Royal Preston Hospital Scheduled Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Pocketbook for You, in Any Print Style: Including Updated and Filtered Data, However You Want It
Hello Since 1994, Media UK - www.mediauk.com - has contained a full media directory. We now contain media news from over 50 sources, RAJAR and playlist information, the industry's widest selection of radio jobs, and much more - and it's all free. From our directory, we're proud to be able to produce a new edition of the Radio Pocket Book. We've based this on the Radio Authority version that was available when we launched 17 years ago. We hope you find it useful. Enjoy this return of an old favourite: and set mediauk.com on your browser favourites list. James Cridland Managing Director Media UK First published in Great Britain in September 2011 Copyright © 1994-2011 Not At All Bad Ltd. All Rights Reserved. mediauk.com/terms This edition produced October 18, 2011 Set in Book Antiqua Printed on dead trees Published by Not At All Bad Ltd (t/a Media UK) Registered in England, No 6312072 Registered Office (not for correspondence): 96a Curtain Road, London EC2A 3AA 020 7100 1811 [email protected] @mediauk www.mediauk.com Foreword In 1975, when I was 13, I wrote to the IBA to ask for a copy of their latest publication grandly titled Transmitting stations: a Pocket Guide. The year before I had listened with excitement to the launch of our local commercial station, Liverpool's Radio City, and wanted to find out what other stations I might be able to pick up. In those days the Guide covered TV as well as radio, which could only manage to fill two pages – but then there were only 19 “ILR” stations. -

Agenda Reports Pack (Public) 16/02/2012, 18.30
Public Document Pack METROPOLITAN BOROUGH OF SEFTON COUNCIL SUMMONS To Members of the Metropolitan Borough Council Dear Councillor You are requested to attend a Meeting of the Sefton Metropolitan Borough Council to be held on Thursday 16th February, 2012 at 6.30 pm at the Town Hall, Southport to transact the business set out on the agenda overleaf. Yours sincerely, Chief Executive Town Hall, Southport 8 February 2012 Please contact Steve Pearce, Head of Committee and Member Services on 0151 934 2046 or e-mail [email protected] 1 This page is intentionally left blank. 2 A G E N D A 1. Apologies for Absence 2. Declarations of Interest Members and Officers are requested to give notice of any personal or prejudicial interest and the nature of that interest, relating to any item on the agenda in accordance with the relevant Code of Conduct. 3. Minutes of Previous Meetings (Pages 7 - 14) Minutes of the meeting held on 24 November 2011 4. Mayor's Communications Public Session 5. Matters Raised by the Public To deal with matters raised by members of the public within the Borough, in accordance with the procedures relating to Petitions, Public Questions.and Motions set out in Rule 11 of the Council and Committee Procedure Rules. (Details of any further Petitions notified or Questions submitted to the Legal Director by members of the public in accordance with Rule 11 will be circulated at the meeting). Council Business Session 6. Questions Raised by Members of the Council To receive and consider questions to Cabinet Members, Chairs of Committees or Spokespersons for any of the Joint Authorities upon any matter within their portfolio/area of responsibility, of which notice has been given in accordance with Rule 12 of the Council and Committee Procedure Rules. -

Shining Lights Newsletter April 2017 Celebrating Success
Shining Lights Newsletter April 2017 Celebrating success Although it’s only been 8 weeks since our last Shining Lights newsletter there is SO much to celebrate this term. From charity fundraising to individual and team excellence we hope you enjoy reading all about the activities and events that took place during the Spring Term. GCSE Results Officially Top Class Earlier this month, The Department for Education confirmed how superb our results were last year in the published School Performance Tables. We knew they were good at the time but looking at the table opposite only serves to remind us how great they truly were. Progress 8 is the new measure for secondary schools and our result of +0.23 simply means that on average our pupils got a quarter of their GCSEs grades higher in each subject compared to all other pupils nationally. A great achievement! Teacher of the Year 2017 - Mrs Hall, we love you! A huge congratulations to Mrs Hall on becoming Teacher of the Year 2017. The award, presented by Rock FM, celebrates heroes from across Lancashire who have been honoured for their courage, selflessness and charity endeavours. This year’s award ceremony for the annual Rock FM Cash 4 Kids Time to Shine awards took place at the Blackpool Tower Ballroom. We are extremely proud of Mrs Hall and want to celebrate and thank her for all that she does in and out of school. She is truly amazing! Journey to Sanctuary Exhibition During the first week of Lent we hosted the 'Journey to Sanctuary' exhibition in school. -
Preston Map 30.1.2014.Indd
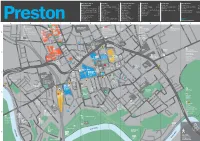
Museums, Arts & Shopping Landmarks & Parks Transport Information Miscellaneous Entertainment Cannon Street E3 Arkwright’s House F3 Bus Station F2 County Hall C4 Cotton Court G3 53 degrees C1 Fishergate Shopping Centre D4 Avenham Park E5 Park & Ride Parking A4,J5 Lancashire Records Office C3 Driving Theory Test Centre E4 Frog & Bucket Comedy Club F3 Friargate D2,E3 Avenham Pavilion E6 Park & Ride Town Hall F3 Post Office D4 Guild Hall & Charter Theatre F3 Fishergate D3,E3 Flag Market E3 Pick up C4,D4,E3,F2,F3,H3 Visitor Information Centre F3 University of Central Harris Museum & Art Gallery F3 Guild Hall Street E3 Harris Institute E5 Railway Station C4 Lancashire (UCLan) C1,C2 Korova D3 Lune Street D3 Miller Arcade F3 Shopmobility E3 Museum of Lancashire H2 Markets E2 Miller Park D6 Taxi Ranks C4,F3,F2 Playhouse Theatre D2 Miller Arcade F3 Preston Minster F3 PR1 Gallery C1 St George’s Shopping Centre E3 St Walburge’s Church B1 Map Key Preston The Continental C6 Winckley Street E4 Winckley Square E4 Please see reverse A B C D E F G H I J STREET L ON Police Division A PR1 Gallery T N D ) A583 Towards ) Headquarters C A6 Towards Noor Hall A6063 Towards 3 B6243 Towards AS A N HARRING 1 E 4 S O 2 Blackpool MAUDLAND 7 ST Blackpool M55 (J1) Mosque E Preston North End 6 G H T Longridge 53 Degrees EE T G R (B 0 STR E P E TON STREET TON N T E E OFFREY 5 OW R D N F CR ELLIN H A A A S L 1 Riversway Docklands Y ( R M M6 (J32) A Deepdale L Student R HO T N O MEADOW STREET L O D E V T A O LS I E Shopping Park E Hanover E Union L E L Ribble Steam Railway -

Pupils Visit Castlerigg the PE Department Pupils Mark Manor
ONECorpus Christi Catholic High School VOICESpring 2014 A HOLY TEAM OF READ ALL RETREAT THE YEAR ABOUT IT Pupils visit Castlerigg The PE department Pupils mark Manor. are celebrating a World Book Day. fantastic win. Giving our PUPILS YEAR 11 PUPILS ARE BmoreEING GIVEN SUPPORT TO PREPARE FOR THEIR SUMMER EXAMS ONE VOICE 1 CONTENTS WELCOME elcome to this first edition of our new school referred to our plans to improve progress and attainment as ‘well- ONE VOICE | SPRING ‘14 magazine ‘One Voice’. shaped’. We have much to celebrate as a school and A major priority this term has been to ensure that our Year 11 our termly magazine will capture some of the pupils attain the best possible GCSE results this summer. Colleagues highlights of our life as a school community. In have worked extremely hard to develop our new Year 11 Revision future editions we also hope to include articles Programme, which was launched with parents on Monday 10 March. 4 Helping Our Pupils to Achieve Success reflecting the many outstanding successes achieved by our former All pupils in Year 11 were provided with an individualised revision plan 6 Visiting Vibrant Media City Wpupils. setting out the revision work that they need to complete each day during the revision period. The response of Year 11 to our Revision Since April 2013 Corpus Christi Catholic High School has undergone Programme has been very impressive with the vast majority of pupils 8 A Refereeing Honour a period of rapid and significant change. Visitors to our school working very hard indeed to keep up with their revision work. -

Ashton Highlightshighlights
AshtonAshton HighlightsHighlights Newsletter 11 Friday 12th December 2014 It’s beginning to look a lot like Christmas here at Ashton. In the newsletter this week you can read all about the range of activities our staff and students have taken part in to spread the seasonal message of peace and goodwill to all. You may recall in the last edition I mentioned we were welcoming some very special visitors to school this week as part of the Ashton Methodist Church Posada. You can see more of how their day was spent on page 3, but suffice to say all those who were in contact with our visitors had an opportunity to reflect on the purpose of their visit and will not forget their experience. When you look at the timetable of events for the day you will also have a good insight into a day in the life of an Ashton student; really quite revealing. Our SCAMPs programme continues to thrive and in this edition you will see how two new additions to the programme are faring. Running Club goes from strength to strength, with numbers increasing each week, see page 4 if you would like to join in. The SJA (St John Ambulance) unit also continues to thrive, with a committed group of staff and students working their way steadily through the training that will see them achieve a first aid qualification that may one day save a life. Truly remarkable determination to make a dif- ference to others can be seen every time that group meet. As we move into the final week of the school term, I would like to remind you one last time that tickets are still available for A Cosy Christmas, but they are selling fast. -

Page 1 Ribchester Road, Longridge Head Teacher: Paul Leaper E Mail
Ribchester Road, Longridge Head Teacher: Paul Leaper E Mail: [email protected] Preston, PR3 3XB Telephone: (01772) 782205 Website: www.hillside.lancsngfl.ac.uk ………………………………………………………………………………………………………………………………………………………… Dear Parents/Carers WE HAVE EXCITING NEWS! We have been successful in being shortlisted for this year’s Rock FM Schools Challenge. The challenge is quite simple, starting today 10 March we have 4 weeks to raise as much money as we can for school. For every pound that we raise Rock FM will match it (up to £2000) and the school that raise the biggest total will get an additional £1000. SO……although we already have planned events this month eg Craft Fair, Bags2school, non-uniform days, April 50/50 club draw, Autism Awareness Day, donations can also be made in the following ways: 1. Hillside has been provided with a personalized electronic fundraising page: https://www.cashforkidsgive.co.uk/campaign/lancashire-schools-challenge-2019/fundraisers/hillside- specialist-school-and-college/ 2. Money can be donated from other sponsored events. If you have any weird and wonderful ideas that you could raise additional funds for school there is an additional £250 cash incentive from Rock FM for: The most creative fundraising idea Best use of social media Teamwork Best PR Any way you can raise extra funds for us would be much appreciated – even if we don’t win the overall prize every pound donated will be matched by Rock FM. Although we would encourage everyone to try and get involved there are rules we must adhere to in regards to fundraising: No street collections or flyers on cars No collections to take place on private property without written permission of the proprietor Pledges received after the end date will not be counted Money is encouraged to be paid via the online fundraising page All money will have to be paid to us by 29 March so we can pay it into our account by the deadline date. -

St Mary's Catholic High School Unavoidable School Closure Policy
St Mary’s Catholic High School Unavoidable School Closure Policy Created: Sept 15 Review by: September 2020 Photo Extreme/unpredictable weather may impact on the School's ability to remain open to pupils and/or employees. If the Governing Body decides that it is necessary to close the school either to pupils or employees, employees will be notified at the earliest opportunity. A decision may be taken to close the school to pupils, but remain open for employees. In such cases, employees will be expected to attend work, unless otherwise notified by the Headteacher/Senior Leadership Team. If you do not hear – assume the school is open. The Site Supervisor on arrival at school contacts the Headteacher. A decision to close for any reason will be taken by the Headteacher as early as possible. The Headteacher will contact members of the School Emergency Team. The following system will then follow: The Headteacher contacts members of the Chair of Governors The Headteacher upon confirmation for the CofC will contact SLT, who will cascade the information. The Business Manager informs parents via school communication system The Network Manager updates the school website status. The Headteacher contacts Liaison and Compliance Officer on: (01772) 531808; (01772) 531893;(01772) 532805; (01772) 531694; (01772) 531494 Via the team mailbox [email protected] An NUC/1 (available via the link below) form is completed for all closures. If notification of closure is completed via the schools portal on the school calendar, further submission of an NUC/1 is not necessary. Link to: https://schoolsportal.lancsngfl.ac.uk/sp_atoz/service.asp?u_id=2189&strSL= 1 W:\SLT\LSM Policies\Health & Safety\Unavoidable School Closure.docx Last Reviewed: September 2018 The Headteacher contacts local radio stations stating:- • School Name • District No/School No (07/102) • DfES No (8885407) • Caller’s name and contact telephone number • Password ‘@@@@@@’ • If known that closure is 24 hrs and then this should be stated, otherwise procedure repeated on a daily basis. -

Multi Agency Flood Plan for Lancashire and the Ribble Valley ‘District Emergency Plan’
Ribble Valley Flood1. Plan Date 1st May 2018 Current Version Version 1.5.18 – PUBLIC Review Date May 2020 Document Control First amendment Due May 2019 Plan Prepared by Chris Shuttleworth, Ribble Valley BC EMERGENCY CALL CENTRE 24-hour telephone 01200 444448 Version 1.5.18 Uncontrolled if printed (1 of 69) Ribble Valley Flood Plan INFORMATION Ctrl + Click on link to page numbers CONTENTS FOREWORD ................................................................................................................................................ 3 AIM OF THE PLAN .............................................................................................................................. 3 OBJECTIVES OF THE PLAN .............................................................................................................. 3 OWNERSHIP ....................................................................................................................................... 4 CIRCULATION ..................................................................................................................................... 4 VERSION CONTROL, AND RECORD OF REVISIONS ..................................................................... 4 EXERCISES AND TESTING ............................................................................................................... 5 TRIGGERS FOR PLAN ACTIVATION (SCOPE) ................................................................................ 5 INCIDENT CONTROL ROOMS .......................................................................................................... -

Maps Aim to Ease Traffic
A 4-star council Awarded top marks by the Audit Commission August 2006 Providing • education • highways • trading standards • social services New 007 mission Stop that cheat Summer fun Tomorrow’s world Young agents Fraudbusters to stamp Scores of exciting Fascinating poll sign up for out the swindle that activities in our points way to the reading skills adds £££s to Council Tax new listing guide services you need Page 3 Page 3 Page 4 Back page Maps aim to GREEN LIGHT ease traffic A NEW route plan- ning system designed specifically for HGV drivers has been introduced by FOR CHILDREN Lancashire County Council in the hope of reducing congestion on county roads. Children’s The free-to-use Lancashire County Council website highlights the loca- centre tion of low-headroom bridges and other bridges with width or weight go-ahead restrictions. Until now, hauliers have found it difficult to plan will take routes without knowledge of these restrictions. Coming across such a county’s bridge can mean that the lorry driver has to reverse and find an alternative total to 61 route – causing nuisance for everyone else. The maps can be viewed - the most by going to www.lan- cashire.gov.uk and open- ing the “Maps of in the Lancashire” option. Select the map category TRANS- PORTATION and click on entire “hauliers’ information”. zDECISION: County Councillor Marcus Johnstone is pictured with Karrie Hudson at Whitegate Children’s Centre in Padiham. nation Taste of More than 30 new children’s centres will soon be open. success Children’s centres SCHOOL catering PARENTS and young chil- staff in Lancashire in your area dren are to benefit from 31 have landed con- new Children’s Centres tracts to provide din- Burnley - has four. -

Application Form
Leyland Community Radio licence application form 1. Station Name Guidance Notes What is the proposed station name? This is the name you expect to use to identify the station on air. Leyland Community Radio 2. Community to be served Guidance Notes Define the community or communities you are It is a legislative requirement that a service is intended proposing to serve. Drawing from various sources of primarily to serve one or more communities (whether or data (e.g. from the Office of Population, Census and not it also serves other members of the public) and we Survey) and in relation to your proposed coverage need to understand who comprises that community or area, please determine the size of the population communities. The target community will also be concerned and the make-up of the population as a specified in the licence, if this application is successful. whole, along with any relevant socio-economic The legislation defines a ‘community’ as: people who live information that would support your application. or work or undergo education or training in a particular (Please tell us the sources of the information you area or locality, or people who have one or more provide.) interests or characteristics in common. Answer in fewer than 300 words: Leyland Community Radio will serve everyone living, working or undergoing education or training in the Leyland area. The main settlement is Leyland, the rest of the geographical area comprising smaller towns and villages, employment zones, and a rural area. The community also extends to other parts of South Ribble. Of these, Bamber Bridge West, Lostock Hall, and the Charnock/Middleforth wards of Penwortham lie within the southernmost part of Preston- based Citybeat’s area (<12% of its potential listeners). -

England, Scotland, Wales and Ireland AM Transmitters
England, Scotland, Wales and Ireland AM Transmitters Frequency Finder kHz Area Station Broadcaster Format kW Transmitter Site Grid 153 Europe (night-time) Radio Algerienne Chaine 1 Algeria Arabic 2000.000 Bechar 162 England & Wales (d), Europe (n) Timing service (phase shift keyed) France No audio 800.000 Allouis 171 Europe (night-time) Medi 1 Morocco Arabic and French 1600.000 Nador 183 South East (d), Europe (n) Europe 1 (French) Germany French Talk 2000.000 Felsberg 189 Europe (night-time) Rikistuvarpid 1/2 Iceland Icelandic Various 300.000 Gufushaler, Iceland 198 England & Wales Radio 4 (Long Wave) BBC Talk, News, Entertainment 500.000 Droitwich SO 929 663 198 Northern Scotland Radio 4 (Long Wave) BBC Talk, News, Entertainment 50.000 Burghead NJ 125 685 198 Central and South Scotland Radio 4 (Long Wave) BBC Talk, News, Entertainment 50.000 Westerglen NS 868 773 207 Europe (night-time) Rikistuvarpid 1/2 Iceland Icelandic Various 100.000 Eidar, Iceland 207 Europe (night-time) Radio Marcaine Morocco Arabic 400.000 Azilal 216 Europe (night-time) RMC Info Monaco French News 1400.000 Roumoules, France 225 Europe (night-time) Polskie Radio Poland Polish 1000.000 Solec-Kujawski 234 South East (d), Europe (n) RTL Radio (French) Luxembourg French Talk 2000.000 Junglinster 243 East Coast (d) Limited Hours Danmarks Radio part time Denmark News and Weather 150.000 Kalundborg 252 Ire, Scot, Wales, N,C,W Engl RTE Radio 1 RTE Talk, Soft, Easy, Irish &Country 300.000 Kilmessan 252 Europe (night-time) Radio Algerienne Chaine 3 Algeria French 1500.000