The Prostate
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Normal 3T MR Anatomy of the Prostate Gland and Surrounding Structures
Hindawi Advances in Medicine Volume 2019, Article ID 3040859, 9 pages https://doi.org/10.1155/2019/3040859 Review Article Normal 3T MR Anatomy of the Prostate Gland and Surrounding Structures K. Sklinda ,1 M. Fra˛czek,2 B. Mruk,1 and J. Walecki1 1MD PhD, Dpt. of Radiology, Medical Center of Postgraduate Education, CSK MSWiA, Woloska 137, 02-507 Warsaw, Poland 2MD, Dpt. of Radiology, Medical Center of Postgraduate Education, CSK MSWiA, Woloska 137, 02-507 Warsaw, Poland Correspondence should be addressed to K. Sklinda; [email protected] Received 24 September 2018; Accepted 17 December 2018; Published 28 May 2019 Academic Editor: Fakhrul Islam Copyright © 2019 K. Sklinda et al. +is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Development on new fast MRI scanners resulted in rising number of prostate examinations. High-spatial resolution of MRI examinations performed on 3T scanners allows recognition of very fine anatomical structures previously not demarcated on performed scans. We present current status of MR imaging in the context of recognition of most important anatomical structures. 1. Introduction also briefly present benign prostate hypertrophy (BPH) which is the most common condition of the prostate, oc- Aging of the society together with growing consciousness of curring in most patients over 50 years of age. the role of early detection of oncologic diseases leads to globally occurring rise in number of detected cases of 2. Imaging Protocol prostate cancer. Widely used transrectal sonography of the prostate gland despite additional support of contrast media According to PI-RADS v2, T1W and T2W sequences should and elastography does not provide sufficient sensitivity or be obtained for all prostate mpMR exams [1]. -

8508-Rectal-Cancer-In-The-Eye-A-Case-Report-Of-Orbital-Metastasis.Pdf
Open Access Case Report DOI: 10.7759/cureus.1589 Rectal Cancer in the Eye: A Case Report of Orbital Metastasis Mohammed Nabeel 1 , Rehan Farooqi 1 , Mahsa Mohebtash 2 , Rupak Desai 3 , Uvesh Mansuri 4 , Smit Patel 5 , Jinal Patel 6 , Vinshi Naz Khan 1 1. Department of Internal Medicine, Medstar Union Memorial Hospital 2. Chief of Medical Oncology and Hematology, Medstar Union Memorial Hospital 3. Research Coordinator, Atlanta Veterans Affairs Medical Center 4. Public Health, Icahn School of Medicine at Mount Sinai 5. Department of Neurology, University of Connecticut Health Center 6. Department of Internal Medicine, Winthrop University Hospital Corresponding author: Rupak Desai, [email protected] Abstract Orbital metastasis from colorectal cancer is extremely rare. In this case report, we describe a 48-year-old woman who presented with recurrent severe headaches and new onset constipation with no known history of cancer. After vigilant workup, imaging, and biopsies, she was diagnosed with orbital metastasis from a primary rectal carcinoma. She was started on chemotherapy and radiation therapy. Her chemotherapy regimen consisted of FLOX (leucovorin + fluorouracil + oxaliplatin), along with panitumumab, which she tolerated well. She received chemotherapy for seven months before she lost her battle with cancer. Categories: Internal Medicine, Gastroenterology, Oncology Keywords: rectal cancer, metastasis, chemotherapy, radiation therapy, orbit Introduction Colorectal cancer (CRC) is the second leading cause of cancer-related deaths in the United States in males and females combined [1]. Around 20% of patients with CRC have distant metastases at the time of diagnosis with an involvement of the liver, lungs, peritoneum, or bone [2-4]. Orbital metastasis from colorectal cancer is rare with only a handful of cases in the literature [5]. -

Mvdr. Natália Hvizdošová, Phd. Mudr. Zuzana Kováčová
MVDr. Natália Hvizdošová, PhD. MUDr. Zuzana Kováčová ABDOMEN Borders outer: xiphoid process, costal arch, Th12 iliac crest, anterior superior iliac spine (ASIS), inguinal lig., mons pubis internal: diaphragm (on the right side extends to the 4th intercostal space, on the left side extends to the 5th intercostal space) plane through terminal line Abdominal regions superior - epigastrium (regions: epigastric, hypochondriac left and right) middle - mesogastrium (regions: umbilical, lateral left and right) inferior - hypogastrium (regions: pubic, inguinal left and right) ABDOMINAL WALL Orientation lines xiphisternal line – Th8 subcostal line – L3 bispinal line (transtubercular) – L5 Clinically important lines transpyloric line – L1 (pylorus, duodenal bulb, fundus of gallbladder, superior mesenteric a., cisterna chyli, hilum of kidney, lower border of spinal cord) transumbilical line – L4 Bones Lumbar vertebrae (5): body vertebral arch – lamina of arch, pedicle of arch, superior and inferior vertebral notch – intervertebral foramen vertebral foramen spinous process superior articular process – mammillary process inferior articular process costal process – accessory process Sacrum base of sacrum – promontory, superior articular process lateral part – wing, auricular surface, sacral tuberosity pelvic surface – transverse lines (ridges), anterior sacral foramina dorsal surface – median, intermediate, lateral sacral crest, posterior sacral foramina, sacral horn, sacral canal, sacral hiatus apex of the sacrum Coccyx coccygeal horn Layers of the abdominal wall 1. SKIN 2. SUBCUTANEOUS TISSUE + SUPERFICIAL FASCIAS + SUPRAFASCIAL STRUCTURES Superficial fascias: Camper´s fascia (fatty layer) – downward becomes dartos m. Scarpa´s fascia (membranous layer) – downward becomes superficial perineal fascia of Colles´) dartos m. + Colles´ fascia = tunica dartos Suprafascial structures: Arteries and veins: cutaneous brr. of posterior intercostal a. and v., and musculophrenic a. -

Genitalia Blood Supply to Internal Female Course
U4-Reproductive BS+NS DEC 2016 FNF, approved by: DR.manoj Blood supply to internal female genitalia: artery origin distribution Anastamoses? Course Sup. large branch: Medially in base of broad Yes, cranially with Internal iliac uterus, inf. Small ligament to junction between ovarian, caudally uterine artery branch: cervix+ sup. cervix and uterus, run above with vaginal Vagina ureter, ascend to anastamose Middle +inferior part Yes, ant+post azygos Descand to vagina after Uterine of vagina along with arteries of vagina branching at junction between Vaginal artery pudendal artery with uterine artery uterus + cervix Yes, with uterine Descend along post. abdominal artery (collateral Ovarian Abdominal wall, at pelvic prim cross Ovary+ uterine tube circulation between artery aorta external iliac> enter suspensory abdominal +pelvic ligament source) vein Drainage Anastamoses? Course Vaginal venous plexus>vaginal vein> anastamose with uterine venous plexus Yes, vaginal plexus with Sides of vagina Vaginal >uterovaginal venous plexus>uterine uterine plexus vein>internal iliac vein uterine venous plexus >uterovaginal Yes, vaginal plexus with Uterine venous plexus>uterine vein>internal iliac Pass in broad ligament uterine plexus vein Pampiniform plexus of veins>ovarian vein Plexus in broad ligament Ovarian Rt:IVC - , ovarian vein in suspensory ligament Lt:LRV Note: -tubal veins drain in ovarian veins+ uterovaginal venous plexus -uterine vessels pass in cardinal ligament 1 | P a g e U4-Reproductive BS+NS DEC 2016 FNF, approved by: DR.manoj Blood supply to external female genitalia: artery origin distribution Course Perineum Leave pelvis through greater sciatic foramen hook Internal Internal iliac artery +external around ischial spine then enter through lesser pudendal genitalia sciatic foramen. -

Gray's Anatomy Review
GRAY’S Anatomy Review This page intentionally left blank GRAY’S Anatomy Review Marios Loukas, MD, PhD Associate Professor Department of Anatomical Sciences St. George’s University School of Medicine Grenada, West Indies Gene L. Colborn, PhD Professor Emeritus of Anatomy and Surgery The Medical College of Georgia Augusta, Georgia Peter Abrahams, MBBS, FRCS(ED), FRCR, DO(Hon) Professor of Clinical Anatomy Medical Teaching Centre Institute of Clinical Education Warwick Medical School University of Warwick United Kingdom Stephen W. Carmichael, PhD, DSc Department of Anatomy Mayo Clinic Rochester, Minnesota With illustrations from Abrahams P, Boon J, Spratt J: McMinn’s Clinical Atlas of Human Anatomy, 6th edition. St. Louis: Elsevier, 2008 1600 John F. Kennedy Blvd. Ste 1800 Philadelphia, PA 19103-2899 GRAY’S ANATOMY REVIEW ISBN: 978-0-443-06938-3 International ISBN: 978-0-8089-2403-6 Copyright © 2010 by Churchill Livingstone, an imprint of Elsevier Inc. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without permission in writing from the publisher. Permissions may be sought directly from Elsevier’s Rights Department: phone: (ϩ1) 215 239 3804 (US) or (ϩ44) 1865 843830 (UK); fax: (ϩ44) 1865 853333; e-mail: [email protected] . You may also complete your request on-line via the Elsevier website at http://www.elsevier.com/permissions . Notice Knowledge and best practice in this fi eld are constantly changing. As new research and experience broaden our knowledge, changes in practice, treatment and drug therapy may become necessary or appropriate. -

Prostate 1 Prostate
Prostate 1 Prostate Prostate Male Anatomy Prostate with seminal vesicles and seminal ducts, viewed from in front and above. Latin prostata [1] Gray's subject #263 1251 Artery internal pudendal artery, inferior vesical artery, and middle rectal artery Vein prostatic venous plexus, pudendal plexus, vesicle plexus, internal iliac vein Nerve inferior hypogastric plexus Lymph external iliac lymph nodes, internal iliac lymph nodes, sacral lymph nodes Precursor Endodermic evaginations of the urethra [2] MeSH Prostate [3] Dorlands/Elsevier Prostate The prostate (from Greek προστάτης - prostates, literally "one who stands before", "protector", "guardian"[4] ) is a compound tubuloalveolar exocrine gland of the male reproductive system in most mammals unless they have it removed at birth.[5] [6] In 2002, female paraurethral glands, or Skene's glands, were officially renamed the female prostate by the Federative International Committee on Anatomical Terminology.[7] The prostate differs considerably among species anatomically, chemically, and physiologically. Prostate 2 Function The function of the prostate is to store and secrete a slightly alkaline fluid, milky or white in appearance,[8] that usually constitutes 20-30% of the volume of the semen along with spermatozoa and seminal vesicle fluid. The alkalinity of semen helps neutralize the acidity of the vaginal tract, prolonging the lifespan of sperm. The alkalinization of semen is primarily accomplished through secretion from the seminal vesicles.[9] The prostatic fluid is expelled in the first ejaculate fractions, together with most of the spermatozoa. In comparison with the few spermatozoa expelled together with mainly seminal vesicular fluid, those expelled in prostatic fluid have better motility, longer survival and better protection of the genetic material (DNA). -

Varicocele Is the Root Cause Of
Accepted: 22 January 2018 DOI: 10.1111/and.12992 ORIGINAL ARTICLE Varicocele is the root cause of BPH: Destruction of the valves in the spermatic veins produces elevated pressure which diverts undiluted testosterone directly from the testes to the prostate M. Goren1 | Y. Gat1,2 1Interventional Radiology, Laniado Hospital, Netanya, Israel Summary 2Department of Condensed Matter In varicocele, there is venous flow of free testosterone (FT) directly from the testes Physics, Sub Micron Research Weizmann into the prostate. Intraprostatic FT accelerates prostate cell production and prolongs Institute of Science, Rehovot, Israel cell lifespan, leading to the development of BPH. We show that in a large group of Correspondence patients presenting with BPH, bilateral varicocele is found in all patients. A total of Yigal Gat, Interventional Radiology, Laniado Hospital, Netanya, Israel. 901 patients being treated for BPH were evaluated for varicocele. Three diagnostic Email: [email protected] methods were used as follows: physical examination, colour flow Doppler ultrasound and contact liquid crystal thermography. Bilateral varicocele was found in all 901 patients by at least one of three diagnostic methods. Of those subsequently treated by sclerotherapy, prostate volume was reduced in more than 80%, with prostate symptoms improved. A straightforward pathophysiologic connection exists between bilateral varicocele and BPH. The failure of the one- way valves in the internal sper- matic veins leads to a cascade of phenomena that are unique to humans, a result of upright posture. The prostate is subjected to an anomalous venous supply of undi- luted, bioactive free testosterone. FT, the obligate control hormone of prostate cells, reaches the prostate directly via the venous drainage system in high concentrations, accelerating the rate of cell production and lengthening cell lifespan, resulting in BPH. -

Anatomy and Physiology Model Guide Book
Anatomy & Physiology Model Guide Book Last Updated: August 8, 2013 ii Table of Contents Tissues ........................................................................................................................................................... 7 The Bone (Somso QS 61) ........................................................................................................................... 7 Section of Skin (Somso KS 3 & KS4) .......................................................................................................... 8 Model of the Lymphatic System in the Human Body ............................................................................. 11 Bone Structure ........................................................................................................................................ 12 Skeletal System ........................................................................................................................................... 13 The Skull .................................................................................................................................................. 13 Artificial Exploded Human Skull (Somso QS 9)........................................................................................ 14 Skull ......................................................................................................................................................... 15 Auditory Ossicles .................................................................................................................................... -

Review Article Intramedullary Spinal Cord Metastasis from Renal Cell Carcinoma: a Systematic Review of the Literature
Hindawi BioMed Research International Volume 2018, Article ID 7485020, 7 pages https://doi.org/10.1155/2018/7485020 Review Article Intramedullary Spinal Cord Metastasis from Renal Cell Carcinoma: A Systematic Review of the Literature Yuxiang Weng, Renya Zhan, Jian Shen, Jianwei Pan, Hao Jiang, Kaiyuan Huang, Kangli Xu, and Hongguang Huang Department of Neurosurgery, Te First Afliated Hospital, School of Medicine, Zhejiang University, Hangzhou, China Correspondence should be addressed to Hongguang Huang; [email protected] Received 31 August 2018; Revised 28 October 2018; Accepted 28 November 2018; Published 16 December 2018 Guest Editor: Rong Xie Copyright © 2018 Yuxiang Weng et al. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Intramedullary spinal cord metastases from renal cell carcinomas (RCCs) are rare and can cause serious diagnostic and therapeutic dilemmas. Te related reports are very few. Tis review was aimed to perform an analysis of all reported cases with intramedullary spinal cord metastases from RCCs. In January 2018, we performed a literature search in PubMed database using a combination of the keywords “intramedullary spinal cord metastasis” and “renal cell carcinoma”. In addition, we present the clinical, neuroradiological, and histopathological fndings in our patient with an intramedullary metastasis from a RCC. 17 cases were generated in our research. Te mean interval from diagnosis of RCC to diagnosis of ISCM was 22 months. Te median survival of surgically treated patients was 8.6 months and 8 months in patients who underwent radical surgery. -
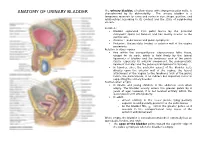
ANATOMY of URINARY BLADDER Characterized by Its Distensibility
The urinary bladder, a hollow viscus with strong muscular walls, is ANATOMY OF URINARY BLADDER characterized by its distensibility . The urinary bladder is a temporary reservoir for urine and varies in size, shape, position, and relationships according to its content and the state of neighboring viscera. Location : Bladder separated from pubic bones by the potential retropubic space (of Retzius) and lies mostly inferior to the peritoneum, Anterior : pubic bones and pubic symphysis Posterior : the prostate (males) or anterior wall of the vagina posteriorly Relation to other organs free within the extraperitoneal subcutaneous fatty tissue, except for its neck, which is held firmly by the lateral ligaments of bladder and the tendinous arch of the pelvic fascia—especially its anterior component, the puboprostatic ligament in males and the pubovesical ligament in females In females, since the posterior aspect of the bladder rests directly upon the anterior wall of the vagina, the lateral attachment of the vagina to the tendinous arch of the pelvic fascia, the paracolpium, is an indirect but important factor in supporting the urinary bladder Position when empty In infants and young children: in the abdomen even when empty. The bladder usually enters the greater pelvis by 6 years of age; however, it is not located entirely within the lesser pelvis until after puberty. In adult : o almost entirely in the lesser pelvis, lying partially superior to and partially posterior to the pubic bones o As the bladder fills, enters the greater pelvis as it ascends in the extraperitoneal fatty tissue of the anterior abdominal wall When empty, the bladder is somewhat tetrahedral externally has an apex,body, fundus, and neck. -

Orbital Metastasis from Rectal Adenocarcinoma- Report of a Rare Case
Case Report | Iran J Pathol. 2016; 11(5): 474-477: (Special Issue for Case Reports) Iranian Journal of Pathology | ISSN: 2345-3656 Orbital Metastasis from Rectal Adenocarcinoma- Report of a Rare Case Subrata Pal1*, Kingshuk Bose2, Abhishek Sharma1, Mrinal Sikdar3 1. Dept. of Pathology, College of Medicine and SagoreDutta Hospital, India 2. Dept. of Pathology, BankuraSammilani Medical College, India 3. Dept of Pathology, Kolkata National Medical College, India KEYWORDS ABSTRACT Orbital Metastasis Adenocarcinoma Colorectal carcinoma is a common malignancy in India as well as in world. Rectum Inspite of its high metastasizing ability to various organs and lymph node, orbital metastasis is exceptional. Very few cases have been reported in the world literature. Article Info We report orbital metastasis in a case of moderately differentiated rectal adenocarcinoma in a 58-year male patient from India in 2015. We want to focus on Received 18 Sep 2015; the rare metastatic pathway of rectal adenocarcinoma and early diagnosis of the Accepted 01 Dec 2016; orbital metastasis, which can help in application of therapy to save the eyesight. Published Online 02 Jan 2017; Corresponding Information: Dr Subrata Pal; Dept. of Pathology, College of Medicine and SagoreDutta Hospital, India, Tel: 9851773224, Email: [email protected] Copyright © 2017, IRANIAN JOURNAL OF PATHOLOGY. This is an open-access article distributed under the terms of the Creative Commons Attribution-noncommercial 4.0 International License which permits copy and redistribute the material just in noncommercial usages, provided the original work is properly cited. Introduction Colorectal carcinoma is a common malignancy for last two months. He had average built and had a in India as well as in the world (1). -

The Cerebrospinal Venous System: Anatomy, Physiology, and Clinical Implications Edward Tobinick, MD
5/8/2017 www.medscape.org/viewarticle/522597_print www.medscape.org The Cerebrospinal Venous System: Anatomy, Physiology, and Clinical Implications Edward Tobinick, MD Posted: 2/22/2006 Abstract and Introduction Abstract There is substantial anatomical and functional continuity between the veins, venous sinuses, and venous plexuses of the brain and the spine. The term "cerebrospinal venous system" (CSVS) is proposed to emphasize this continuity, which is further enhanced by the general lack of venous valves in this network. The first of the two main divisions of this system, the intracranial veins, includes the cortical veins, the dural sinuses, the cavernous sinuses, and the ophthalmic veins. The second main division, the vertebral venous system (VVS), includes the vertebral venous plexuses which course along the entire length of the spine. The intracranial veins richly anastomose with the VVS in the suboccipital region. Caudally, the CSVS freely communicates with the sacral and pelvic veins and the prostatic venous plexus. The CSVS constitutes a unique, largecapacity, valveless venous network in which flow is bidirectional. The CSVS plays important roles in the regulation of intracranial pressure with changes in posture, and in venous outflow from the brain. In addition, the CSVS provides a direct vascular route for the spread of tumor, infection, or emboli among its different components in either direction. Introduction "... we begin to wonder whether our conception of the circulation today is completely acceptable. As regards the venous part of the circulation, I believe our present conception is incorrect." Herlihy[1] "It seems incredible that a great functional complex of veins would escape recognition as a system until 1940..