An Overview of 3D Printing Technologies for Soft Materials and Potential Opportunities for Lipid-Based Drug Delivery Systems
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Metallizations by Direct-Write Inkjet Printing
October 2001 • NREL/CP-520-31020 Metallizations by Direct-Write Inkjet Printing Preprint C. Curtis, T. Rivkin, A. Miedaner, J. Alleman, J. Perkins, L. Smith, and D. Ginley To be presented at the NCPV Program Review Meeting Lakewood, Colorado 14-17 October 2001 National Renewable Energy Laboratory 1617 Cole Boulevard Golden, Colorado 80401-3393 NREL is a U.S. Department of Energy Laboratory Operated by Midwest Research Institute ••• Battelle ••• Bechtel Contract No. DE-AC36-99-GO10337 NOTICE The submitted manuscript has been offered by an employee of the Midwest Research Institute (MRI), a contractor of the US Government under Contract No. DE-AC36-99GO10337. Accordingly, the US Government and MRI retain a nonexclusive royalty-free license to publish or reproduce the published form of this contribution, or allow others to do so, for US Government purposes. This report was prepared as an account of work sponsored by an agency of the United States government. Neither the United States government nor any agency thereof, nor any of their employees, makes any warranty, express or implied, or assumes any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, apparatus, product, or process disclosed, or represents that its use would not infringe privately owned rights. Reference herein to any specific commercial product, process, or service by trade name, trademark, manufacturer, or otherwise does not necessarily constitute or imply its endorsement, recommendation, or favoring by the United States government or any agency thereof. The views and opinions of authors expressed herein do not necessarily state or reflect those of the United States government or any agency thereof. -
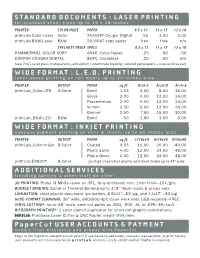
Standard Documents : Laser Printing Wide Format : L.E.D
STANDARD DOCUMENTS : LASER PRINTING for standard sheet sizes up to 12 x 18 inches PRINTER COLOR MODE PAPER 8.5 x 11 11 x 17 12 x 18 printLab-Color-Laser Color 24/60#T Cougar Digital .50 1.00 1.00 printLab-B&W-Laser B&W 20/50#T copy paper free free n/a SPECIALTY MEDIA SPECS 8.5 x 11 11 x 17 12 x 18 HAMMERMILL COLOR COPY 60#C, Extra-Heavy .25 .50 .50 DOMTAR COUGAR DIGITAL 80#C, Cardstock .25 .50 n/a Also: 70#T, laser gloss, transparency, and vellum / strathmore drawing / colored copy papers — sizes & prices vary WIDE FORMAT : L.E.D. PRINTING toner-based printing on roll media up to 36 inches wide PRINTER OUTPUT PAPER sq.ft. Arch-C Arch-D Arch-E printLab_Color-LED 4-Color Bond 1.33 4.00 8.00 16.00 Gloss 2.00 6.00 12.00 24.00 Presentation 2.00 6.00 12.00 24.00 Vellum 2.00 6.00 12.00 24.00 Banner 2.50 7.50 15.00 30.00 printLab_B&W-LED B&W Bond .50 1.50 3.00 6.00 WIDE FORMAT : INKJET PRINTING aqueous pigment printing on rolls & sheets up to 60 inches wide PRINTER OUTPUT PAPER sq.ft. C/18x24 D/24x36 E/36x48 printLab_Color-Inkjet 8-Color Coated 3.33 10.00 20.00 40.00 Photo Satin 4.00 12.00 24.00 48.00 Photo Gloss 4.00 12.00 24.00 48.00 printLab-E9800* 8-Color for high-resolution photos and sheet media up to 44” wide ADDITIONAL SERVICES finishing options & other stuff we offer 3D PRINTING: Prusa i3 MK3s—save as .STL, fully-enclosed; min. -
Introduction to Printing Technologies
Edited with the trial version of Foxit Advanced PDF Editor To remove this notice, visit: www.foxitsoftware.com/shopping Introduction to Printing Technologies Study Material for Students : Introduction to Printing Technologies CAREER OPPORTUNITIES IN MEDIA WORLD Mass communication and Journalism is institutionalized and source specific. Itfunctions through well-organized professionals and has an ever increasing interlace. Mass media has a global availability and it has converted the whole world in to a global village. A qualified journalism professional can take up a job of educating, entertaining, informing, persuading, interpreting, and guiding. Working in print media offers the opportunities to be a news reporter, news presenter, an editor, a feature writer, a photojournalist, etc. Electronic media offers great opportunities of being a news reporter, news editor, newsreader, programme host, interviewer, cameraman,Edited with theproducer, trial version of Foxit Advanced PDF Editor director, etc. To remove this notice, visit: www.foxitsoftware.com/shopping Other titles of Mass Communication and Journalism professionals are script writer, production assistant, technical director, floor manager, lighting director, scenic director, coordinator, creative director, advertiser, media planner, media consultant, public relation officer, counselor, front office executive, event manager and others. 2 : Introduction to Printing Technologies INTRODUCTION The book introduces the students to fundamentals of printing. Today printing technology is a part of our everyday life. It is all around us. T h e history and origin of printing technology are also discussed in the book. Students of mass communication will also learn about t h e different types of printing and typography in this book. The book will also make a comparison between Traditional Printing Vs Modern Typography. -

Real-Time Kinematics Coordinated Swarm Robotics for Construction 3D Printing
1 Real-time Kinematics Coordinated Swarm Robotics for Construction 3D Printing Darren Wang and Robert Zhu, John Jay High School Abstract Architectural advancements in housing are limited by traditional construction techniques. Construction 3D printing introduces freedom in design that can lead to drastic improvements in building quality, resource efficiency, and cost. Designs for current construction 3D printers have limited build volume and at the scale needed for printing houses, transportation and setup become issues. We propose a swarm robotics-based construction 3D printing system that bypasses all these issues. A central computer will coordinate the movement and actions of a swarm of robots which are each capable of extruding concrete in a programmable path and navigating on both the ground and the structure. The central computer will create paths for each robot to follow by processing the G-code obtained from slicing a CAD model of the intended structure. The robots will use readings from real-time kinematics (RTK) modules to keep themselves on their designated paths. Our goal for this semester is to create a single functioning unit of the swarm and to develop a system for coordinating its movement and actions. Problem Traditional concrete construction is costly, has substantial environmental impact, and limits freedom in design. In traditional concrete construction, workers use special molds called forms to shape concrete. Over a third of the construction cost of a concrete house stems from the formwork alone. Concrete manufacturing and construction are responsible for 6% – 8% of CO2 emissions as well as 10% of energy usage in the world. Many buildings use more concrete than necessary, and this stems from the fact that formwork construction requires walls, floors, and beams to be solid. -

& Who's Who in Printing 2018 Printing Impressions
2018 Printing Impressions 35th Annua l Ranking & Who’s Who in Printing PIworld.com | Printing Impressions 1 2018 PRINTING IMPRESSIONS Celebrating its 35th consecutive year, the PRINTING IMPRESSIONS 400 provides the industry’s most comprehensive listing 35th Annua of the leading printing companies in the l Ranking United States and Canada ranked by annual sales volume. The listings include company name and the their annual revenue figures, so they are not location of the headquarters; parent company, included on our PI 400 list. This year, based if applicable; current and previous year’s rank- on Forbes’ ranking of the largest privately-held ings; most recent and previous fiscal year sales companies, we included Taylor Corp. and figures; percentage change in sales; primary used Forbes’ estimated sales calculation. product specialties; principal officer(s); number In addition, some very large firms that are of employees and manufacturing plants; as well ranked, notably RR Donnelley, would not, as the firm’s total range of in-house sheetfed or could not, break down their annual sales and webfed digital and conventional printing by the various print market specialties that process capabilities. we track (so, they may not appear on some of The financial information shown for the our Top 5 market segment leaders charts). PI 400 rankings was provided voluntarily by Individual printing companies that are privately-held and employee-owned firms, part of larger graphic arts networks are not and we instructed companies to not provide listed separately. In essence, to do so would be projected/estimated sales figures if their fiscal to show sales figures twice. -

Carbon Nanotubes and Graphene As Additives in 3D Printing Lara A
University of Massachusetts Amherst ScholarWorks@UMass Amherst Chemistry Department Faculty Publication Series Chemistry 2016 Carbon Nanotubes and Graphene as Additives in 3D Printing Lara A. Al-Hariri University of Massachusetts Amherst Branden Leonhardt Florida State University Mesopotamia Nowotarski Florida State University James Magi Florida State University Kaelynn Chambliss Florida State University See next page for additional authors Follow this and additional works at: https://scholarworks.umass.edu/chem_faculty_pubs Part of the Chemistry Commons, and the Education Commons Recommended Citation Al-Hariri, Lara A.; Leonhardt, Branden; Nowotarski, Mesopotamia; Magi, James; Chambliss, Kaelynn; Venzel, Thaís; Delekar, Sagar; and Acquah, Steve, "Carbon Nanotubes and Graphene as Additives in 3D Printing" (2016). Carbon Nanotubes - Current Progress of their Polymer Composites. 1448. https://doi.org/10.5772/63419 This Article is brought to you for free and open access by the Chemistry at ScholarWorks@UMass Amherst. It has been accepted for inclusion in Chemistry Department Faculty Publication Series by an authorized administrator of ScholarWorks@UMass Amherst. For more information, please contact [email protected]. Authors Lara A. Al-Hariri, Branden Leonhardt, Mesopotamia Nowotarski, James Magi, Kaelynn Chambliss, Thaís Venzel, Sagar Delekar, and Steve Acquah This article is available at ScholarWorks@UMass Amherst: https://scholarworks.umass.edu/chem_faculty_pubs/1448 PUBLISHED BY World's largest Science, Technology & Medicine -
3D Printing Technology Applications in Occupational Therapy
Open Access Physical Medicine and Rehabilitation - International Special Article – Occupational Therapy 3D Printing Technology Applications in Occupational Therapy Ganesan B1,2, Al-Jumaily A1 and Luximon A2* 1Faculty of Engineering and IT, University of Technology Abstract Sydney, Australia With the rapid development of three dimensional technologies in last three 2The Hong Kong Polytechnic University, Hong Kong decades, it is widely spread worldwide and made dramatic impact into various *Corresponding author: Luximon Ameersing, The fields such as medicine, dentistry, other health care and engineering area. The Hong Kong Polytechnic University, Hung Hom, Hong promising future of this 3D printing technology made new future in the medicine Kong to design the various hard tissues, models of body parts, implants, orthosis and prosthesis with high accuracy. This paper focuses on the possibilities Received: May 26, 2016; Accepted: June 06, 2016; and benefits of 3D printing technology in the occupational therapy research Published: June 09, 2016 or clinical practice and presents the different procedures for creating different types of three dimensional physical models. Keywords: 3D printing; Occupational Therapy; Three dimensional Printing; Assistive devices Introduction 3D three-dimensional printing (3DP), Ink Jet printing techniques, vacuum casting and milling (VCM), two-photon polymerization Three dimensional (3D) printing is a novel emerging technology (TPP), direct laser metal sintering (DLMS) [6, 14]. In medicine, there widely used for various fields such as medical, engineering, are different types of materials are used to create rapid prototype educations, and other industrial areas. It is the process of making model of medical devices and implants such as stainless steel, Cobalt three dimensional physical models by using 3D software, computer, Chromium alloys (Co Cr), titanium (Ti) alloys, Polycaprolactone and printer. -
Challenges in the Optimization of 3D Printing of Zirconia Based Pastes By
Challenges in the optimization of 3D printing and robocasting processes using zirconia based pastes 2018 NanoMatLab/Biomat Meeting Robocasting - Introduction • Layer-by-layer deposition of ceramic slurries (paste) through a nozzle (extrusion). • Computer numerical control over nozzle position coordinates and piston movement. • Nozzle diameter ranging from 0.03mm to 2mm. Freeforming 24h. Ceramic parts with bespoke, intricate geometries can be produced quickly and inexpensively. Picture source: [1] Substrate bed heated to 30 [1], [2], [3] Robocasting – Products [4] [1] Robocasting - Slurries • Slurries must be pseudoplastic to flow through the nozzle. • Slurry compositions are kept close to the dilatant ratio. Dilatant Capillarity Adapted from [4] [2] Adapted from [2] • Dilatant mass maintains structural integrity after minimal drying time. • Heated bed speeds up the pseudoplastic to dilatant transition. [2], [4] Robocasting - Slurries • Slurries of high solid fraction, usually 50-65 vol.% ceramic powder. • 35-50 vol.% volatile solvent (usually water). • Higher ceramic loadings decrease sintering shrinkage and cracking. • Highly loaded slurries are prone to agglomeration, that can cause nozzle clogging during extrusion. • Tested slurries: Slurry designation Zirconia powder Powder/dispersant loading weight ratio X High High Y Medium Low Z Low Low [2], [3] 3D Printer Commercial open source 3D printer “Lulzbot MINI” Syringe Hypodermic (extruder) + needle (nozzle) Printing parameters Optimization - Example Movement Extruded slurry Increase flow -

Building 3D-Structures with an Intelligent Robot Swarm
BUILDING 3D-STRUCTURES WITH AN INTELLIGENT ROBOT SWARM A Dissertation Presented to the Faculty of the Graduate School of Cornell University in Partial Fulfillment of the Requirements for the Degree of Master of Science by Yiwen Hua May 2018 c 2018 Yiwen Hua ALL RIGHTS RESERVED BUILDING 3D-STRUCTURES WITH AN INTELLIGENT ROBOT SWARM Yiwen Hua, M.S. Cornell University 2018 This research is an extension to the TERMES system, a decentralized au- tonomous construction team composed of swarm robots building 2.5D struc- tures1, with custom-designed bricks. The work in this thesis concerns 1) im- proved mechanical design of the robots, 2) addition of heterogeneous building material, and 3) an extended algorithmic framework to use this material. In or- der to lower system cost and maintenance, the TERMES robot is redesigned for manufacturing in low-end 3D printers and the new drive train, including motor adapters and pulleys, is based on 3D printed components instead of machined aluminum. The work further extends the original system by enabling construc- tion of 3D structures without added hardware complexity in the robots. To do this, we introduce a reusable, spring-loaded expandable brick which can be eas- ily manufactured through one-step casting and which complies with the origi- nal robots and bricks. This thesis also introduces a decentralized construction algorithm that permits an arbitrary number of robots to build overhangs over convex cavities. To enable timely completion of large-scale structures, we also introduce a method by which to optimize the transition probabilities used by the robots to traverse the structure. -

(12) United States Patent (10) Patent No.: US 7,050,725 B2 Jingu (45) Date of Patent: May 23, 2006
US007050725B2 (12) United States Patent (10) Patent No.: US 7,050,725 B2 Jingu (45) Date of Patent: May 23, 2006 (54) IMAGE FORMING APPARATUS 5,373.350 A * 12/1994 Taylor et al. .................. EMPLOYING TWO PRINTING METHODS 5,563,694. A * 10/1996 Katayama ............ 5,729,785 A * 3/1998 Sakaizawa et al. ... (75) Inventor: Hidehito Jingu, Tokyo (JP) 5,781,823 A * 7/1998 Isobe et al. .................... 399.2 6,725,770 B1 * 4/2004 Maeda ....................... 101 129 (73) Assignee: Oki Data Corporation, Tokyo (JP) FOREIGN PATENT DOCUMENTS (*) Notice: Subject to any disclaimer, the term of this JP 09-169474 6, 1997 patent is extended or adjusted under 35 k . U.S.C. 154(b) by 0 days. cited by examiner Primaryy Examiner—Louis Arana (21) Appl. No.: 10/790,041 (74) Attorney, Agent, or Firm—Rabin & Berdo, PC (65) Prior Publication Data US 2004/0175191 A1 Sep. 9, 2004 An image forming apparatus has a first image forming unit and a second image forming unit that form images by (30) Foreign Application Priority Data different methods on the same page. The image formed by Mar. 3, 2003 (JP) 2003-055.192 the second image forming unit is used as an identifying • - s 1- w - way - F · · · · · · · · · · · · · · · · · · · · · · · · · · · · · image to distinguish an original document made by the (51) Int. Cl. image forming apparatus from copies of the original docu GO3G I5/00 (2006.01) ment. The second image forming unit may, for example, (52) U.S. Cl 399/2: 39976 emboss or punch holes in the printing medium. The second (58) Field O f Classification search- - - - - - - - - - - - 399A2 image forming unit may accordingly be a serial impact dot - - - - - - - - - - - - - - - - - - - -39976 7 matrix printing unit or a stamping unit, while the first See application file for complete search history s printing unit may be, for example, an inkjet printing unit or an electrophotographic printing unit. -

Inkjet and Inkjet-Based 3D Printing: Connecting Fluid Properties and Printing Performance
Inkjet and inkjet-based 3D printing: connecting fluid properties and printing performance Yang Guo, Huseini S. Patanwala and Brice Bognet Institute of Materials Science, University of Connecticut, Storrs, Connecticut, USA, and Anson W.K. Ma Polymer Program, Institute of Materials Science, University of Connecticut, Storrs, Connecticut, USA and Department of Chemical and Biomolecular Engineering, University of Connecticut, Storrs, Connecticut, USA Abstract Purpose – This paper aims to summarize the latest developments both in terms of theoretical understanding and experimental techniques related to inkjet fluids. The purpose is to provide practitioners a self-contained review of how the performance of inkjet and inkjet-based three-dimensional (3D) printing is fundamentally influenced by the properties of inkjet fluids. Design/methodology/approach – This paper is written for practitioners who may not be familiar with the underlying physics of inkjet printing. The paper thus begins with a brief review of basic concepts in inkjet fluid characterization and the relevant dimensionless groups. Then, how drop impact and contact angle affect the footprint and resolution of inkjet printing is reviewed, especially onto powder and fabrics that are relevant to 3D printing and flexible electronics applications. A future outlook is given at the end of this review paper. Findings – The jettability of Newtonian fluids is well-studied and has been generalized using a dimensionless Ohnesorge number. However, the inclusion of various functional materials may modify the ink fluid properties, leading to non-Newtonian behavior, such as shear thinning and elasticity. This paper discusses the current understanding of common inkjet fluids, such as particle suspensions, shear-thinning fluids and viscoelastic fluids. -

A Study on 3D Printing and Its Effects on the Future of Transportation
CAIT-UTC-NC19 A Study on 3D Printing and its Effects on the Future of Transportation September 2018 Submitted by: Omar Jumaah, Doctoral Candidate Department of Mechanical and Aerospace Engineering Rutgers, The State University of New Jersey 98 Brett Road Piscataway, NJ 08854-8058 [email protected] External Project Manager Patrick Szary, PhD Associate Director, CAIT Central Administration Rutgers, The State University of New Jersey 100 Brett Road Piscataway, NJ 08854-8058 [email protected] In cooperation with Rutgers, The State University of New Jersey & State of Department of Transportation & U.S. Department of Transportation Federal Highway Administration i Disclaimer Statement The contents of this report reflect the views of the authors, who are responsible for the facts and the accuracy of the information presented herein. This document is disseminated under the sponsorship of the Department of Transportation, University Transportation Centers Program, in the interest of information exchange. The U.S. Government assumes no liability for the contents or use thereof. The Center for Advanced Infrastructure and Transportation (CAIT) is a National UTC Consortium led by Rutgers, The State University. Members of the consortium are the University of Delaware, Utah State University, Columbia University, New Jersey Institute of Technology, Princeton University, University of Texas at El Paso, Virginia Polytechnic Institute, and University of South Florida. The Center is funded by the U.S. Department of Transportation. ii CAIT-UTC-NC19 1. Report No. 2. Government Accession No. 3. Recipient’s Catalog No. CAIT-UTC-NC19 4. Title and Subtitle 5. Report Date A Study on 3D Printing and its Effects on the Future of Transportation September 2018 6.