Geographic Distribution of Leishmania Species in Ecuador Based on the Cytochrome B Gene Sequence Analysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

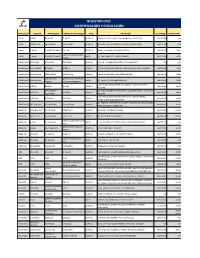
Turnos De Farmacia DICIEMBRE
TURNOS DE FARMACIA Coordinación Zonal 2 Turnos de farmacia DICIEMBRE PICHINCHA RURAL 2020 *RUMIÑAHUI* PROVINCIA Farmacia Ciudad Dirección Teléfono Fecha Inicio Fecha Final 06:00 AM 06:00 AM FARMACIA SANA SANA RUMIÑAHUI - AV GENERAL ENRIQUEZ, 023968500 05 DE DICIEMBRE 12 DE GENERAL ENRÍQUEZ SANGOLQUÍ S/N Y RIO CHINCHIPE. DE 2020 DICIEMBRE DE 2020 FARMACIA SELVA RUMIÑAHUI - CALLE FRANCISCO 0998391431 05 DE DICIEMBRE 12 DE ALEGRE SANGOLQUÍ GUARDERAS, DE 2020 DICIEMBRE DE CONJUNTO: ALCANTARA 2020 4L SELVA ALEGRE 19 DE FARMACIA PLUS RUMIÑAHUI - AV. MARIANA DE JESÚS 0992732231 12 DE DICIEMBRE DICIEMBRE DE SANGOLQUÍ N 644 Y VENEZUELA /022867882 DE 2020 2020 FARMACIA TU RUMIÑAHUI – CALLE GUARDERAS Y 022870671 12 DE DICIEMBRE 19 DE FARMACIA SALUD Y SANGOLQUI JUAN LARREA, N PB Y DE 2020 DICIEMBRE DE BIENESTAR FRANCISCO 2020 GUARDERAS AV GENERAL 022993100 / 26 DE FARMACIA ECONÓMICA RUMIÑAHUI – 19 DE DICIEMBRE RUMIÑAHUI, S/N E ISLA 0985442317 DICIEMBRE DE SAN RAFAEL SAN RAFAEL DE 2020 FLOREANA. 2020 FARMACIA CRUZ AZUL RUMIÑAHUI – AVENIDA GENERAL 022732632 / 26 DE UIO GENERAL ENRIQUEZ SAN RAFAEL ENRÍQUEZ, N/ 3333 E 0992803297 19 DE DICIEMBRE DICIEMBRE DE Y SANTIAGO ISLA SANTIAGO DE 2020 2020 FARMACIAS RUMIÑAHUI - CALLE MERCADO, N 27- 02331061 19 DE DICIEMBRE 26 DE COMUNITARIAS SANGOLQUÍ 35 Y MONTUFAR. DE 2020 DICIEMBRE DE SANGOLQUI 2020 FARMACIA SANTA AV. LOS SHIRIS, N 2-59 RUMIÑAHUI - 022551126 26 DE DICIEMBRE 02 DE ENERO DE MARTHA 280 Y AV. ABDON SANGOLQUÍ DE 2020 2021 CALDERON. FARMACIAS RUMIÑAHUI – AV GENERAL ENRIQUEZ 02 DE ENERO DE ECONOMICAS QUITO 022993100 26 DE DICIEMBRE SAN RAFAEL S/N E ISLA RABIDA. -

Pontificia Universidad Católica Del Ecuador
PONTIFICIA UNIVERSIDAD CATÓLICA DEL ECUADOR ESCUELA DE TRABAJO SOCIAL DISERTACIÓN PREVIA A LA OBTENCIÓN DEL TÍTULO DE “MAGÍSTER EN GESTIÓN DEL DESARROLLO LOCAL Y COMUNITARIO” “ALTERNATIVAS PARA LA REDUCCIÓN SOSTENIBLE DEL ENVEJECIMIENTO DE LA FUERZA PRODUCTIVA EN EL SECTOR AGROPECUARIO DEL CANTÓN PUERTO QUITO, PROVINCIA DE PICHINCHA” ING. LUIS FRANCISCO BRAVO SOLIS DIRECTORA: MGTR. MARÍA CECILIA PÉREZ QUITO - ECUADOR 2016 DECLARACIÓN DE AUTENTICIDAD Yo, Luis Francisco Bravo Solís, declaro en honor a la verdad, que la presente investigación es de total responsabilidad del autor y que se han respetado las diferentes fuentes de información. ____________________________ Luis Francisco Bravo Solís CI: 1712937299 I CERTIFICADO DE AUTORÍA Se autoriza utilizar los contenidos de esta investigación como referencia bibliográfica para fines académicos, por cualquier medio o procedimiento, siempre y cuando se cite como fuente de información al autor de la misma. Octubre de 2016 Nombre: Luis Francisco Bravo Solís Dirección: Portoviejo, Parroquia 12 de marzo, Avenida universitaria y Calle nueva. Email: [email protected] Teléfono: 0982342958 II CERTIFICACIÓN DEL DIRECTOR Mtr. María Cecilia Pérez DIRECTORA DEL PROYECTO DE GRADO CERTIFICA: Haber revisado el presente informe final de investigación, el mismo que se ajusta a las normas vigentes de la Escuela de Gestión Social, de la Pontificia Universidad Católica del Ecuador; cumpliendo los requisitos establecidos por la Dirección General Académica; en consecuencia está apta para su presentación y sustentación. -

Ecuador: Justice and Protection for Amazonian Women, Defenders Of
“THEY WILL NOT STOP US” Ecuador: Justice and protection for Amazonian Women, defenders of the land, territory and environment Amnesty International it’s a global movement of more than 7 million people working for respect and protection of human rights. Our vision is of a world in which all people enjoy the human rights set out in the las personas disfrutan de todos los derechos humanos Universal Declaration of Human Rights and other international standards. We are independent of any government, political ideology, economic interest or religious belief. Our work is funded primarily by contributions from our members and through donations. © Amnesty International 2019 Unless stated otherwise, the content of this document is protected by Creative Commons licence 4.0 (attribution, non-commercial, no derivative works, international). https://creativecommons.org/licenses/by-nc-nd/4.0/legalcode For more information, visit the Permissions page of our website: https://www.amnesty.org/es/about-us/permissions/. Material attributed to copyright holders other than Amnesty International is not subject to the Creative Commons licence. 2 THEY WILL NOT STOP US ECUADOR: JUSTICE AND PROTECTION FOR AMAZONIAN WOMEN, DEFENDERS OF THE LAND, TERRITORY AND ENVIRONMENT “THEY WILL NOT STOP US” ECUADOR: JUSTICE AND PROTECTION FOR AMAZONIAN WOMEN, DEFENDERS OF THE LAND, TERRITORY AND ENVIRONMENT AMNESTY INTERNATIONAL 3 INTRODUCTION Throughout 2018 in Ecuador, Amnesty International recorded a series of attacks and threats perpetrated against women human rights defenders and leaders Patricia Gualinga, Nema Grefa, Salomé Aranda and Margoth Escobar, members of Mujeres Amazónicas Defensoras de la Selva de las Bases frente al Extractivismo (Amazonian Women Defending the Forest from Extractivism), also known as the Mujeres Amazónicas (Amazonian Women) collective. -

ECUADOR Ecuador Is a Constitutional Republic with a Population Of
ECUADOR Ecuador is a constitutional republic with a population of approximately 14.3 million. In 2008 voters approved a referendum on a new constitution, which became effective in October of that year, although many of its provisions continued to be implemented. In April 2009 voters reelected Rafael Correa for his second presidential term and chose members of the National Assembly in elections that were considered generally free and fair. Security forces reported to civilian authorities. The following human rights problems continued: isolated unlawful killings and use of excessive force by security forces, sometimes with impunity; poor prison conditions; arbitrary arrest and detention; corruption and other abuses by security forces; a high number of pretrial detainees; and corruption and denial of due process within the judicial system. President Correa and his administration continued verbal and legal attacks against the independent media. Societal problems continued, including physical aggression against journalists; violence against women; discrimination against women, indigenous persons, Afro- Ecuadorians, and lesbians and gay men; trafficking in persons and sexual exploitation of minors; and child labor. RESPECT FOR HUMAN RIGHTS Section 1 Respect for the Integrity of the Person, Including Freedom From: a. Arbitrary or Unlawful Deprivation of Life The government or its agents did not commit any politically motivated killings; however, there continued to be credible reports that security forces used excessive force and committed isolated unlawful killings. On April 23, the government's Unit for the Fight against Organized Crime released a report exposing the existence of a gang of hit men composed of active-duty police. The report stated that police were part of a "social cleansing group" that killed delinquents in Quevedo, Los Rios Province. -

The Prevalence of Malnutrition in Ecuador 6
38689 Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized THE WORLDBANK Causes, Consequences, andSolutions Ecuador Nutritional Failure in A WORLD BANK COUNTRY STUDY BANK COUNTRY WORLD A A WORLD BANK COUNTRY STUDY Nutritional Failure in Ecuador Causes, Consequences, and Solutions THE WORLD BANK Washington, D.C. Copyright © 2007 The International Bank for Reconstruction and Development/The World Bank 1818 H Street, N.W. Washington, D.C. 20433, U.S.A. All rights reserved Manufactured in the United States of America First Printing: February 2007 printed on recycled paper 1 2 3 4 5 10 09 08 07 World Bank Country Studies are among the many reports originally prepared for internal use as part of the continuing analysis by the Bank of the economic and related conditions of its devel- oping member countries and to facilitate its dialogs with the governments. Some of the reports are published in this series with the least possible delay for the use of governments, and the aca- demic, business, financial, and development communities. The manuscript of this paper there- fore has not been prepared in accordance with the procedures appropriate to formally-edited texts. Some sources cited in this paper may be informal documents that are not readily available. The findings, interpretations, and conclusions expressed herein are those of the author(s) and do not necessarily reflect the views of the International Bank for Reconstruction and Development/The World Bank and its affiliated organizations, or those of the Executive Directors of The World Bank or the governments they represent. The World Bank does not guarantee the accuracy of the data included in this work. -
Registro Civil Identificación Y Cedulación
REGISTRO CIVIL IDENTIFICACIÓN Y CEDULACIÓN PROVINCIA CANTÓN PARROQUIA PUNTO DE ATENCIÓN TIPO DIRECCIÓN TELÉFONO EXTENSIÓN CARCHI ESPEJO EL ÁNGEL EL ANGEL AGENCIA ESMERALDAS Y SALINAS (GAD MUNICIPAL DE ESPEJO) 062977688 S/N CARCHI MONTUFAR SAN GABRIEL SAN GABRIEL AGENCIA BOLIVAR Y SALINAS (JUNTO A LA ESCUELA JOSE REYES) 062291767 S/N CARCHI TULCAN GONZÁLEZ SUÁREZ TULCAN AGENCIA BRASIL Y PANAMA ( VIA AEROPUERTO) 063731030 4001 HOSPITAL LUIS GUSTAVO CARCHI TULCAN GONZÁLEZ SUÁREZ ARCES AV. SAN FRANCISCO Y ADOLFO BEKER 062999400 4023 DAVILA ESMERALDAS ATACAMES ATACAMES ATACAMES AGENCIA CALLE D Y LA PRIMERA, SECTOR LOS ALMENDROS S/N S/N ESMERALDAS ELOY ALFARO BORBON BORBON AGENCIA JUNTA PARROQUIAL FRENTE AL PARQUE EN LA CALLE PRINCIPAL 063731040 8402 ESMERALDAS ESMERALDAS ESMERALDAS ESMERALDAS AGENCIA NUEVE DE OCTUBRE Y MALECÓN ESQUINA 063731040 8306 SIMON PLATA MATERNIDAD VIRGEN DE ESMERALDAS ESMERALDAS ARCES AV. LIBERTAD Y MANABÍ(PARADA 8) 063731040 8303 TORRES LA BUENA ESPERANZA CALLE ISIDRO AYORA ENTRE AV. MANABI Y SACOTO BOWEN, ESMERALDAS MUISNE MUISNE MUISNE AGENCIA 063731040 8401 ESQUINA ROSA ZARATE VIA GUALLABAMBA SECTOR NUEVO QUININDÉ BARRIO 3 DE MAYO ESMERALDAS QUININDE QUININDE AGENCIA 063731040 8407 (QUININDE) ESQUINA CALLE 5 DE AGOSTO ESQUINA FRENTE AL PARQUE CENTRAL, ESMERALDAS RIOVERDE RIOVERDE RIOVERDE AGENCIA 063731040 8422 JUNTO A UNA IGLESIA CATOLICA AV. ESMERALDAS ENTRE 29 DE ABRIL Y ARMADA NACIONAL BARRIO ESMERALDAS SAN LORENZO SAN LORENZO SAN LORENZO AGENCIA 063731040 8421 NUEVO HORIZONTEROBALINO IMBABURA ANTONIO ANTE -

The Burden of Cutaneous and Mucocutaneous Leishmaniasis in Ecuador
bioRxiv preprint doi: https://doi.org/10.1101/751446; this version posted August 29, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 The burden of cutaneous and mucocutaneous leishmaniasis in Ecuador 2 (2014-2018), a national registry-based study. 3 4 Aquiles R. Henríquez-Trujillo1¶*, Marco Coral-Almeida1¶, Manuel Calvopiña Hinojosa1¶. 5 1 One Health Research Group, Faculty of Health Sciences, Universidad de Las Américas, Quito, 6 Pichincha, Ecuador. 7 * Corresponding author: E-mail: [email protected] (ARHT). Address: One Health 8 Research Group, Faculty of Health Sciences, Universidad de Las Américas, Av. de los 9 Granados E12-41y Colimes, Quito EC170125, Ecuador. 10 ¶ These authors contributed equally to this work 11 12 Author's ORCID codes: 13 ARHT http://orcid.org/0000-0002-3094-4438 14 MCA http://orcid.org/0000-0003-0211-2906 15 MCH http://orcid.org/0000-0003-0093-7955 16 1 bioRxiv preprint doi: https://doi.org/10.1101/751446; this version posted August 29, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 17 Abstract 18 Background 19 Cutaneous (CL) and mucocutaneous (MCL) leishmaniasis remain as endemic tropical 20 diseases in several Latin American countries. This study aimed to estimate the burden of CL 21 and MCL in Ecuador for the period 2014-2018, in order to inform decision-making and resource 22 allocation to tackle this neglected disease. -

Rendición De Cuentas 2018
RENDICIÓN DE CUENTAS 2018 0 COMPETENCIAS Y FUNCIONES DEL GOBIERNO AUTÓNOMO DESCENTRALIZADO DE LA PROVINCIA DE PICHINCHA COMPETENCIA 1: Planificar el desarrollo provincial y formular los correspondientes planes de ordenamiento territorial, de manera articulada con la planificación nacional, regional, cantonal y parroquial. PROGRAMA: PLANIFICACIÓN DEL DESARROLLO PROVINCIAL INVERSIÓN COMPROMETIDA GADPP 2018: USD 122.414 1 Certificación ISO 37001 (Norma anti soborno) en ejecución, a ser aplicada en la Dirección de Gestión de Compras Públicas del GADPP. Funcionamiento y servicios del sistema de información territorial provincial 11 reportes realizados sobre la actualización de información cartográfica. 2.000 personas que acceden a la plataforma del visor geográfico. 6 reportes realizados en el repositorio digital. 2.655 documentos institucionales revisados y elevados al repositorio digital. Planificación del Desarrollo Territorial. 2 Agendas zonales realizadas: Sur, Equinoccial. Evaluación PDOT 2015-2019 Base de datos POAs 2006-2018 Implementación y funcionamiento del sistema de gestión por resultados (GPR). 283 proyectos a los que se realizó seguimiento. 28 POA´s aprobados e ingresados en el sistema. 12 reportes LOTAIP realizados. 1 documento de Rendición de Cuentas 2018. Provisión de información catastral. 3 catastros elaborados por Contribución Especial de Mejoras en las obras de construcción, ensanche, rehabilitación y mejoramiento de las vías de competencia exclusiva del Gobierno Provincial. 20 expropiaciones de obras solicitadas. Catastro actualizado de bienes institucionales. 1 10 informes, permutas, comodatos, donaciones, arrendamientos y peritajes elaborados. Unidad de Tierras 276 títulos de propiedad otorgados para la formalización de la tenencia de tierras en el sector rural, varias parroquias del Cantón Quito. 37 títulos de propiedad entregados en la Zona Centro. -

International Convention on the Elimination of All Forms of Racial Discrimination
United Nations CERD/C/ECU/25 International Convention on Distr.: General 5 August 2020 the Elimination of All Forms English of Racial Discrimination Original: Spanish English, French and Spanish only Committee on the Elimination of Racial Discrimination Twenty-fifth periodic report submitted by Ecuador under article 9 of the Convention, due in 2020*, ** [Date received: 30 December 2019] * The present document is being issued without formal editing. ** The annexes to the present report are available in the files of the secretariat. GE.20-10451 (E) 151020 201020 CERD/C/ECU/25 I. Introduction 1. Ecuador has been a party to the Convention since 22 September 1966. Under article 9 of the Convention, States parties are required to submit periodic reports on their compliance with their international obligations. Ecuador presented its combined twenty-third and twenty- fourth periodic reports to the Committee in 2017. 2. The present report sets out the country’s legislative framework and the current situation in the country in respect of this topic. It has been drafted in accordance with the relevant guidelines (CERD/C/2007/1). 3. The report was drawn up by the National Council for the Equality of Peoples and Nationalities in coordination with the Human Rights Secretariat and the Ministry of Foreign Affairs and Human Mobility. Contributions were also made by all the institutions with competencies in this area. 4. Ecuador demonstrated its commitment to progress in this area by extending invitations to visit the country to the Special Rapporteur on the rights of indigenous peoples, Victoria Tauli-Corpuz, whose visit took place between 19 and 29 November 2018, and to the Working Group of Experts on People of African Descent, whose visit took place between 16 and 20 December 2019. -

Sustainability Multivariate Analysis of the Energy Consumption of Ecuador Using Musiasem and BIPLOT Approach
Article Sustainability Multivariate Analysis of the Energy Consumption of Ecuador Using MuSIASEM and BIPLOT Approach Nathalia Tejedor-Flores 1,*, Purificación Vicente-Galindo 1,2 and Purificación Galindo-Villardón 1,2,3 1 Department of Statistics, University of Salamanca, 37008 Salamanca, Spain; [email protected] (P.V.-G.); [email protected] (P.G.-V.) 2 Instituto de Investigación Biomédica (IBSAL), 08028 Salamanca, Spain 3 Escuela Superior Politécnica del Litoral (ESPOL), Facultad de Ciencias de la Vida, 09-01-5863 Guayaquil, Ecuador * Correspondence: [email protected]; Tel.: +34-675-011-677 Academic Editor: Manfred Max Bergman Received: 26 April 2017; Accepted: 1 June 2017; Published: 7 June 2017 Abstract: Rapid economic growth, expanding populations and increasing prosperity are driving up demand for energy, water and food, especially in developing countries. To understand the energy consumption of a country, we used the Multi-Scale Integrated Analysis of Societal and Ecosystem Metabolism (MuSIASEM) approach. The MuSIASEM is an innovative approach to accounting that integrates quantitative information generated by distinct types of conventional models based on different dimensions and scales of analysis. The main objective of this work is to enrich the MuSIASEM approach with information from multivariate methods in order to improve the efficiency of existing models of sustainability. The Biplot method permits the joint plotting, in a reduced dimension of the rows (individuals) and columns (variables) of a multivariate data matrix. We found, in the case study of Ecuador, that the highest values of the Exosomatic Metabolic Rate (EMR) per economic sector and Economic Labor Productivity (ELP) are located in the Productive Sector (PS). -

Class and Ethnicity in the Canton of Cayambe: the Roots of Ecuador's Modern Indian Movement
Class and Ethnicity in the Canton of Cayambe: The Roots of Ecuador's Modern Indian Movement by Marc Becker B.A., Bethel College, 1985 M.A., University of Kansas, 1990 Submitted to the Department of History and the Faculty of the Graduate School of the University of Kansas in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Chair) (Committee Members) Date Defended: Abstract Marc Becker, Ph.D. Department of History, 1997 University of Kansas My research examines changes in ideologies of class and ethnicity within rural movements for social change in Ecuador during the twentieth century. It explores how popular organizations engaged class analyses and ethnic identities in order to influence strategies of political mobilization among Indigenous and peasant peoples. Although recently ethnicity has come to dominate Indigenous political discourse, I have discovered that historically the rural masses defended their class interests, especially those related to material concerns such as land, wages, and work, even while embracing an ideology of ethnicity. Through the study of land tenure and political mobilization issues, this project examines the roles of leadership, institutions, economics, and class relations in order to understand the formation of class ideologies and ethnic politics in Ecuador. Although various Indigenous revolts occurred during the colonial period, these were localized and lacked a global vision for social change. In contrast, beginning in the 1920s Indian organizations emerged which understood that immediate and local solutions would not improve their situation, but rather that there must be fundamental structural changes in society. Moving from narrow, local revolts to broad organiza- tional efforts for structural change represented a profound ideological shift which marks the birth of Ecuador's modern Indian movement. -

Pomacea Canaliculata in Ecuador: a Recent Pest with Multiple Implications
Pomacea canaliculata in Ecuador: a recent pest with multiple implications Modesto Correoso Rodriguez1, Esteban Espinosa2, Marcela Coello Rodriguez 3 1 Department of Earth Sciences, Geographical and Environmental Engineering. University of the Army-ESPE. Avenida El Progreso, s / n. Sangolquí, Ecuador. Email: [email protected], [email protected] 2 Animal and Plant Health Inspection Service, United States Department of Agriculture,American Embassy, Calle Avigiras E12-170 y Avenida Eloy Alfaro, Quito, Ecuador. Email: [email protected] 5 Faculty of Biological Sciences, Central University of Ecuador, Quito. Email: [email protected] Abstract This article characterises and analyses the presence of the alien invasive species Pomacea canaliculata in Ecuador, a pest present in many countries that has severe impacts on agriculture, human health and the natural environment. For the first time, a list of the native species of the genus Pomacea in Ecuador is provided, as well as an occurrence map, based on review of existing (but few) bibliographic data, museum collections and recent field work. There is a lack of information on other mollusc species in Ecuador, but there is the potential for ecological impact of P. canaliculata on the native mollusc fauna, especially other Pomacea species, which may already be in decline. Other biological threats and consequences are considered, highlighting the impacts that the invasion has had in this Andean country. Also, events that have occurred since the detection of the pest are reviewed, in particular, the decisions adopted by the rice agricultural sector in comparison with those reported by other countries facing a similar situation. The epidemiological role of P.