Connections of the Skull Bones. Temporomandibular Joint
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
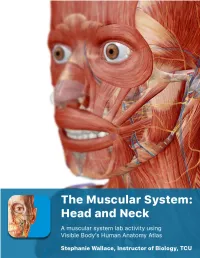
The Muscular System Views
1 PRE-LAB EXERCISES Before coming to lab, get familiar with a few muscle groups we’ll be exploring during lab. Using Visible Body’s Human Anatomy Atlas, go to the Views section. Under Systems, scroll down to the Muscular System views. Select the view Expression and find the following muscles. When you select a muscle, note the book icon in the content box. Selecting this icon allows you to read the muscle’s definition. 1. Occipitofrontalis (epicranius) 2. Orbicularis oculi 3. Orbicularis oris 4. Nasalis 5. Zygomaticus major Return to Muscular System views, select the view Head Rotation and find the following muscles. 1. Sternocleidomastoid 2. Scalene group (anterior, middle, posterior) 2 IN-LAB EXERCISES Use the following modules to guide your exploration of the head and neck region of the muscular system. As you explore the modules, locate the muscles on any charts, models, or specimen available. Please note that these muscles act on the head and neck – those that are located in the neck but act on the back are in a separate section. When reviewing the action of a muscle, it will be helpful to think about where the muscle is located and where the insertion is. Muscle physiology requires that a muscle will “pull” instead of “push” during contraction, and the insertion is the part that will move. Imagine that the muscle is “pulling” on the bone or tissue it is attached to at the insertion. Access 3D views and animated muscle actions in Visible Body’s Human Anatomy Atlas, which will be especially helpful to visualize muscle actions. -
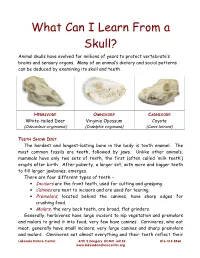
What Can I Learn from a Skull? Animal Skulls Have Evolved for Millions of Years to Protect Vertebrate’S Brains and Sensory Organs
What Can I Learn From a Skull? Animal skulls have evolved for millions of years to protect vertebrate’s brains and sensory organs. Many of an animal’s dietary and social patterns can be deduced by examining its skull and teeth. HERBIVORE OMNIVORE CARNIVORE White-tailed Deer Virginia Opossum Coyote (Odocoileus virginianus) (Didelphis virginiana) (Canis latrans) TEETH SHOW DIET . The hardest and longest-lasting bone in the body is tooth enamel. The most common fossils are teeth, followed by jaws. Unlike other animals, mammals have only two sets of teeth, the first (often called ‘milk teeth’) erupts after birth. After puberty, a larger set, with more and bigger teeth to fill larger jawbones, emerges. There are four different types of teeth – • Incisors are the front teeth, used for cutting and grasping. • Canines are next to incisors and are used for tearing. • Premolars , located behind the canines, have sharp edges for crushing food. • Molars , the very back teeth, are broad, flat grinders. Generally, herbivores have large incisors to nip vegetation and premolars and molars to grind it into food; very few have canines. Carnivores, who eat meat, generally have small incisors, very large canines and sharp premolars and molars. Omnivores eat almost everything and their teeth reflect their Lakeside Nature Center 4701 E Gregory, KCMO 64132 816-513-8960 www.lakesidenaturecenter.org preferences; they have all four types of teeth. In fact, if you’d like to see an excellent example of an omnivore’s teeth, look in the mirror. EYE PLACEMENT IDENTIFIES PREDATORS . Carnivores generally have large eyes, placed so that the eyes look forward and the areas of vision of the two eyes overlap. -

Applied Anatomy of the Temporomandibular Joint
Applied anatomy of the temporomandibular joint CHAPTER CONTENTS process which, together with the temporal process of the zygo- Bones . e198 matic bone, forms the zygomatic arch (Fig. 1). The midline fusion of the left and right mandibular bodies Joint .capsule .and .ligaments . e198 provides a connection between the two temporomandibular Intra-articular .meniscus . e198 joints, so that movement in one joint always influences the opposite one. Nociceptive .innervation . e199 Muscles .and .tendons . e199 Joint capsule and ligaments Biomechanical .aspects . e200 Forward movement of the mandible . e200 The joint capsule is wide and loose on the upper aspect around Opening and closing the mouth. e200 the mandibular fossa. Distally, it diminishes in a funnel shaped Grinding movements . e200 manner to become attached to the mandibular neck (Fig. 2). Nerves .and .blood .vessels . e200 Its laxity prevents rupture even after dislocation. Laterally and medially, a local reinforcement of the joint capsule is found. The lateral collateral ligament courses from The temporomandibular joint (TMJ) is sited at the base of the the zygomatic arch obliquely downwards and backwards skull and formed by parts of the mandible and the temporal towards the posterior rim of the mandibular neck, lateral to bone, separated by an intra-articular meniscus. It is a synovial the outer aspect of the capsule. At its posterior aspect, it is in joint capable of both hinge (rotation) and sliding (translatory) close relation to the joint capsule and prevents the joint from movements. Like other synovial joints, it may be affected by opening widely. Medially, the joint capsule is locally reinforced internal derangement, inflammatory arthritis, arthrosis, and by the medial collateral ligament. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Innervation of the Temporomandibular Joint Can Be Discussed It Is Necessary First to Describe Its Embryology, Gfoss Anatomy and Microscopic Appe¿Ìrance
à8.ì 'R? INNERVATION OF THE TEMPOROMAI\DIBULAR J AN EXPERIMENTAL AMMAL MODEL USING AUSTRALIAN MERINO STIEEP ABDOLGHAFAR TAHMASEBI-SARVESTANI' B. Sc, M. Sc Thesis submitted for the degree of DOCTOR OF PHILOSOPHY In The Department of Anatomical Sciences The University of Adelaide (Faculty of Medicine)' Adelaide, South Australia, 5005 April, L997 tfüs tñesisis [elicatelø nl wtfe Aggñleñ ø¡tlour g4.arzi"e tfr.re e c friûfren Ía fiera ñ, fo zic ñ atú fi l-1 ACKNOWLEDGMENTS I am greatly indebted to my supervisors Dr. Ray Tedman and Professor Alastair Goss who first inrroduced me to this freld of study and providing me with the opportunity to carry out this work. I wish to thank them for their constant interest and guidance throughout the course of this study. I am also indebted to the scholarship committee of the Shiraz Medical Science University and Ministry of Health and Medical Education, Iran for gânting me a 4 year scholarship to study at the Universiry of Adelaide. I thank professor Goss and the Japanese Surgical Research team for their expertise in surgical animal models, and Professor July Polak and Dr Mika Hukkanen, Royal postgraduate Medical School London University for their expertise in immunohistochemistry and for providing some of the antisera used in the neuropeptide studies. I would also like to thank Professor Ian Gibbins, Department of Anatomy and Histology of the Flinders Medical Centre for, without the use of his laboratories, materials, and expertise, the double and triple labelling parts of the immunocytochemical work would not have occurred. I also orwe many thanks to Susan Matthew, a senior laboratory officer for her skilful technical assistance in double and triple immunocytochemistry. -

Diagnosis and Treatment of Temporomandibular Disorders ROBERT L
Diagnosis and Treatment of Temporomandibular Disorders ROBERT L. GAUER, MD, and MICHAEL J. SEMIDEY, DMD, Womack Army Medical Center, Fort Bragg, North Carolina Temporomandibular disorders (TMD) are a heterogeneous group of musculoskeletal and neuromuscular conditions involving the temporomandibular joint complex, and surrounding musculature and osseous components. TMD affects up to 15% of adults, with a peak incidence at 20 to 40 years of age. TMD is classified asintra-articular or extra- articular. Common symptoms include jaw pain or dysfunction, earache, headache, and facial pain. The etiology of TMD is multifactorial and includes biologic, environmental, social, emotional, and cognitive triggers. Diagnosis is most often based on history and physical examination. Diagnostic imaging may be beneficial when malocclusion or intra-articular abnormalities are suspected. Most patients improve with a combination of noninvasive therapies, including patient education, self-care, cognitive behavior therapy, pharmacotherapy, physical therapy, and occlusal devices. Nonsteroidal anti-inflammatory drugs and muscle relaxants are recommended initially, and benzodiazepines or antidepressants may be added for chronic cases. Referral to an oral and maxillofacial surgeon is indicated for refrac- tory cases. (Am Fam Physician. 2015;91(6):378-386. Copyright © 2015 American Academy of Family Physicians.) More online he temporomandibular joint (TMJ) emotional, and cognitive triggers. Factors at http://www. is formed by the mandibular con- consistently associated with TMD include aafp.org/afp. dyle inserting into the mandibular other pain conditions (e.g., chronic head- CME This clinical content fossa of the temporal bone. Muscles aches), fibromyalgia, autoimmune disor- conforms to AAFP criteria Tof mastication are primarily responsible for ders, sleep apnea, and psychiatric illness.1,3 for continuing medical education (CME). -

Diagnosing and Treating Trigeminal Neuralgia in General Dentistry
general practice feature Chasing Pain Diagnosing and Treating Trigeminal Neuralgia in General Dentistry by Steven Olmos, DDS, DABCP, DABCDSM, DABDSM, DAAPM, FAAOP, FAACP, FICCMO, FADI, FIAO As dentists, we know quite a bit about tooth and gum pain, but when it comes to chronic facial pain and neuropathic pain, our dental school education leaves us unprepared. The objective of this article is to explain the differences between men and women with chronic orofacial pain and the relationship to proper functional breathing, using a case study as demonstration. 34 JANUARY 2016 // dentaltown.com general practice feature the United States, nearly half research published in Chest 2015 demonstrates that of all adults lived with chronic respiratory-effort-related arousal may be the most pain in 2011. Of 353,000 adults likely cause (nasal obstruction or mouth breath- 11 aged 18 years or older who were ing). Rising C02 (hypercapnia) in a patient with a surveyed by Gallup-Health- sleep-breathing disorder (including mouth breath- ways, 47 percent reported having at least one of ing) specifically stimulates the superficial masseter three types of chronic pain: neck or back pain, muscles to contract.12 knee or leg pain, or recurring pain.2 Identifying the structural area of obstruction A study published in The Journal of the Amer- (Four Points of Obstruction; Fig. 1) of the air- ican Dental Association October 2015 stated: way will insure the most effective treatment for a “One in six patients visiting a general dentist had sleep-breathing disorder and effectively reduce the experienced orofacial pain during the last year. -

MRI-Based Assessment of Masticatory Muscle Changes in TMD Patients After Whiplash Injury
Journal of Clinical Medicine Article MRI-Based Assessment of Masticatory Muscle Changes in TMD Patients after Whiplash Injury Yeon-Hee Lee 1,* , Kyung Mi Lee 2 and Q-Schick Auh 1 1 Department of Orofacial Pain and Oral Medicine, Kyung Hee University Dental Hospital, #613 Hoegi-dong, Dongdaemun-gu, Seoul 02447, Korea; [email protected] 2 Department of Radiology, Kyung Hee University College of Medicine, Kyung Hee University Hospital, #26 Kyunghee-daero, Dongdaemun-gu, Seoul 02447, Korea; [email protected] * Correspondence: [email protected]; Tel.: +82-2-958-9409; Fax: +82-2-968-0588 Abstract: Objective: to investigate the change in volume and signal in the masticatory muscles and temporomandibular joint (TMJ) of patients with temporomandibular disorder (TMD) after whiplash injury, based on magnetic resonance imaging (MRI), and to correlate them with other clinical parameters. Methods: ninety patients (64 women, 26 men; mean age: 39.36 ± 15.40 years), including 45 patients with symptoms of TMD after whiplash injury (wTMD), and 45 age- and sex- matched controls with TMD due to idiopathic causes (iTMD) were included. TMD was diagnosed using the study diagnostic criteria for TMD Axis I, and MRI findings of the TMJ and masticatory muscles were investigated. To evaluate the severity of TMD pain and muscle tenderness, we used a visual analog scale (VAS), palpation index (PI), and neck PI. Results: TMD indexes, including VAS, PI, and neck PI were significantly higher in the wTMD group. In the wTMD group, muscle tenderness was highest in the masseter muscle (71.1%), and muscle tenderness in the temporalis (60.0%), lateral pterygoid muscle (LPM) (22.2%), and medial pterygoid muscle (15.6%) was significantly more frequent than that in the iTMD group (all p < 0.05). -

Orofacial Pain Caused by Trigeminal Neuralgia And/Or Temporomandibular Joint Disorder
PERIODICUM BIOLOGORUM UDC 57:61 VOL. 115, No 2, 185–189, 2013 CODEN PDBIAD ISSN 0031-5362 Original scientific paper Orofacial pain caused by trigeminal neuralgia and/or temporomandibular joint disorder Abstract TOMISLAV BADEL1 IVANA SAVI] PAVI^IN2 Background and Purpose: The purpose was to evaluate an accurate VANJA BA[I] KES3 method of differentiating between temporomandibular joint (TMJ) dis- IRIS ZAVOREO3 4 order and trigeminal neuralgia (TN) in the sample of patients from a DIJANA ZADRAVEC subspecialist dental practice. JOSIPA KERN5 Patients and Methods: Patients (n=239, mean age 39.3 years, 83.3% 1 Department of Removable Prosthodontics, female) were examined for clinical symptoms and signs of orofacial pain of School of Dental Medicine, non-dental origin. The study included 12 female patients (group G-1; mean University of Zagreb, Gunduli}eva 5, 10000 Zagreb, Croatia age 60.3 years) with determined co-morbidity of TMJ disorder and TN, and 17 patients (group G-2; mean age 53.8 years, 64.7% female) with only TN 2Department of Dental Anthropology, confirmed and the TMJ disorder ruled out. The TMJ diagnosis by means of School of Dental Medicine magnetic resonance imaging (MRI) was confirmed. Pain intensity was University of Zagreb, Gunduli}eva 5, 10000 Zagreb, Croatia rated on a visual-analogue scale (VAS with range 0–10) and maximal mouth opening capacity (mm) measured by gauge. 3 Department of Neurology, Clinical Hospital Results: TMJ pain on the VAS scale for G-1 patients amounted to 6.91. Centre “Sisters of Charity”University of Zagreb, Vinogradska cesta 29, TN related pain symptoms on the VAS scale for G-1 patients amounted to 10000 Zagreb, Croatia 9.0±1.6 and for G-2 patients 8.1±2.7. -

6. the Pharynx the Pharynx, Which Forms the Upper Part of the Digestive Tract, Consists of Three Parts: the Nasopharynx, the Oropharynx and the Laryngopharynx
6. The Pharynx The pharynx, which forms the upper part of the digestive tract, consists of three parts: the nasopharynx, the oropharynx and the laryngopharynx. The principle object of this dissection is to observe the pharyngeal constrictors that form the back wall of the vocal tract. Because the cadaver is lying face down, we will consider these muscles from the back. Figure 6.1 shows their location. stylopharyngeus suuperior phayngeal constrictor mandible medial hyoid bone phayngeal constrictor inferior phayngeal constrictor Figure 6.1. Posterior view of the muscles of the pharynx. Each of the three pharyngeal constrictors has a left and right part that interdigitate (join in fingerlike branches) in the midline, forming a raphe, or union. This raphe forms the back wall of the pharynx. The superior pharyngeal constrictor is largely in the nasopharynx. It has several origins (some texts regard it as more than one muscle) one of which is the medial pterygoid plate. It assists in the constriction of the nasopharynx, but has little role in speech production other than helping form a site against which the velum may be pulled when forming a velic closure. The medial pharyngeal constrictor, which originates on the greater horn of the hyoid bone, also has little function in speech. To some extent it can be considered as an elevator of the hyoid bone, but its most important role for speech is simply as the back wall of the vocal tract. The inferior pharyngeal constrictor also performs this function, but plays a more important role constricting the pharynx in the formation of pharyngeal consonants. -

Giant Cell Arteritis Misdiagnosed As Temporomandibular Disorder: a Case Report and Review of the Literature
360_Reiter.qxp 10/14/09 3:17 PM Page 360 Giant Cell Arteritis Misdiagnosed as Temporomandibular Disorder: A Case Report and Review of the Literature Shoshana Reiter, DMD Giant cell arteritis (GCA) is a systemic vasculitis involving medium Teacher and large-sized arteries, most commonly the extracranial branches Department of Oral Rehabilitation of the carotid artery. Early diagnosis and treatment are essential to avoid severe complications. This article reports on a GCA case Ephraim Winocur, DMD and discusses how the orofacial manifestations of GCA can lead to Lecturer misdiagnosis of GCA as temporomandibular disorder. GCA Department of Oral Rehabilitation should be included in the differential diagnosis of orofacial pain in Carole Goldsmith, DMD the elderly based on the knowledge of related signs and symptoms, Instructor mainly jaw claudication, hard end-feel limitation of range of Department of Oral Rehabilitation motion, and temporal headache. J OROFAC PAIN 2009;23:360–365 Alona Emodi-Perlman, DMD Key words: Giant cell arteritis, jaw claudication, Teacher temporomandibular disorders, trismus Department of Oral Rehabilitation Meir Gorsky, DMD Professor Department of Oral Pathology and Oral iant cell arteritis (GCA) is a systemic vasculitis involving Medicine the large and medium-sized vessels, particularly the extracranial branches of the carotid artery. It is more com- The Maurice and Gabriela Goldschleger G School of Dental Medicine mon in women (M:F ratio 2:5) and usually affects patients older 1 Tel Aviv University, Israel than 50 years with an increased risk with age. The highest preva- lence of GCA has been reported in Scandinavian populations and Correspondence to: in those with a strong Scandinavian ethnic background.2 Dr. -

The Skull O Neurocranium, Form and Function O Dermatocranium, Form
Lesson 15 ◊ Lesson Outline: ♦ The Skull o Neurocranium, Form and Function o Dermatocranium, Form and Function o Splanchnocranium, Form and Function • Evolution and Design of Jaws • Fate of the Splanchnocranium ♦ Trends ◊ Objectives: At the end of this lesson, you should be able to: ♦ Describe the structure and function of the neurocranium ♦ Describe the structure and function of the dermatocranium ♦ Describe the origin of the splanchnocranium and discuss the various structures that have evolved from it. ♦ Describe the structure and function of the various structures that have been derived from the splanchnocranium ♦ Discuss various types of jaw suspension and the significance of the differences in each type ◊ References: ♦ Chapter: 9: 162-198 ◊ Reading for Next Lesson: ♦ Chapter: 9: 162-198 The Skull: From an anatomical perspective, the skull is composed of three parts based on the origins of the various components that make up the final product. These are the: Neurocranium (Chondocranium) Dermatocranium Splanchnocranium Each part is distinguished by its ontogenetic and phylogenetic origins although all three work together to produce the skull. The first two are considered part of the Cranial Skeleton. The latter is considered as a separate Visceral Skeleton in our textbook. Many other morphologists include the visceral skeleton as part of the cranial skeleton. This is a complex group of elements that are derived from the ancestral skeleton of the branchial arches and that ultimately gives rise to the jaws and the skeleton of the gill