborn care provided to each and every neonate immediately after birth. 3. To understand the existing knowledge, skills, attitudes and practices of the health service providers. 4. On job trainings to the service providers on novelties in essential newborn care and resuscitation. Materials and Methods 1. A structured and tested assessment tool has been used to assess the facilities on 8 parameters viz. facility identification and infrastructure, availability of services, human resource, Equipment and supplies, Register and client case records, protocols and guidelines, individual case records, and knowledge and practices. 2. Knowledge and skill assessment has been done on the newborn simulators (mannequins). 3. The current and ideal practices in essential newborn care and resuscitation have been demonstrated to the service providers on the mannequins. A team of Consultants and Interns visited 36 facilities in the district, from 13th May, 2013 to 18th May, 2013, including General Hospital, Sub-District Hospital, all CHCs and PHCs and the delivery huts with monthly delivery load of 3 or more. Following is the list of facilities visited: Sr. No. Name of Facility 1. GH Jind 2. SDH Narwana 3. CHC Julana 4. CHC Kalwa 5. CHC Kandela 6. CHC Kharak Ramji 7. CHC Safidon 8. -

M/S B.R. Spintex P. Ltd. Patiala Road, Nawana Jind 320, 350 670 1000
Name of the CPP Installed capacity Total T/F capacity Total KVA KVA Sr. No. M/s B.R. Spintex P. Ltd. Patiala Road, 320, 1000 1000 670 1 nawana Jind 350 M/s Jind Textile Ltd. V. Baroda Uchana 2x380 1000 1000 900 2 1x140 M/s Haryana Agro Cattle Feed Plant Near 250 300 300 250 3 Rly. Station, Jind M/s Jind Institute of Eng.. Tech. Panipat 125, 82.5 250 250 207 4 Road, Jind Ms Haaryana Oil Soya ltd. Jhanjkala, th 5 K.M. Narwana Road, Jind M/s Reliacne Infocom Ltd. Plot No. 40 2x30 125 125 60 6 HSIDC, Jind M/s Kisan Breeding Farms V. Ganguli 2X125 500 500 250 7 Jind M/s Hanuman Rice Mill, Dhanori, 2x82.5 200 200 164.5 8 Narwana M/s Arihant Super Rice Mill, Matt Road, 315 315 9 Safidon, Jind Mor Forms P. Ltd. Vill. Ludana, 250 250 10 Pillukhera. 11 Shiv Oil Mill, Dhamatana Sahiv, Narwana 100 100 Dilbag Singh S/o Sh. Rai Singh milenion, 100 100 12 Kalanwali, Pillukhera Azad Singh C/o Shakti Hatcheries and 100 100 13 Pultary Farms Shanpur Jind. 14 Gopi Ram cotton mill pinjupur Kalayat 750 750 L M Industries Opp PNB Anaj Mandi 250 250 15 HSIDC Plot No 1 Narwana Jind A One Cottan Mill Pinjupura narwana 500 500 16 road Kalayat Chaudhary Enteprises Meham Road, 200 200 17 Julana Jind Sh. Subhash Sheoran Indus Public School 100 100 18 Jind Ganga Putra H ospital Research Centre, 400 400 6th K.M. Stone Chandigarh Road, Kandela 19 Dev Raj S/o Lakhmi Chand, HSIDC, 160 160 20 Narwana 21 Sampurana Feed, V.p.o.