Plant Medicines for Clinical Trial
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Additional Land South of the Gas Treatment Plant Vegetation and Flora Survey
Additional Land South of the Gas Treatment Plant Vegetation and Flora Survey October 2013 Prepared for Chevron Australia Pty Ltd Astron Environmental Services 129 Royal Street East Perth WA 6004 Phone: (08) 9421 9600 Fax: (08) 9421 9699 Report Reference: 2609-13-BSR-1Rev0_131128 Email: [email protected] Doc. ID: G1-NT-REP00000220 Doc. ID: G1-NT-REP00000220 Additional Land South of the Gas Treatment Plant Vegetation and Flora Survey Prepared for Chevron Australia Pty Ltd Job Number: 2609-13 Reference: 2609-13-BSR-1Rev0_131128 Revision Status Rev Date Description Author(s) Reviewer A 01/11/2013 Draft Issued for Client Review N. Cadd J. Kruger B 08/11/2013 Revised Draft Issued for Client Review N. Cadd J. Kruger C 12/11/2013 Revised Draft Issued for Client Review N. Cadd V. Clarke 0 28/11/2013 Final Issued for Information N. Cadd V. Clarke Approval Rev Date Issued to Authorised by Name Signature A 01/11/2013 A. Smith/S. Finn S. Pearse B 08/11/2013 A. Smith/S. Finn S. Pearse C 12/11/2013 A. Smith/S. Finn S. Atkinson 0 28/11/2013 A. Smith/S. Finn S. Pearse © Copyright 2012 Astron Environmental Services Pty Ltd. All rights reserved. This document and information contained in it has been prepared by Astron Environmental Services under the terms and conditions of its Doc.contract ID: with G1-NT-REP00000220 its client. The report is for the clients use only and may not be used, exploited, copied, duplicated or reproduced in any form or medium whatsoever without the prior written permission of Astron Environmental Services or its client. -

Toxic Effects of Root Extract of Calotropis Gigantea Linn
Journal of Pharmaceutical Research And Opinion 1:3 (2011) 92 – 93 Contents lists available at www.innovativejournal.in JOURNAL OF PHARMACEUTICAL RESEARCH AND OPINION Journal homepage: http://www.innovativejournal.in/index.php/jpro RESEARCH EVALUATION OF ANTIFERTILITY POTENTIAL OF CALOTROPIS GIGANTEA LINN. IN FEMALE ALBINO RATS. M. Mishra 1, R. K Gautam2, R. Mathur3* 1School of Zoology and Anthropology, Opp. GDA, Gwalior. Madhya Pradesh, India. 2School of Life sciences, Khandari campus, Agra Univerisity, Agra, Uttar Pradesh. India. 3School of Studies in Zoology, Jiwaji University, Gwalior, Madhya Pradesh, India. ARTICLE INFO ABSTRACT Received 22 July 2011 The present study has been undertaken to evaluate antifertility and ovaro-uterotoxic Accepted 28 July 2011 activities of the extracts of Calotropis gigantea Linn. Animals studied were divided Corresponding Author: into various groups control and experimental groups. Crude and ethanolic extracts R.Mathur were prepared and 150 and 300 mg/kg body weight doses were selected. [email protected] Oestrogenicity/antioestrogenicity was tested by using bilaterally ovariectomized School of Studies in Zoology, immature rats. Biochemical parameters viz. uterine glycogen, total protein, acid and Jiwaji University, Gwalior, alkaline phosphatase were measured and compared with control and vehicle. The Madhya Pradesh, India. findings suggest that the extracts are strong antiestrogenic and antiprogestagenic. Sharp decline was found in uterine glycogen, total proteins and acid phosphatase level whereas the level of alkaline phosphatase was found to increase. Though the KeyWords: Antifertility, extracts are highly toxic at higher doses yet they exhibit potential to be elucidated as Calotropin, Endometrium, female antifertility agents with proper control of toxicity. Hyaluronic acid ©2011, JPRO, All Right Reserved. -

The Utilization of Various Asclepias Species by Larvae of the Monarch Butterfly, Danaus Plexippus by James M
THE UTILIZATION OF VARIOUS ASCLEPIAS SPECIES BY LARVAE OF THE MONARCH BUTTERFLY, DANAUS PLEXIPPUS BY JAMES M. ERICKSON* Dept. o Entomology, Cornell University Ithaca, New York, 485o INTRODUCTION Plants of the genus Asclepias are well known to. contain high concentrations o cardiac glycosides (cardenolides). It is generally surmised that such cardiac stimulants unctio,n to, protect plants containing th,em against insect and vertebrate herbivores (Euw et al. 967). In addition, some insects w,hich are adapted to. eed on Asclepias plants store cardiac glyco,sides apparently as a means o. protection against vertebrate predat.ors which ind he compounds distasteful (Brower and Brower 964, Brower 969). It was by means of such an herbivore-predato,r interaction, bluejays eeding on monarch butterflies, Danaus plexippus L. (Brower 969, Brower et al. 968), that a spectrum o.f palatability was detected among monarch butterflies reared on various species ,o milkw.eed. It is surmised that this spectrum of toxicity to a vertebrate predator reflects a spectrum of concentrations o cardiac glycosides in the different species o the insects' larval ood plants (Brower and Brower 964, Brower et al. 967, Brower 1969). However, quantitative and qualitative data ,or cardenolides in Asclepias leaves, are at best in- complete (Reynard and Morton 942, Kupchan et al. 964, Duffey 97o, Singh and Rastogi 97o, Feir and Suen 97, Duffey and Scudder 972, Scudder and Duffey 972, and Eggermann and Bongers 972). The following experiments were undertaken to determine whether a dierential response by D. plexippus larvae to their host plants could be detected by measuring their efficiency o ood utiliza- tion and whether such a response would support the concept o a spectrum o toxicity. -

Biosystematic Studies in Heliotropium Indicum, Trichodesma Indicum and T
Int.J.Curr.Microbiol.App.Sci (2016) 5(4): 720-729 International Journal of Current Microbiology and Applied Sciences ISSN: 2319-7706 Volume 5 Number 4 (2016) pp. 720-729 Journal homepage: http://www.ijcmas.com Original Research Article http://dx.doi.org/10.20546/ijcmas.2016.504.083 Biosystematic Studies in Heliotropium indicum, Trichodesma indicum and T. zeylanicum of Boraginaceae Ashwini Kumar1 and Baidyanath Kumar2* 1PG Dept. of Botany, Gaya College, Gaya, India 2PG Department of Biotechnology, College of Commerce, Patna, Magadh University, India *Corresponding author ABSTRACT In the present observation biosystematics of three species of Boraginaceae viz., of Heliotropium indicum, Trichodesma indicum and Trichodesma zeylanicum was K eywo rd s studied. All the three species showed a marked difference in leaf and inflorescence Biosystematics, morphology, stomatal behaviour, epidermal trichome, pollen grain characteristics Heliotropium and stem anatomy, hypodromous and brochidodromous venation of their leaves. indicum. Leaves were landeolate to ovate. The inflorescence colour was pale blue to white. Trichodesma Length of inflorescence was found to be 4.0 to 6.5. The stomatal Index in these indicum, three species varied greatly. T. indicum and T. zeylanicum showed anomocytic Trichodesma stomata with 16mm in length and 12mm width and Stomatal Index was 34.88 and zeylanicum , 44.68 respectively. Heliotropium indicum exhibited anisocytic stomata which were Numerical analysis. 12mm long and 10mm wide. The Stomatal Index was 32.65. All the three species showed the presence of unicellular glandular hairs which differed in forms. All the three species showed tricolpate pollen grains, but differed in their form and size. Article Info All the three species showed more or less similar stem anatomical features with differences only in their hypodermal layers. -
I PHASE-TRAFFICKING METHODS in NATURAL
PHASE-TRAFFICKING METHODS IN NATURAL PRODUCTS, MODULATORS OF ORGANIC ANION TRANSPORTING POLYPEPTIDES FROM ROLLINIA EMARGINATA, AND PREGNANE AND CARDIAC GLYCOSIDES FROM ASCLEPIAS SPP. BY ©2012 JUAN JOSE ARAYA BARRANTES Submitted to the graduate degree program in Medicinal Chemistry and the Graduate Faculty of the University of Kansas in partial fulfillment of the requirements for the degree of Doctor of Philosophy. ________________________________ Chair ________________________________ ________________________________ ________________________________ ________________________________ Committee members Date Defended: ________________________________ i The Dissertation Committee for Juan Jose Araya Barrantes certifies that this is the approved version of the following dissertation: PHASE-TRAFFICKING METHODS IN NATURAL PRODUCTS, MODULATORS OF ORGANIC ANION TRANSPORTING POLYPEPTIDES FROM ROLLINIA EMARGINATA, AND PREGNANE AND CARDIAC GLYCOSIDES FROM ASCLEPIAS SPP. ________________________________ Chair ________________________________ ________________________________ ________________________________ ________________________________ Committee members Date approved:_______________________ ii ABSTRACT Phase-Trafficking Methods in Natural Products, Modulators of Organic Anion Transporting Polypeptides from Rollinia emarginata, and Pregnane and Cardiac Glycosides from Asclepias spp. Juan J. Araya Barrantes, Ph. D. The University of Kansas, 2012 For decades, chemists and medicinal chemists have found in nature the source of inspiration for drug discovery -
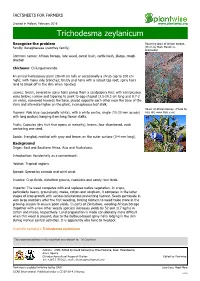
Trichodesma Zeylanicum
FACTSHEETS FOR FARMERS Created in Malawi, February 2016 www.plantwise.org Trichodesma zeylanicum Recognize the problem Flowering plant of African borage. Family: Boraginaceae (comfrey family) (Photo by Mark Marathon, Wikimedia) Common names: African borage, late weed, camel bush, cattle bush, jilarga, rough bluebell Chichewa: Chilungumwamba An annual herbaceous plant (30-40 cm tall) or occasionally a shrub (up to 100 cm high); with many side branches; bristly and hairy with a robust tap root; spiny hairs tend to break off in the skin when handled. Leaves: Green, covered in spiny hairs giving them a sandpapery feel; with conspicuous veins below; narrow and tapering to point to egg-shaped (3.5-10.5 cm long and 0.7-2 cm wide), narrowed towards the base, placed opposite each other near the base of the stem and alternate higher on the plant, inconspicuous leaf stalk. Flower of African borage. (Photo by Flowers: Pale blue (occasionally white), with a white centre, single (15-20 mm across) Pete Hill, www.flickr.com) with long pedicel, hanging from long flower stalks. Fruits: Capsules (dry fruit that opens at maturity), brown, four chambered, each containing one seed. Seeds: 3-angled, mottled with grey and brown on the outer surface (3-4 mm long). Background Origin: East and Southern Africa, Asia and Australasia. Introduction: Accidentally as a contaminant. Habitat: Tropical regions. Spread: Spread by animals and whirl wind. Invades: Crop fields, disturbed ground, roadsides and sandy river beds. Impacts: The weed competes with and replaces native vegetation. In crops, particularly beans, groundnuts, maize, cotton and sorghum, it competes in the latter stages of crop growth with serious infestations preventing harvest. -
Palatability of Plants to Camels (DBIRD NT)
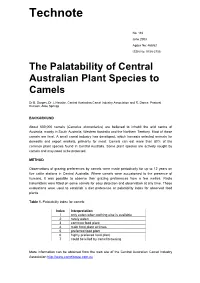
Technote No. 116 June 2003 Agdex No: 468/62 ISSN No: 0158-2755 The Palatability of Central Australian Plant Species to Camels Dr B. Dorges, Dr J. Heucke, Central Australian Camel Industry Association and R. Dance, Pastoral Division, Alice Springs BACKGROUND About 600,000 camels (Camelus dromedarius) are believed to inhabit the arid centre of Australia, mainly in South Australia, Western Australia and the Northern Territory. Most of these camels are feral. A small camel industry has developed, which harvests selected animals for domestic and export markets, primarily for meat. Camels can eat more than 80% of the common plant species found in Central Australia. Some plant species are actively sought by camels and may need to be protected. METHOD Observations of grazing preferences by camels were made periodically for up to 12 years on five cattle stations in Central Australia. Where camels were accustomed to the presence of humans, it was possible to observe their grazing preferences from a few metres. Radio transmitters were fitted on some camels for easy detection and observation at any time. These evaluations were used to establish a diet preference or palatability index for observed food plants. Table 1. Palatability index for camels Index Interpretation 1 only eaten when nothing else is available 2 rarely eaten 3 common food plant 4 main food plant at times 5 preferred food plant 6 highly preferred food plant 7 could be killed by camel browsing More information can be obtained from the web site of the Central Australian Camel Industry Association http://www.camelsaust.com.au 2 RESULTS Table 2. -

Pyrrolizidine Alkaloids in Plants Used in the Traditional Medicine of Madagascar and the Mascarene Islands
REVIEW Pharmazeutisches Institut der Rheinischen Friedrich-Wilhelms-Universität, Bonn, Germany Pyrrolizidine alkaloids in plants used in the traditional medicine of Madagascar and the Mascarene islands E. Roeder, H. Wiedenfeld Received April 26, 2011, accepted May 20, 2011 Prof. Dr.Dr.h.c. Erhard Roeder,Dr.Helmut Wiedenfeld, Pharmazeutisches Institut der Universität, An der Immenburg 4, D-53121 Bonn, Germany [email protected], [email protected] Dedicated to Prof. Dr. med. Dr. rer. nat. Drs. h.c. Ernst Mutschler on the occasion of his 80th birthday Pharmazie 66: 637–647 (2011) doi: 10.1691/ph.2011.1572 Pyrrolizidine alkaloids (PAs) can be hazardous to the health of humans and animals. Although their toxicity has been known for a long time, PA containing plants are still in use in many traditional medicines. Traditional healing systems have become of increasing interest as many people believe that they can be used without any risk and side effects. This also applies to the traditional medicine of Madagascar and the Mascarene island (Mauritius, Réunion, Rodriguez). Recent literature reports have recommended this traditional medicine because of its good efficacy and pharmacological properties. However, several plants are listed there which have already been described to contain toxic PAs or are suspected of containing them. 1. Introduction play a growing role in the treatment of diseases in the form of self-medication. Pyrrolizidine alkaloids (PAs)are naturally occurring compounds In addition, increased tourism has made it possible that people which are contained in about 3% of all flowering plants (Bull come into contact with different traditional healing systems all et al. -

Organic & Biomolecular Chemistry
Organic & Biomolecular Chemistry Accepted Manuscript This is an Accepted Manuscript, which has been through the Royal Society of Chemistry peer review process and has been accepted for publication. Accepted Manuscripts are published online shortly after acceptance, before technical editing, formatting and proof reading. Using this free service, authors can make their results available to the community, in citable form, before we publish the edited article. We will replace this Accepted Manuscript with the edited and formatted Advance Article as soon as it is available. You can find more information about Accepted Manuscripts in the Information for Authors. Please note that technical editing may introduce minor changes to the text and/or graphics, which may alter content. The journal’s standard Terms & Conditions and the Ethical guidelines still apply. In no event shall the Royal Society of Chemistry be held responsible for any errors or omissions in this Accepted Manuscript or any consequences arising from the use of any information it contains. www.rsc.org/obc Page 1 of 10Organic & BiomolecularOrganic & Biomolecular Chemistry Dynamic Article Links ► Chemistry Cite this: DOI: 10.1039/c0xx00000x ARTICLE TYPE www.rsc.org/xxxxxx Structures, chemotaxonomic significance, cytotoxic and Na +,K +-ATPase inhibitory activities of new cardenolides from Asclepias curassavica Rong-Rong Zhang a, Hai-Yan Tian a, Ya-Fang Tan a, Tse-Yu Chung d, Xiao-Hui Sun a, Xue Xia a,Wen-Cai Yea, David A. Middleton b, Natalya Fedosova c, Mikael Esmann c* , Jason T.C. Tzen d* , Ren-Wang Jiang a* Manuscript 5 Received (in XXX, XXX) Xth XXXXXXXXX 20XX, Accepted Xth XXXXXXXXX 20XX DOI: 10.1039/b000000x Five new cardenolide lactates (1-5) and one new dioxane double linked cardenolide glycoside ( 17 ) along with 15 known compounds ( 6- 16 and 18 -21 ) were isolated from the ornamental milkweed Asclepias curassavica . -

Two Newly Naturalized Plants of the Boraginaceae in Taiwan: Trichodesma Indicum (L.) Lehm
Taiwan J For Sci 29(2): 149-56, 2014 149 Research note Two Newly Naturalized Plants of the Boraginaceae in Taiwan: Trichodesma indicum (L.) Lehm. and Trichodesma zeylanicum (Burm.f.) R. Br. Chiu-Mei Wang,1) Kun-Cheng Chang2,3) 【Summary】 Trichodesma indicum (L.) Lehm., an herb native to Asia and Africa, and Trichodesma zeylani- cum (Burm.f.) R. Br., one native to Africa, tropical Asia, and Australasia, were recently found in west-central Taiwan. Both species are considered to be newly naturalized. This report gives taxo- nomic descriptions, illustrations, and distribution maps. Photographs are also provided to help with identification. Key words: Trichodesma indicum, Trichodesma zeylanicum, Boraginaceae, naturalized plant, Tai- wan. Wang CM, Chang KC. 2014. Two newly naturalized plants of the Boraginaceae in Taiwan: Trichodesma indicum (L.) Lehm. and Trichodesma zeylanicum (Burm.f.) R. Br.. Taiwan J For Sci 29(2):149-56. 1) Department of Biology, National Museum of Natural Science, 1 Guancian Rd., Taichung 40453, Taiwan. 國立自然科學博物館生物學組,40453台中市館前路1號。 2) Department of Forestry and Natural Resources, National Chiayi Univ., 300 Xuefu Rd., Chiayi City 60004, Taiwan. 國立嘉義大學森林暨自然資源學系,60004嘉義市鹿寮里學府路300號。 3) Corresponding author, e-mail:[email protected] 通訊作者。 Received September 2013, Accepted February 2014. 2013年9月送審 2014年2月通過。 150 Wang and Chang─Newly naturalized plants of the Boraginaceae in Taiwan 研究簡報 兩種新歸化的紫草科植物: 印度碧果草及斯里蘭卡碧果草 王秋美1) 張坤城2,3) 摘要 原產於熱帶亞洲及非洲的印度碧果草與斯里蘭卡碧果草(亦見於澳洲)最近發現於臺灣中部。這兩 種紫草科植物,均為新近歸化於臺灣的外來種。本文提供此兩物種的分類特徵描述,手繪圖,以及在 臺灣的分布點以供區分鑑定。 關鍵詞:印度碧果草、斯里蘭卡碧果草、紫草科、歸化植物、臺灣。 王秋美、張坤城。2014。兩種新歸化的紫草科植物:印度碧果草及斯里蘭卡碧果草。台灣林業科學 29(2):149-56。 INTRODUCTION The Boraginaceae comprises about 156 lia (Weigend et al. 2013), and is characterized genera and 2500 species which are distrib- by the connective of the anthers prominently uted in temperate and tropical regions, and subulate and spirally twisted. -

Digitoxigenin (AMANTADIG) Affects G2/M Cell Cycle
www.impactjournals.com/oncotarget/ Oncotarget, 2017, Vol. 8, (No. 7), pp: 11676-11691 Research Paper A new semisynthetic cardenolide analog 3β-[2-(1-amantadine)- 1-on-ethylamine]-digitoxigenin (AMANTADIG) affects G2/M cell cycle arrest and miRNA expression profiles and enhances pro- apoptotic survivin-2B expression in renal cell carcinoma cell lines Elke Nolte1, Sven Wach1, Izabella Thais Silva2,6, Sabine Lukat1, Arif B. Ekici3, Jennifer Munkert4, Frieder Müller-Uri4, Wolfgang Kreis4, Cláudia Maria Oliveira Simões2, Julio Vera5, Bernd Wullich1, Helge Taubert1, Xin Lai5 1Department of Urology, University Hospital Erlangen, Erlangen, Germany 2Department of Pharmaceutical Sciences, Universidade Federal de Santa Catarina, Florianópolis, Brazil 3Institute of Human Genetics, Friedrich-Alexander-Universität Erlangen-Nürnberg, Erlangen, Germany 4Department of Biology, Chair of Pharmaceutical Biology, Friedrich-Alexander-University Erlangen-Nürnberg, Erlangen, Germany 5Laboratory of Systems Tumor Immunology, Department of Dermatology, University Hospital Erlangen, Friedrich-Alexander- University Erlangen-Nürnberg, Erlangen, Germany 6Department of Pharmacy, Federal University of Minas Gerais, Belo Horizonte, Brazil Correspondence to: Xin Lai, email: [email protected] Keywords: 3β-[2-(1-amantadine)-1-on-ethylamine]-digitoxigenin, cardiac glycoside analog, human renal cell carcinoma cells, miRNA, cell cycle Received: June 21, 2016 Accepted: December 24, 2016 Published: January 14, 2017 ABSTRACT Cardiac glycosides are well known in the treatment of cardiovascular diseases; however, their application as treatment option for cancer patients is under discussion. We showed that the cardiac glycoside digitoxin and its analog AMANTADIG can inhibit the growth of renal cell carcinoma (RCC) cell lines and increase G2/M cell cycle arrest. To identify the signaling pathways and molecular basis of this G2/M arrest, microRNAs were profiled using microRNA arrays. -

Relative Selectivity of Plant Cardenolides for Na+/K+-Atpases from the Monarch Butterfly and Non-Resistant Insects
fpls-09-01424 September 26, 2018 Time: 15:23 # 1 ORIGINAL RESEARCH published: 28 September 2018 doi: 10.3389/fpls.2018.01424 Relative Selectivity of Plant Cardenolides for NaC/KC-ATPases From the Monarch Butterfly and Non-resistant Insects Georg Petschenka1*, Colleen S. Fei2, Juan J. Araya3, Susanne Schröder4, Barbara N. Timmermann5 and Anurag A. Agrawal2 1 Institute for Insect Biotechnology, Justus-Liebig-Universität, Giessen, Germany, 2 Department of Ecology and Evolutionary Biology, Cornell University, Ithaca, NY, United States, 3 Centro de Investigaciones en Productos Naturales, Escuela de Química, Instituto de Investigaciones Farmacéuticas, Facultad de Farmacia, Universidad de Costa Rica, San Pedro, Costa Rica, 4 Institut für Medizinische Biochemie und Molekularbiologie, Universität Rostock, Rostock, Germany, 5 Department of Medicinal Chemistry, School of Pharmacy, University of Kansas, Lawrence, KS, United States A major prediction of coevolutionary theory is that plants may target particular herbivores with secondary compounds that are selectively defensive. The highly specialized Edited by: monarch butterfly (Danaus plexippus) copes well with cardiac glycosides (inhibitors Daniel Giddings Vassão, C C Max-Planck-Institut für chemische of animal Na /K -ATPases) from its milkweed host plants, but selective inhibition Ökologie, Germany of its NaC/KC-ATPase by different compounds has not been previously tested. Reviewed by: We applied 17 cardiac glycosides to the D. plexippus-NaC/KC-ATPase and to the Stephen Baillie Malcolm, C C Western Michigan University, more susceptible Na /K -ATPases of two non-adapted insects (Euploea core and United States Schistocerca gregaria). Structural features (e.g., sugar residues) predicted in vitro Supaart Sirikantaramas, inhibitory activity and comparison of insect NaC/KC-ATPases revealed that the monarch Chulalongkorn University, Thailand has evolved a highly resistant enzyme overall.