The Genetics of Primary Dystonias and Related Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
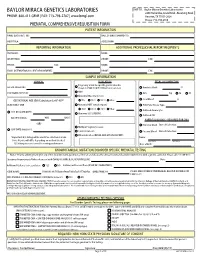
Prenatal Testing Requisition Form
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 PRENATAL COMPREHENSIVE REQUISITION FORM PATIENT INFORMATION NAME (LAST,FIRST, MI): DATE OF BIRTH (MM/DD/YY): HOSPITAL#: ACCESSION#: REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: SAMPLE INFORMATION CLINICAL INDICATION FETAL SPECIMEN TYPE Pregnancy at risk for specific genetic disorder DATE OF COLLECTION: (Complete FAMILIAL MUTATION information below) Amniotic Fluid: cc AMA PERFORMING PHYSICIAN: CVS: mg TA TC Abnormal Maternal Screen: Fetal Blood: cc GESTATIONAL AGE (GA) Calculation for AF-AFP* NTD TRI 21 TRI 18 Other: SELECT ONLY ONE: Abnormal NIPT (attach report): POC/Fetal Tissue, Type: TRI 21 TRI 13 TRI 18 Other: Cultured Amniocytes U/S DATE (MM/DD/YY): Abnormal U/S (SPECIFY): Cultured CVS GA ON U/S DATE: WKS DAYS PARENTAL BLOODS - REQUIRED FOR CMA -OR- Maternal Blood Date of Collection: Multiple Pregnancy Losses LMP DATE (MM/DD/YY): Parental Concern Paternal Blood Date of Collection: Other Indication (DETAIL AND ATTACH REPORT): *Important: U/S dating will be used if no selection is made. Name: Note: Results will differ depending on method checked. Last Name First Name U/S dating increases overall screening performance. Date of Birth: KNOWN FAMILIAL MUTATION/DISORDER SPECIFIC PRENATAL TESTING Notice: Prior to ordering testing for any of the disorders listed, you must call the lab and discuss the clinical history and sample requirements with a genetic counselor. -

Candidate Chromosome 1 Disease Susceptibility Genes for Sjogren's Syndrome Xerostomia Are Narrowed by Novel NOD.B10 Congenic Mice P
Donald and Barbara Zucker School of Medicine Journal Articles Academic Works 2014 Candidate chromosome 1 disease susceptibility genes for Sjogren's syndrome xerostomia are narrowed by novel NOD.B10 congenic mice P. K. A. Mongini Zucker School of Medicine at Hofstra/Northwell J. M. Kramer Northwell Health T. Ishikawa H. Herschman D. Esposito Follow this and additional works at: https://academicworks.medicine.hofstra.edu/articles Part of the Medical Molecular Biology Commons Recommended Citation Mongini P, Kramer J, Ishikawa T, Herschman H, Esposito D. Candidate chromosome 1 disease susceptibility genes for Sjogren's syndrome xerostomia are narrowed by novel NOD.B10 congenic mice. 2014 Jan 01; 153(1):Article 2861 [ p.]. Available from: https://academicworks.medicine.hofstra.edu/articles/2861. Free full text article. This Article is brought to you for free and open access by Donald and Barbara Zucker School of Medicine Academic Works. It has been accepted for inclusion in Journal Articles by an authorized administrator of Donald and Barbara Zucker School of Medicine Academic Works. For more information, please contact [email protected]. NIH Public Access Author Manuscript Clin Immunol. Author manuscript; available in PMC 2015 July 01. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: Clin Immunol. 2014 July ; 153(1): 79–90. doi:10.1016/j.clim.2014.03.012. Candidate chromosome 1 disease susceptibility genes for Sjogren’s syndrome xerostomia are narrowed by novel NOD.B10 congenic mice Patricia K. A. Monginia and Jill M. Kramera,1 Tomo-o Ishikawab,2 and Harvey Herschmanb Donna Espositoc aThe Feinstein Institute for Medical Research North Shore-Long Island Jewish Health System 350 Community Drive Manhasset, NY 11030 bDavid Geffen School of Medicine at UCLA 341 Boyer Hall (MBI) 611 Charles E. -

NGS Panels 2020
NGS Panels 2020 BENEFIT FROM OUR MEDICAL EXPERTISE AND STREAMLINED GENETIC TESTING NGS Panels 2020 Benefit from our Medical Expertise and Streamlined Genetic Testing CENTOGENE is fully committed to bringing the best possible diagnostic solutions to our patients and their families. We always strive to incorporate the latest in-house findings and medical research in our products to improve and ease the diagnostic odyssey of rare disease patients. To reflect the fast-growing knowledge of complex associations of genes with diseases as well as to maximize clinical sensitivity, we have updated and significantly redesigned our Next Generation Sequencing (NGS) gene panels. The gene composition of each panel has been revised to meet the latest gene discoveries as well as to provide the highest clinical validity. Additionally, we have minimized complexity and removed redundancy in the panel portfolio by creating phenotype-directed diagnostic panels, which are the most comprehensive and include all relevant genes necessary for differential diagnosis of syndromes with overlapping phenotype, therefore allowing the diagnosis of diseases that otherwise would be missed. This principle increases the clinical utility, de-risks panel choice, increases cost-effectiveness, and ultimately simplifies the diagnostic process. When choosing one of our NGS panels, feel confident that you will receive high-quality sequencing combined with best data analysis and interpretation, which are documented in comprehensive medical reports. As always, CENTOGENE and our Customer -

Human Social Genomics in the Multi-Ethnic Study of Atherosclerosis
Getting “Under the Skin”: Human Social Genomics in the Multi-Ethnic Study of Atherosclerosis by Kristen Monét Brown A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Epidemiological Science) in the University of Michigan 2017 Doctoral Committee: Professor Ana V. Diez-Roux, Co-Chair, Drexel University Professor Sharon R. Kardia, Co-Chair Professor Bhramar Mukherjee Assistant Professor Belinda Needham Assistant Professor Jennifer A. Smith © Kristen Monét Brown, 2017 [email protected] ORCID iD: 0000-0002-9955-0568 Dedication I dedicate this dissertation to my grandmother, Gertrude Delores Hampton. Nanny, no one wanted to see me become “Dr. Brown” more than you. I know that you are standing over the bannister of heaven smiling and beaming with pride. I love you more than my words could ever fully express. ii Acknowledgements First, I give honor to God, who is the head of my life. Truly, without Him, none of this would be possible. Countless times throughout this doctoral journey I have relied my favorite scripture, “And we know that all things work together for good, to them that love God, to them who are called according to His purpose (Romans 8:28).” Secondly, I acknowledge my parents, James and Marilyn Brown. From an early age, you two instilled in me the value of education and have been my biggest cheerleaders throughout my entire life. I thank you for your unconditional love, encouragement, sacrifices, and support. I would not be here today without you. I truly thank God that out of the all of the people in the world that He could have chosen to be my parents, that He chose the two of you. -

Genetic Testing Medical Policy – Genetics
Genetic Testing Medical Policy – Genetics Please complete all appropriate questions fully. Suggested medical record documentation: • Current History & Physical • Progress Notes • Family Genetic History • Genetic Counseling Evaluation *Failure to include suggested medical record documentation may result in delay or possible denial of request. PATIENT INFORMATION Name: Member ID: Group ID: PROCEDURE INFORMATION Genetic Counseling performed: c Yes c No **Please check the requested analyte(s), identify number of units requested, and provide indication/rationale for testing. 81400 Molecular Pathology Level 1 Units _____ c ACADM (acyl-CoA dehydrogenase, C-4 to C-12 straight chain, MCAD) (e.g., medium chain acyl dehydrogenase deficiency), K304E variant _____ c ACE (angiotensin converting enzyme) (e.g., hereditary blood pressure regulation), insertion/deletion variant _____ c AGTR1 (angiotensin II receptor, type 1) (e.g., essential hypertension), 1166A>C variant _____ c BCKDHA (branched chain keto acid dehydrogenase E1, alpha polypeptide) (e.g., maple syrup urine disease, type 1A), Y438N variant _____ c CCR5 (chemokine C-C motif receptor 5) (e.g., HIV resistance), 32-bp deletion mutation/794 825del32 deletion _____ c CLRN1 (clarin 1) (e.g., Usher syndrome, type 3), N48K variant _____ c DPYD (dihydropyrimidine dehydrogenase) (e.g., 5-fluorouracil/5-FU and capecitabine drug metabolism), IVS14+1G>A variant _____ c F13B (coagulation factor XIII, B polypeptide) (e.g., hereditary hypercoagulability), V34L variant _____ c F2 (coagulation factor 2) (e.g., -

Proquest Dissertations
mn u Ottawa l.'Univcrsilc can.ifficn/ic Canada's university FACULTE DES ETUDES SUPERIEURES 11=1 FACULTY OF GRADUATE AND ET POSTOCTORALES U Ottawa POSDOCTORAL STUDIES L'Urriversittf canadienne (Canada's university Fabin Han AUTEUR DE LA THESE / AUTHOR OF THESIS Ph.D. (Microbiology and Immunology) GRADE/DEGREE Department of Biochemistry, Microbiology and Immunology Characterization of the Genes for Myoclonus-Dystonia TITRE DE LA THESE / TITLE OF THESIS Dennis Bulman EXAMINATEURS (EXAMINATRICES) DE LA THESE /THESIS EXAMINERS John Bell Peter Ray Robert Korneluk Catherine Tsilfidis Gary W. Slater. Le Doyen de la Faculte des etudes superieures et postdoctorales / Dean of the Faculty of Graduate and Postdoctoral Studies Characterization of the Genes for Myoclonus-Dystonia By Fabin Han Thesis Submitted to the School of Graduate Studies in Partial Fulfillment of the Requirements for the Degree of Doctorate of Philosophy Department of Biochemistry, Microbiology and Immunology, Graduate Collaborative Program in Human and Molecular Genetics, Faculty of Medicine University of Ottawa Copyright by Fabin Han, 2007 Ottawa, Canada Library and Bibliotheque et 1*1 Archives Canada Archives Canada Published Heritage Direction du Branch Patrimoine de I'edition 395 Wellington Street 395, rue Wellington Ottawa ON K1A0N4 Ottawa ON K1A0N4 Canada Canada Your file Votre reference ISBN: 978-0-494-49354-0 Our file Notre reference ISBN: 978-0-494-49354-0 NOTICE: AVIS: The author has granted a non L'auteur a accorde une licence non exclusive exclusive license allowing -

TOR1A Gene Torsin Family 1 Member A
TOR1A gene torsin family 1 member A Normal Function The TOR1A gene (also known as DYT1) provides instructions for making a protein called torsinA. This protein is found in the space between two neighboring structures within cells, the nuclear envelope and the endoplasmic reticulum. The nuclear envelope surrounds the nucleus and separates it from the rest of the cell. The endoplasmic reticulum processes proteins and other molecules and helps transport them to specific destinations either inside or outside the cell. Although little is known about the function of torsinA, studies suggest that it may help process and transport other proteins. TorsinA may also participate in the movement of membranes associated with the nuclear envelope and endoplasmic reticulum. TorsinA is active in many of the body's tissues, and it is particularly important for the normal function of nerve cells in the brain. For example, researchers have found high levels of torsinA in a part of the brain called the substantia nigra. This region contains nerve cells that produce dopamine, a chemical messenger that transmits signals within the brain to produce smooth physical movements. Health Conditions Related to Genetic Changes Early-onset primary dystonia A particular mutation in the TOR1A gene causes most cases of early-onset primary dystonia. This mutation, which is often called the GAG deletion or delta GAG, deletes three DNA building blocks (base pairs) from the TOR1A gene. The resulting torsinA protein is missing one protein building block (amino acid) in a critical region. The altered protein's effect on the function of nerve cells in the brain is unclear. -

Using Zebrafish As a Model System for Dyt1 Dystonia
USING ZEBRAFISH AS A MODEL SYSTEM FOR DYT1 DYSTONIA by Jonathan Sager BS, University of Wisconsin - Oshkosh, 2006 Submitted to the Graduate Faculty of Neurobiology in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Pittsburgh 2012 UNIVERSITY OF PITTSBURGH SCHOOL OF MEDICINE This dissertation was presented by Jonathan Sager It was defended on June 12th, 2012 And approved by A. Paula Monaghan-Nichols, PhD, Neurobiology Neil A. Hukriede, PhD, Microbiology and Molecular genetics Edward A. Burton, MD DPhil FRCP, Neurology Laurie Ozelius, PhD, Genetics and Genomic Sciences, Mount Sinai Hospital Committee Chair: Laura E. Lillien, PhD, Neurobiology Dissertation Advisor: Gonzalo E. Torres, PhD, Neurobiology ii Copyright © by Jonathan Sager 2012 iii USING ZEBRAFISH AS A MODEL SYSTEM FOR DYT1 DYSTONIA Jonathan Sager University of Pittsburgh, 2012 Dystonia is characterized by sustained involuntary muscle contractions producing repetitive twisting movements and abnormal postures. DYT1 dystonia, an early-onset primary dystonia, is caused by a trinucleotide deletion in the TOR1A gene, resulting in the loss of a single glutamic acid in the TorsinA protein. It is unknown how this mutation causes dysfunction of CNS motor circuits resulting in dystonia. The aims of this work were: (i) characterize the zebrafish homolog of human TOR1A in order to elucidate the functions of Torsins in vivo; (ii) generate transgenic zebrafish models of DYT1 dystonia suitable for mechanistic and drug discovery studies. An ancestral tor1 gene found in the genomes of several fish species was duplicated at the root of the tetrapod lineage. In zebrafish, tor1 is expressed as two isoforms with unique 5' exons. -

Transcriptional Regulators Are Upregulated in the Substantia Nigra
Journal of Emerging Investigators Transcriptional Regulators are Upregulated in the Substantia Nigra of Parkinson’s Disease Patients Marianne Cowherd1 and Inhan Lee2 1Community High School, Ann Arbor, MI 2miRcore, Ann Arbor, MI Summary neurological conditions is an established practice (3). Parkinson’s disease (PD) affects approximately 10 Significant gene expression dysregulation in the SN and million people worldwide with tremors, bradykinesia, in the striatum has been described, particularly decreased apathy, memory loss, and language issues. Though such expression in PD synapses. Protein degradation has symptoms are due to the loss of the substantia nigra (SN) been found to be upregulated (4). Mutations in SNCA brain region, the ultimate causes and complete pathology are unknown. To understand the global gene expression (5), LRRK2 (6), and GBA (6) have also been identified changes in SN, microarray expression data from the SN as familial markers of PD. SNCA encodes alpha- tissue of 9 controls and 16 PD patients were compared, synuclein, a protein found in presynaptic terminals that and significantly upregulated and downregulated may regulate vesicle presence and dopamine release. genes were identified. Among the upregulated genes, Eighteen SNCA mutations have been associated with a network of 33 interacting genes centered around the PD and, although the exact pathogenic mechanism is cAMP-response element binding protein (CREBBP) was not confirmed, mutated alpha-synuclein is the major found. The downstream effects of increased CREBBP- component of protein aggregates, called Lewy bodies, related transcription and the resulting protein levels that are often found in PD brains and may contribute may result in PD symptoms, making CREBBP a potential therapeutic target due to its central role in the interactive to cell death. -

Quantitative Trait Loci Mapping of Macrophage Atherogenic Phenotypes
QUANTITATIVE TRAIT LOCI MAPPING OF MACROPHAGE ATHEROGENIC PHENOTYPES BRIAN RITCHEY Bachelor of Science Biochemistry John Carroll University May 2009 submitted in partial fulfillment of requirements for the degree DOCTOR OF PHILOSOPHY IN CLINICAL AND BIOANALYTICAL CHEMISTRY at the CLEVELAND STATE UNIVERSITY December 2017 We hereby approve this thesis/dissertation for Brian Ritchey Candidate for the Doctor of Philosophy in Clinical-Bioanalytical Chemistry degree for the Department of Chemistry and the CLEVELAND STATE UNIVERSITY College of Graduate Studies by ______________________________ Date: _________ Dissertation Chairperson, Johnathan D. Smith, PhD Department of Cellular and Molecular Medicine, Cleveland Clinic ______________________________ Date: _________ Dissertation Committee member, David J. Anderson, PhD Department of Chemistry, Cleveland State University ______________________________ Date: _________ Dissertation Committee member, Baochuan Guo, PhD Department of Chemistry, Cleveland State University ______________________________ Date: _________ Dissertation Committee member, Stanley L. Hazen, MD PhD Department of Cellular and Molecular Medicine, Cleveland Clinic ______________________________ Date: _________ Dissertation Committee member, Renliang Zhang, MD PhD Department of Cellular and Molecular Medicine, Cleveland Clinic ______________________________ Date: _________ Dissertation Committee member, Aimin Zhou, PhD Department of Chemistry, Cleveland State University Date of Defense: October 23, 2017 DEDICATION I dedicate this work to my entire family. In particular, my brother Greg Ritchey, and most especially my father Dr. Michael Ritchey, without whose support none of this work would be possible. I am forever grateful to you for your devotion to me and our family. You are an eternal inspiration that will fuel me for the remainder of my life. I am extraordinarily lucky to have grown up in the family I did, which I will never forget. -

Multitarget Deep Brain Stimulation for Clinically Complex Movement Disorders
CASE REPORT Multitarget deep brain stimulation for clinically complex movement disorders Tariq Parker, MRCS, Ashley L. B. Raghu, BSc(Hons), James J. FitzGerald, FRCS(SN), Alexander L. Green, FRCS(SN), and Tipu Z. Aziz, FMedSci Oxford Functional Neurosurgery, Nuffield Department of Surgical Sciences, University of Oxford, United Kingdom Deep brain stimulation (DBS) of single-target nuclei has produced remarkable functional outcomes in a number of move- ment disorders such as Parkinson’s disease, essential tremor, and dystonia. While these benefits are well established, DBS efficacy and strategy for unusual, unclassified movement disorder syndromes is less clear. A strategy of dual pal- lidal and thalamic electrode placement is a rational approach in such cases where there is profound, medically refractory functional impairment. The authors report a series of such cases: midbrain cavernoma hemorrhage with olivary hyper- trophy, spinocerebellar ataxia-like disorder of probable genetic origin, Holmes tremor secondary to brainstem stroke, and hemiballismus due to traumatic thalamic hemorrhage, all treated by dual pallidal and thalamic DBS. All patients demon- strated robust benefit from DBS, maintained in long-term follow-up. This series demonstrates the flexibility and efficacy, but also the limitations, of dual thalamo-pallidal stimulation for managing axial and limb symptoms of tremors, dystonia, chorea, and hemiballismus in patients with complex movement disorders. https://thejns.org/doi/abs/10.3171/2019.11.JNS192224 KEYWORDS deep brain stimulation; dystonia; essential tremor; thalamus; globus pallidus; functional neurosurgery EEP brain stimulation (DBS) surgery for the treat- Her condition progressed to developing speech difficul- ment of movement disorders usually employs stim- ties, left-sided one-and-a-half syndrome, and a bilateral ulation at a single site in one or both hemispheres. -

The Dystonias
LE JOURNAL CANADIEN DES SCIENCES NEUROLOGIQUES SUBJECT REVIEW The Dystonias Edith G. McGeer and Patrick L. McGeer Can. J. Neurol. Sci. 1988; 15: 447-483 Contents This review is intended for both the practitioner and the sci entist. Its purpose is to summarize current knowledge regarding the various forms of dystonia, as well as the pathology known Introduction to produce the syndrome in specialized circumstances. Histopathological and brain imaging studies The low incidence of the disorder, its prolonged course, and the difficulty of accurate diagnosis has precluded the type of Sleep and other physiological studies systematic investigation that is possible with many other disor Chemical pathology ders. Yet such systematic investigation is essential if the myster Brain studies ies surrounding dystonia are to be unravelled and methods of CSF studies treatment improved. Blood studies Dystonia has been defined by the Scientific Advisory Board Urine studies of the Dystonia Medical Research Foundation as a syndrome of Fibroblast studies sustained muscle contraction, frequently causing twisting and Miscellaneous repetitive movements, or abnormal posture. It is a clinical term Therapy and not a disease description. It refers to all anatomical forms, whether they involve generalized musculature or only focal Iatrogenic dystonia groups. Although dystonia appears as part of the syndrome in a Possible animal models of dystonia number of disease states, it is idiopathic dystonia, where inheri Summary tance is a major factor, that has aroused the greatest medical interest. This review emphasizes recent literature and those aspects which may contribute to an understanding of the under 1. INTRODUCTION lying mechanisms of dystonic movement.