Inkjet Printing: an Emerging Technology for 3D Tissue Or Organ Printing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Metallizations by Direct-Write Inkjet Printing
October 2001 • NREL/CP-520-31020 Metallizations by Direct-Write Inkjet Printing Preprint C. Curtis, T. Rivkin, A. Miedaner, J. Alleman, J. Perkins, L. Smith, and D. Ginley To be presented at the NCPV Program Review Meeting Lakewood, Colorado 14-17 October 2001 National Renewable Energy Laboratory 1617 Cole Boulevard Golden, Colorado 80401-3393 NREL is a U.S. Department of Energy Laboratory Operated by Midwest Research Institute ••• Battelle ••• Bechtel Contract No. DE-AC36-99-GO10337 NOTICE The submitted manuscript has been offered by an employee of the Midwest Research Institute (MRI), a contractor of the US Government under Contract No. DE-AC36-99GO10337. Accordingly, the US Government and MRI retain a nonexclusive royalty-free license to publish or reproduce the published form of this contribution, or allow others to do so, for US Government purposes. This report was prepared as an account of work sponsored by an agency of the United States government. Neither the United States government nor any agency thereof, nor any of their employees, makes any warranty, express or implied, or assumes any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, apparatus, product, or process disclosed, or represents that its use would not infringe privately owned rights. Reference herein to any specific commercial product, process, or service by trade name, trademark, manufacturer, or otherwise does not necessarily constitute or imply its endorsement, recommendation, or favoring by the United States government or any agency thereof. The views and opinions of authors expressed herein do not necessarily state or reflect those of the United States government or any agency thereof. -
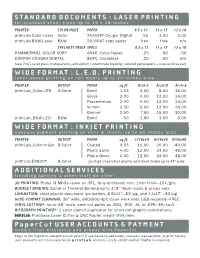
Standard Documents : Laser Printing Wide Format : L.E.D
STANDARD DOCUMENTS : LASER PRINTING for standard sheet sizes up to 12 x 18 inches PRINTER COLOR MODE PAPER 8.5 x 11 11 x 17 12 x 18 printLab-Color-Laser Color 24/60#T Cougar Digital .50 1.00 1.00 printLab-B&W-Laser B&W 20/50#T copy paper free free n/a SPECIALTY MEDIA SPECS 8.5 x 11 11 x 17 12 x 18 HAMMERMILL COLOR COPY 60#C, Extra-Heavy .25 .50 .50 DOMTAR COUGAR DIGITAL 80#C, Cardstock .25 .50 n/a Also: 70#T, laser gloss, transparency, and vellum / strathmore drawing / colored copy papers — sizes & prices vary WIDE FORMAT : L.E.D. PRINTING toner-based printing on roll media up to 36 inches wide PRINTER OUTPUT PAPER sq.ft. Arch-C Arch-D Arch-E printLab_Color-LED 4-Color Bond 1.33 4.00 8.00 16.00 Gloss 2.00 6.00 12.00 24.00 Presentation 2.00 6.00 12.00 24.00 Vellum 2.00 6.00 12.00 24.00 Banner 2.50 7.50 15.00 30.00 printLab_B&W-LED B&W Bond .50 1.50 3.00 6.00 WIDE FORMAT : INKJET PRINTING aqueous pigment printing on rolls & sheets up to 60 inches wide PRINTER OUTPUT PAPER sq.ft. C/18x24 D/24x36 E/36x48 printLab_Color-Inkjet 8-Color Coated 3.33 10.00 20.00 40.00 Photo Satin 4.00 12.00 24.00 48.00 Photo Gloss 4.00 12.00 24.00 48.00 printLab-E9800* 8-Color for high-resolution photos and sheet media up to 44” wide ADDITIONAL SERVICES finishing options & other stuff we offer 3D PRINTING: Prusa i3 MK3s—save as .STL, fully-enclosed; min. -
Introduction to Printing Technologies
Edited with the trial version of Foxit Advanced PDF Editor To remove this notice, visit: www.foxitsoftware.com/shopping Introduction to Printing Technologies Study Material for Students : Introduction to Printing Technologies CAREER OPPORTUNITIES IN MEDIA WORLD Mass communication and Journalism is institutionalized and source specific. Itfunctions through well-organized professionals and has an ever increasing interlace. Mass media has a global availability and it has converted the whole world in to a global village. A qualified journalism professional can take up a job of educating, entertaining, informing, persuading, interpreting, and guiding. Working in print media offers the opportunities to be a news reporter, news presenter, an editor, a feature writer, a photojournalist, etc. Electronic media offers great opportunities of being a news reporter, news editor, newsreader, programme host, interviewer, cameraman,Edited with theproducer, trial version of Foxit Advanced PDF Editor director, etc. To remove this notice, visit: www.foxitsoftware.com/shopping Other titles of Mass Communication and Journalism professionals are script writer, production assistant, technical director, floor manager, lighting director, scenic director, coordinator, creative director, advertiser, media planner, media consultant, public relation officer, counselor, front office executive, event manager and others. 2 : Introduction to Printing Technologies INTRODUCTION The book introduces the students to fundamentals of printing. Today printing technology is a part of our everyday life. It is all around us. T h e history and origin of printing technology are also discussed in the book. Students of mass communication will also learn about t h e different types of printing and typography in this book. The book will also make a comparison between Traditional Printing Vs Modern Typography. -

& Who's Who in Printing 2018 Printing Impressions
2018 Printing Impressions 35th Annua l Ranking & Who’s Who in Printing PIworld.com | Printing Impressions 1 2018 PRINTING IMPRESSIONS Celebrating its 35th consecutive year, the PRINTING IMPRESSIONS 400 provides the industry’s most comprehensive listing 35th Annua of the leading printing companies in the l Ranking United States and Canada ranked by annual sales volume. The listings include company name and the their annual revenue figures, so they are not location of the headquarters; parent company, included on our PI 400 list. This year, based if applicable; current and previous year’s rank- on Forbes’ ranking of the largest privately-held ings; most recent and previous fiscal year sales companies, we included Taylor Corp. and figures; percentage change in sales; primary used Forbes’ estimated sales calculation. product specialties; principal officer(s); number In addition, some very large firms that are of employees and manufacturing plants; as well ranked, notably RR Donnelley, would not, as the firm’s total range of in-house sheetfed or could not, break down their annual sales and webfed digital and conventional printing by the various print market specialties that process capabilities. we track (so, they may not appear on some of The financial information shown for the our Top 5 market segment leaders charts). PI 400 rankings was provided voluntarily by Individual printing companies that are privately-held and employee-owned firms, part of larger graphic arts networks are not and we instructed companies to not provide listed separately. In essence, to do so would be projected/estimated sales figures if their fiscal to show sales figures twice. -

(12) United States Patent (10) Patent No.: US 7,050,725 B2 Jingu (45) Date of Patent: May 23, 2006
US007050725B2 (12) United States Patent (10) Patent No.: US 7,050,725 B2 Jingu (45) Date of Patent: May 23, 2006 (54) IMAGE FORMING APPARATUS 5,373.350 A * 12/1994 Taylor et al. .................. EMPLOYING TWO PRINTING METHODS 5,563,694. A * 10/1996 Katayama ............ 5,729,785 A * 3/1998 Sakaizawa et al. ... (75) Inventor: Hidehito Jingu, Tokyo (JP) 5,781,823 A * 7/1998 Isobe et al. .................... 399.2 6,725,770 B1 * 4/2004 Maeda ....................... 101 129 (73) Assignee: Oki Data Corporation, Tokyo (JP) FOREIGN PATENT DOCUMENTS (*) Notice: Subject to any disclaimer, the term of this JP 09-169474 6, 1997 patent is extended or adjusted under 35 k . U.S.C. 154(b) by 0 days. cited by examiner Primaryy Examiner—Louis Arana (21) Appl. No.: 10/790,041 (74) Attorney, Agent, or Firm—Rabin & Berdo, PC (65) Prior Publication Data US 2004/0175191 A1 Sep. 9, 2004 An image forming apparatus has a first image forming unit and a second image forming unit that form images by (30) Foreign Application Priority Data different methods on the same page. The image formed by Mar. 3, 2003 (JP) 2003-055.192 the second image forming unit is used as an identifying • - s 1- w - way - F · · · · · · · · · · · · · · · · · · · · · · · · · · · · · image to distinguish an original document made by the (51) Int. Cl. image forming apparatus from copies of the original docu GO3G I5/00 (2006.01) ment. The second image forming unit may, for example, (52) U.S. Cl 399/2: 39976 emboss or punch holes in the printing medium. The second (58) Field O f Classification search- - - - - - - - - - - - 399A2 image forming unit may accordingly be a serial impact dot - - - - - - - - - - - - - - - - - - - -39976 7 matrix printing unit or a stamping unit, while the first See application file for complete search history s printing unit may be, for example, an inkjet printing unit or an electrophotographic printing unit. -

Inkjet and Inkjet-Based 3D Printing: Connecting Fluid Properties and Printing Performance
Inkjet and inkjet-based 3D printing: connecting fluid properties and printing performance Yang Guo, Huseini S. Patanwala and Brice Bognet Institute of Materials Science, University of Connecticut, Storrs, Connecticut, USA, and Anson W.K. Ma Polymer Program, Institute of Materials Science, University of Connecticut, Storrs, Connecticut, USA and Department of Chemical and Biomolecular Engineering, University of Connecticut, Storrs, Connecticut, USA Abstract Purpose – This paper aims to summarize the latest developments both in terms of theoretical understanding and experimental techniques related to inkjet fluids. The purpose is to provide practitioners a self-contained review of how the performance of inkjet and inkjet-based three-dimensional (3D) printing is fundamentally influenced by the properties of inkjet fluids. Design/methodology/approach – This paper is written for practitioners who may not be familiar with the underlying physics of inkjet printing. The paper thus begins with a brief review of basic concepts in inkjet fluid characterization and the relevant dimensionless groups. Then, how drop impact and contact angle affect the footprint and resolution of inkjet printing is reviewed, especially onto powder and fabrics that are relevant to 3D printing and flexible electronics applications. A future outlook is given at the end of this review paper. Findings – The jettability of Newtonian fluids is well-studied and has been generalized using a dimensionless Ohnesorge number. However, the inclusion of various functional materials may modify the ink fluid properties, leading to non-Newtonian behavior, such as shear thinning and elasticity. This paper discusses the current understanding of common inkjet fluids, such as particle suspensions, shear-thinning fluids and viscoelastic fluids. -

Polymer-Relief Microstructures by Inkjet Etching**
DOI: 10.1002/adma.200502051 Polymer-Relief Microstructures by Inkjet Etching** By Berend-Jan de Gans, Stephanie Hoeppener, and Ulrich S. Schubert* COMMUNICATIONS Inkjet printing is developing at a rapid pace. The last de- microstructures, whereby a more direct structuring technique cade saw continuous improvements in quality and resolution, can be applied than in common photolithographic approach- and the technology has now arrived at the point where it chal- es. The spreading and the minimum diameter of the inkjet- lenges conventional silver halide photography. But inkjet printed droplets, which in recent years could be decreased to technology is not only a printing technology. A lot of effort is less than 10 lm, set the resolution. Even if inkjet etching may being put into turning inkjet printing into a versatile tool for not be feasible for production, since it is not as fast as conven- various industrial processes for accurately depositing minute tional production technologies such as screen printing, the quantities of materials in defined spots on surfaces, in particu- combination of low cost and flexibility makes it an ideal can- lar in plastic electronics and polymer light-emitting diodes.[1–5] didate for rapid-prototyping applications. Inkjet etching also Inkjet printing may also become a cost-saving alternative to holds enormous potential for the production of biochips and photolithography for the production of next-generation ac- micropatterned cell arrays where one single process step suf- tive-matrix liquid-crystal displays.[6] -

Xerox® Impika® Reference Inkjet Press
Xerox® Impika® Reference Inkjet Press The ultimate versatility in continuous feed inkjet printing. The Impika Reference is a supremely scalable system, providing valuable options to manage speed, inks and image quality so you can keep costs low without sacrificing performance. Configurable to help you meet today’s Key benefits of the Impika Reference: Seamless integration in your workflow— Three controller options provide even more needs, as well as tomorrow’s. Modular design—Engineered for scalability, flexibility in how you integrate the Impika The Impika Reference takes the hallmark with options for number of print heads, Reference into your environment. of the entire Impika line—configurability— colors, and speed in either a single or two to a whole new level. Start by choosing a tower configuration. The Xerox® Impika® Controller is a PC-based configuration ranging from single engine 1-up RIP and spool solution that supports the PDF Proven technology—Based on reliable, duplex to dual engine 2-up duplex based on and PostScript workflows typically found in high performance drop-on-demand your expected productivity requirement. direct mail or book production workflows. piezoelectric inkjet technology. You can further modify that base system to The Xerox® Impika® IPDS Controller supports Low printing costs—A quick ROI is meet new needs over time. Adding a print head IPDS workflows for high speed, fully variable achieved through: to the base four color offering enables MICR data direct mail or transaction jobs and can and opens up even more application potential. • Use of low-cost papers with new generation easily scale up as volume or complexity grows. -

Keeping Business Moving
Financial Services and SIDM Range KEEPING BUSINESS MOVING FINANCIAL SERVICES PRODUCT RANGE Epson is the world’s largest manufacturer of printers for banks and post offices with a product range that offers the ultimate in high speed, low cost, reliable and durable printing across all stationery types. Ideal for back office, cheque processing, and multi-part stationery, for which there is simply no alternative other than impact printing. EPSON 9-PIN DOT MATRIX PRINTERS Ideal for commercial, industrial and logistic applications, Epson’s 9-pin dot matrix range offers excellent print quality for a competitive price. Combining high precision alignment and sophisticated paper handling, this comprehensive range of narrow and wide carriage 1 printers can tackle even heavy duty print jobs. EPSON 24-PIN DOT MATRIX PRINTERS Offering all the features available across the 9-pin range, but with the advantage of scalable fonts and letter quality printing. Epson 24-pin printers are ideal for front desk applications in the retail and service industries, as well as invoice and order printing. The range also includes flatbed printers for use with a wider (and thicker) range of materials including receipts and labels. 02 Field of application Printer model Printhead/ Duty Point Instore Accounting Listing Pass-book Cheque Brochure Resolution of sale handling page Epson LX-350 9-pin Light 8 Epson LX-1350 Medium 8 Epson FX-890/890A High 9 Epson FX-2190/2190N High 9 Epson DFX-9000/9000N Heavy 10 Epson LQ-50 24-pin Light 10 Epson LQ-350 Light 11 Epson LQ-590 Medium -
Infotrends Emerging Technologies White Paper
January 17, 2008 Strategic Assessment Emerging Marking Technologies: A Review and Comparison of Xerographic and Ink- Based Imaging Authors Abstract Robert Palmer Several ink-based marking technologies have recently surfaced, and these technologies are causing quite a stir in the market. The potential for inkjet technology is based on some basic principles: ink costs less than toner; ink print heads have relatively few parts; and the quality that can be delivered is high. This white paper provides an overview and history of marking technologies and explains the potential benefits that ink-based systems could deliver to the office printing market. Published by Digital Peripherals Solutions Consulting Service For More Information © 2008 InfoTrends, Inc. If you would like to order extra copies of this report, receive permission to use any part of the www.infotrends.com report, or be informed of upcoming market updates, reports, and related projects, please e-mail us at [email protected]. Headquarters: Europe: Asia: 97 Libbey Industrial Parkway 3rd Floor, Sceptre House Hiroo Office Building Suite 300 7-9 Castle Street 1-3-18 Hiroo, Shibuya-ku Weymouth, MA 02189 Luton, Bedfordshire Tokyo 150-0012 United States United Kingdom, LU1 3AJ Japan +1 781 616 2100 +44 1582 400120 +81 3 5475 2663 [email protected] [email protected] [email protected] Emerging Marking Technologies January 2008 Table of Contents Introduction ................................................................................................................................ -

Color Inkjet Printing and Laser Marking for Plastics by Scott Sabreen, President, the Sabreen Group, Inc
TECHNOLOGY Color Inkjet Printing and Laser Marking for Plastics by Scott Sabreen, president, The Sabreen Group, Inc. igital printing technologies, such as inkjet and required results. As a result, the “total solutions” aspects of inkjet laser on plastics, offer monumental advantages printing and laser marking technologies as a guide for systems Dfor manufacturers compared to traditional analog procurement and process optimization become very important. methods, e.g., pad printing, hot stamping, screen printing, etc. Digital printing allows for full product customization, unique Piezoelectric “drop-on-demand” UV LED inkjet technology alphanumeric part identification, product security, serialization, Inkjet is noncontact, computer-to-print process where barcode/2D codes, logos, graphics and more. These capabilities droplets of ink are propelled toward a substrate in a regular are essential for today’s digital interactive universe. A tangential x-y pixel pattern derived from benefit is the capability to print assembled products at the end a digital file. Major system of manufacturing operations, which offers cost savings and components consist of a better inventory control management. This article examines printhead assembly, printhead two types of digital printing/marking process methods: full drive electronic controllers, color piezoelectric drop-on-demand inkjet printing and beam- UV inks, curing irradiator steered fiber laser marking. Piezoelectric drop-on-demand and motion-controlled parts (DOD) inkjet and fiber laser are modern technologies that offer handling. countless advantages for product (and mass) customization. The basic component is the Piezoelectric DOD inkjet printing and beam-steered fiber printhead (Figure 2). It has a laser marking are both digital, noncontact processes. Many supply of ink and a multiplicity manufacturers already recognize the value of offering both of small volume ink chambers technologies to meet custom printing requirements on diverse with circular nozzles from polymeric substrates. -

Inkjet Printing for 2D and 3D Printed Electronics Meyer Burger Netherlands
Inkjet printing for 2D and 3D printed electronics Meyer Burger Netherlands Jan 2016 Meyer Burger Netherlands products For flexible electronics - From Research to Production PECVD / ALD ™ FLEx LT FLEx XL FLEx R2R Engineering Pilot Production Mass Production Versatile Flexible Efficient ™ IP410 JETx LP50 Functional inkjet What is functional inkjet printing? . Piezo element presses on a fluid channel Ink channel and ejects a droplet of functional material Nozzle plate . Advantages of technique: . Additive (instead of subtractive): . less process steps 0 . optimal use of precious materials . Direct digital (without mask or master): . little pre-production costs . better economy-of-scale . inline correction and yield improvement . Contact-less: . minimizing breakage . printing on non-flat topology . 3-dimensional Distance to nozzle plate (mm) 1 Inkjet Inks Types and Operating Conditions Main types of ink Solvent-based Source: Annu. Rev. Mater. Res. 40:395, 2010 Particle dispersion UV and/or monomer Polymers Too viscous Viscosity* 8 – 20 cPoise (mPa.s) Surface tension 24 – 36 Dyne/cm (mN/m) Satellite droplets Typical ingredients Functional material Carrier liquids/solvents Surfactants Viscosity modifiers Insufficient energy Adhesion promoters Dispersants Particle size < ~1 µm *Viscosity references Post treatments Drying Wide selection of materials:Water = 1 cP UV-curing conductive, dielectric, adhesive,Olive oil = 80 cP Sintering (thermal, laser, Honey = 10,000 cP photonic) resist, biologic, ceramic, optical,.. Conductive Inks Applications Printed