Progress Toward Measles Elimination — European Region, 2009–2018
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The United Nations' Political Aversion to the European Microstates
UN-WELCOME: The United Nations’ Political Aversion to the European Microstates -- A Thesis -- Submitted to the University of Michigan, in partial fulfillment for the degree of HONORS BACHELOR OF ARTS Department Of Political Science Stephen R. Snyder MARCH 2010 “Elephants… hate the mouse worst of living creatures, and if they see one merely touch the fodder placed in their stall they refuse it with disgust.” -Pliny the Elder, Naturalis Historia, 77 AD Acknowledgments Though only one name can appear on the author’s line, there are many people whose support and help made this thesis possible and without whom, I would be nowhere. First, I must thank my family. As a child, my mother and father would try to stump me with a difficult math and geography question before tucking me into bed each night (and a few times they succeeded!). Thank you for giving birth to my fascination in all things international. Without you, none of this would have been possible. Second, I must thank a set of distinguished professors. Professor Mika LaVaque-Manty, thank you for giving me a chance to prove myself, even though I was a sophomore and studying abroad did not fit with the traditional path of thesis writers; thank you again for encouraging us all to think outside the box. My adviser, Professor Jenna Bednar, thank you for your enthusiastic interest in my thesis and having the vision to see what needed to be accentuated to pull a strong thesis out from the weeds. Professor Andrei Markovits, thank you for your commitment to your students’ work; I still believe in those words of the Moroccan scholar and will always appreciate your frank advice. -

San Marino Legal E
Study on Homophobia, Transphobia and Discrimination on Grounds of Sexual Orientation and Gender Identity Legal Report: San Marino 1 Disclaimer: This report was drafted by independent experts and is published for information purposes only. Any views or opinions expressed in the report are those of the author and do not represent or engage the Council of Europe or the Office of the Commissioner for Human Rights. 1 This report is based on Dr Maria Gabriella Francioni, The legal and social situation concerning homophobia and discrimination on the grounds of sexual orientation in the Republic of San Marino , University of the Republic of San Marino, Juridical Studies Department, 2010. The latter report is attached to this report. Table of Contents A. EXECUTIVE SUMMARY 3 B. FINDINGS 3 B.1. Overall legal framework 3 B.2. Freedom of Assembly, Association and Expression 10 B.3. Hate crime - hate speech 10 B.4. Family issues 13 B.5. Asylum and subsidiary protection 16 B.6. Education 17 B.7. Employment 18 B.8. Health 20 B.9. Housing and Access to goods and services 21 B.10. Media 22 B.11. Transgender issues 23 Annex 1: List of relevant national laws 27 Annex 2: Report of Dr Maria Gabriella Francioni, The legal and social situation concerning homophobia and discrimination on the grounds of sexual orientation in the Republic of San Marino, University of the Republic of San Marino, Juridical Studies Department, 2010 31 A. Executive Summary 1. The Statutes "Leges Statuae Reipublicae Sancti Marini" that came into force in 1600 and the Laws that reform such Statutes represented the written source for excellence of the Sammarinese legal system. -
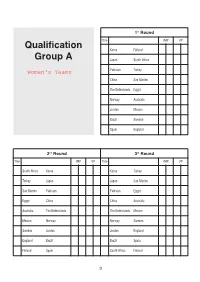
WBF Wroclaw 2016 Schedule Open
1st Round TbleIMP VP Qualification Korea Finland Group A Japan South Africa Pakistan Turkey China San Marino The Netherlands Egypt Norway Australia Jordan Mexico Brazil Sweden Spain England 2nd Round 3rd Round TbleIMP VP TbleIMP VP South Africa Korea Korea Turkey Turkey Japan Japan San Marino San Marino Pakistan Pakistan Egypt Egypt China China Australia Australia The Netherlands The Netherlands Mexico Mexico Norway Norway Sweden Sweden Jordan Jordan England England Brazil Brazil Spain Finland Spain South Africa Finland 3 4th Round 5th Round TbleIMP VP TbleIMP VP San Marino Korea Korea Egypt Egypt Japan Japan Australia Australia Pakistan Pakistan Mexico Mexico China China Sweden Sweden The Netherlands The Netherlands England England Norway Norway Spain Spain Jordan Jordan Brazil Finland Brazil San Marino South Africa South Africa Turkey Turkey Finland 6th Round 7th Round TbleIMP VP TbleIMP VP Australia Korea Korea Mexico Mexico Japan Japan Sweden Sweden Pakistan Pakistan England England China China Spain Spain The Netherlands The Netherlands Brazil Brazil Norway Norway Jordan Finland Jordan Australia South Africa South Africa Egypt Egypt Turkey Turkey San Marino San Marino Finland 4 8th Round 9th Round TbleIMP VP TbleIMP VP Sweden Korea Korea England England Japan Japan Spain Spain Pakistan Pakistan Brazil Brazil China China Jordan Jordan The Netherlands The Netherlands Norway Finland Norway Sweden South Africa South Africa Mexico Mexico Turkey Turkey Australia Australia San Marino San Marino Egypt Egypt Finland 10th Round 11th Round -

An Analysis of Five European Microstates
Geoforum, Vol. 6, pp. 187-204, 1975. Pergamon Press Ltd. Printed in Great Britain The Plight of the Lilliputians: an Analysis of Five European Microstates Honor6 M. CATUDAL, Jr., Collegeville, Minn.” Summary: The mini- or microstate is an important but little studied phenomenon in political geography. This article seeks to redress the balance and give these entities some of the attention they deserve. In general, five microstates are examined; all are located in Western Europe-Andorra, Liechtenstein, Monaco, San Marino and the Vatican. The degree to which each is autonomous in its internal affairs is thoroughly explored. And the extent to which each has control over its external relations is investigated. Disadvantages stemming from its small size strike at the heart of the ministate problem. And they have forced these nations to adopt practices which should be of use to large states. Zusammenfassung: Dem Zwergstaat hat die politische Geographie wenig Beachtung geschenkt. Urn diese Liicke zu verengen, werden hier fiinf Zwergstaaten im westlichen Europa untersucht: Andorra, Liechtenstein, Monaco, San Marino und der Vatikan. Das Ma13der inneren und lul3eren Autonomie wird griindlich untersucht. Die Kleinheit hat die Zwargstaaten zu Anpassungsformen gezwungen, die such fiir groRe Staaten van Bedeutung sein k8nnten. R&sum& Les Etats nains n’ont g&e fait I’objet d’Btudes de geographic politique. Afin de combler cette lacune, cinq mini-Etats sent examines ici; il s’agit de I’Andorre, du Liechtenstein, de Monaco, de Saint-Marin et du Vatican. Dans quelle mesure ces Etats disposent-ils de l’autonomie interne at ont-ils le contrble de leurs relations extirieures. -
ESC15 Points from Juries
Sven Zemanek (hszemi.de) underCC-BY-SA Points from Juries 10 12 4 8 6 0 2 Czech Republic Malta Australia Lithuania Montenegro Sweden Iceland Poland Cyprus Azerbaijan Portugal Slovenia Germany Ireland Israel Italy Latvia Norway San Marino Switzerland United Kingdom Sven Zemanek (hszemi.de) underCC-BY-SA Points from Juries 10 12 4 8 6 0 2 Italy Israel Australia Ireland Norway Slovenia United Kingdom Germany Latvia Cyprus Poland Iceland Lithuania Sweden Czech Republic San Marino Switzerland Azerbaijan Malta Montenegro Portugal Sven Zemanek (hszemi.de) underCC-BY-SA Points from Juries 10 12 4 8 6 0 2 Poland Israel Germany Ireland San Marino United Kingdom Portugal Sweden Czech Republic Montenegro Australia Azerbaijan Cyprus Iceland Italy Latvia Lithuania Malta Norway Slovenia Switzerland Sven Zemanek (hszemi.de) underCC-BY-SA Points from Juries 10 12 4 8 6 0 2 Azerbaijan Switzerland Ireland Poland Lithuania Portugal Australia Cyprus Czech Republic Iceland Germany Israel Italy Latvia Malta Montenegro Norway San Marino Slovenia Sweden United Kingdom Sven Zemanek (hszemi.de) underCC-BY-SA Points from Juries 10 12 4 8 6 0 2 Latvia United Kingdom Czech Republic Sweden Germany Cyprus Australia San Marino Switzerland Ireland Lithuania Slovenia Norway Azerbaijan Iceland Italy Montenegro Poland Israel Malta Portugal Sven Zemanek (hszemi.de) underCC-BY-SA Points from Juries 10 12 4 8 6 0 2 United Kingdom Poland Azerbaijan Ireland Italy Norway Portugal Cyprus Iceland Israel Malta Germany San Marino Sweden Australia Montenegro Lithuania Slovenia Switzerland -

Treaty of Lausanne: the Tool of Minority Protection for the Cham Albanians of Greece
PEOPLE: International Journal of Social Sciences ISSN 2454-5899 Gözübenli & Çavuşoğlu, 2018 Volume 4 Issue 3, pp.474-481 Date of Publication: 23rd November 2018 DOI-https://dx.doi.org/10.20319/pijss.2018.43.474481 This paper can be cited as: Gözübenli, A. S. & Çavuşoğlu, H. (2018). Treaty of Lausanne: The Tool of Minority Protection for the Cham Albanians of Greece. PEOPLE: International Journal of Social Sciences, 4(3), 474-481. This work is licensed under the Creative Commons Attribution-NonCommercial 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc/4.0/ or send a letter to Creative Commons, PO Box 1866, Mountain View, CA 94042, USA. TREATY OF LAUSANNE: THE TOOL OF MINORITY PROTECTION FOR THE CHAM ALBANIANS OF GREECE Abdullah Sencer Gözübenli, MA Mother Teresa University, Skopje, Republic of Macedonia [email protected] Halim Çavuşoğlu, Ph.D Hacettepe University, Ankara, Turkey [email protected] Abstract Cham Albanians, a predominantly Muslim sub-group of Albanians who originally reside in the coastal region of Southern Epirus in Greece’s border region with Albania, had been expelled from Greece twice.As the majority of Cham Albanians were Muslim, they were treated with the same contempt as ethnic Turks living in Greece. According to official data, 3.000 of them were transferred to Turkey as part of the Greek-Turkish population exchange according to the Convention Concerning the Exchange of Greek and Turkish Populations signed at Lausanne on 30 January 1923. Articles 37 to 44 of the Lausanne Peace Treaty attribute substantive rights for exempted Muslims in Greece and non-Muslims in Turkey from the Greek-Turkish population exchange and 17,008 of them wereexempted from the exchange. -

In San Marino REPUBLIC of SAN MARINO
Year IV July-September 2012 n. 3 INFORMATION MAGAZINE PUBLISHED BY THE CHAMBER OF COMMERCE OF THE in san marino REPUBLIC OF SAN MARINO CONTENTS Foreign Office Mission in Slovenia Foreign Club news Members’ area Statistics Postal cards issue San Marino Castels Emissione cartoline postali Castelli di San Marino (2005) Author / Autore: Irio Ottavio Fantini E DITORIAL Massimo Ghiotti - General Manager The real voyage of discovery consists not in seeking generations are making to create for themselves managing to tackle the crisis precisely because new landscapes, but in having new eyes a place in the world, for their determination to they have been exporting their goods the world Marcel Proust build something, create, innovate, sometimes re- over for more than twenty years now. inventing jobs and trades, other times emigrating The biggest gift which 2012 can make to us, is When historians speak in future about 2012 for the in search of better opportunities. We really are at to leave us at this turning point and enable us to a turning point. Republic of San Marino, they will do so with mixed firmly grip the reins of our future. And today, youngsters represent a new collective As entrepreneurs, I feel sure you will take up the emotions. Depending on individual viewpoints, voice, increasingly more a part of social and eco- 2012 is proving to be a year of stimulation for challenge and prove that radical change is possi- nomic dynamics, to the extent that Governments ble; the old ways of doing business must be re- creativity, search for opportunities and innovation, and Companies are learning, some more slowly but also one of recession, high unemployment and nounced, old models must be seen in a new per- than others, that listening to the voice of the mass- spective, more creative, might I say unexpected. -

Italy and the Republic of San Marino
Integrated Country Strategy Italy and The Republic of San Marino FOR PUBLIC RELEASE FOR PUBLIC RELEASE Table of Contents 1. Chief of Mission Priorities ................................................................................................... 2 2. Mission Strategic Framework ............................................................................................. 5 3. Mission Goals and Objectives ............................................................................................. 7 4. Management Objectives. .................................................................................................. 13 FOR PUBLIC RELEASE Approved: August 3, 2018 1 FOR PUBLIC RELEASE 1. Chief of Mission Priorities Italy has long been one of our closest allies and best trading partners, with exceptionally strong bonds between our people, including tens of millions of Americans of Italian descent, and the exchange of millions of travelers and students between our two countries every year. Italy embraces its role as a founding member of NATO and the European Union, and Italian politicians and diplomats frequently observe that Italy has had a consistent foreign policy since the beginning of the Italian Republic in 1946, despite frequent changes of government. Under NATO, Italy hosts over 30,000 U.S. military and Department of Defense civilians and their families on five bases. Italy has been the second leading troop contributor to both the Defeat-ISIS Coalition in Iraq and the Resolute Support Mission in Afghanistan, and is strongly committed to UN peacekeeping. Italy has been a steadfast partner in international forums and our single most important ally for projecting military power into the greater Mediterranean. Due to its historical relationships and geographic proximity to North Africa, Italy has been vulnerable to the influx of migrants across the Mediterranean and has been a leader on addressing instability in Libya and the root causes of the migration crisis in the Sahel. -

Smallest Country.Indd
Unit focus: Countries Around The World Text focus: Information Text (710L) STAGE 3 The Smallest Country Not all countries are as big as you might think. Some are smaller than some of the citi es of you know. They might even have fewer people living there than are in your school! Let’s have a look at the 5 smallest countries in the world. Fifth smallest - San Marino Once upon a ti me, Italy was made up of lots of small city-states. These all became part of one big country over ti me, but San Marino stood on its own. It is the world’s oldest republic (a nati on that has an elected president instead of a king or queen). San Marino is situated in the middle of Italy. This makes it almost unique. It has an area of 23.63 square miles and a populati on of roughly 33,000 people. Fourth smallest - Tuvalu Tuvalu is a country made up of 9 ti ny islands in the South Pacifi c Ocean. It is part of the Briti sh Empire. The total area of the islands is less than 10 square miles. Most of the 11,000 people live on the island of Fongafale. This island is only 20 metres across at its narrowest point! Scienti sts and locals are worried that the islands will disappear beneath the sea in the next 50 to 100 years because of global warming. Third smallest - Nauru Nauru is a ti ny island in Micronesia. It is northeast of Australia. It gained independence in 1968. -

Member States
1/10/19 Total: 193 MEMBER STATES Afghanistan Democratic Republic of the Congo Albania Denmark Algeria Djibouti Andorra Dominica Angola Dominican Republic* Antigua and Barbuda Ecuador Argentina* Egypt* Armenia El Salvador Australia* Equatorial Guinea* Austria Eritrea Azerbaijan Estonia Bahamas Eswatini Bahrain Ethiopia Bangladesh Fiji Barbados Finland* Belarus France* Belgium Gabon Belize Gambia Benin Georgia Bhutan Germany* Bolivia (Plurinational State of) Ghana Bosnia and Herzegovina Greece* Botswana Grenada Brazil* Guatemala Brunei Darussalam Guinea Bulgaria Guinea-Bissau Burkina Faso Guyana Burundi Haiti Cabo Verde Honduras Cambodia Hungary Cameroon Iceland Canada* India* Central African Republic Indonesia Chad Iran (Islamic Republic of) Chile Iraq China* Ireland Colombia* Israel Comoros Italy* Congo Jamaica Cook Islands Japan* Costa Rica* Jordan Côte d'Ivoire* Kazakhstan Croatia Kenya Cuba Kiribati Cyprus Kuwait Czechia Kyrgyzstan Democratic People's Republic of Korea Lao People's Democratic Republic *Council Member State Latvia Rwanda Lebanon Saint Kitts and Nevis Lesotho Saint Lucia Liberia Saint Vincent and the Grenadines Libya Samoa Lithuania San Marino Luxembourg Sao Tome and Principe Madagascar Saudi Arabia* Malawi Senegal Malaysia* Serbia Maldives Seychelles Mali Sierra Leone Malta Singapore* Marshall Islands Slovakia Mauritania Slovenia Mauritius Solomon Islands Mexico* Somalia Micronesia (Federated States of) South Africa* Monaco South Sudan Mongolia Spain* Montenegro Sri Lanka Morocco Sudan* Mozambique Suriname Myanmar Sweden -

Women Teams Schedule
46th European Teams Championships Women Teams Schedule Match 1 Match 2 Denmark v Bye Netherlands v Denmark Sweden v Netherlands Finland v Sweden Finland v Croatia Poland v Croatia Germany v Poland Norway v Germany Norway v Scotland Israel v Scotland Iceland v Israel San Marino v Iceland San Marino v France Turkey v France England v Turkey Faroe Islands v England Czech Republic v Faroe Islands Spain v Czech Republic Italy v Spain Ireland v Italy Ireland v Austria Hungary v Austria Russia v Hungary Bye v Russia Match 3 Match 4 Denmark v Finland Poland v Denmark Sweden v Poland Norway v Sweden Croatia v Norway Israel v Croatia Germany v Israel San Marino v Germany Scotland v San Marino Turkey v Scotland Iceland v Turkey Faroe Islands v Iceland France v Faroe Islands Spain v France England v Spain Ireland v England Czech Republic v Ireland Hungary v Czech Republic Italy v Hungary Russia v Italy Austria v Russia Bye v Austria Netherlands v Bye Netherlands v Finland Match 5 Match 6 Denmark v Norway Israel v Denmark Sweden v Israel San Marino v Sweden Croatia v San Marino Turkey v Croatia Germany v Turkey Faroe Islands v Germany Scotland v Faroe Islands Spain v Scotland Iceland v Spain Ireland v Iceland France v Ireland Hungary v France England v Hungary Russia v England Czech Republic v Russia Austria v Czech Republic Italy v Austria Bye v Italy Poland v Netherlands Netherlands v Norway Finland v Bye Finland v Poland Match 7 Match 8 Denmark v San Marino Turkey v Denmark Sweden v Turkey Faroe Islands v Sweden Croatia v Faroe Islands Spain v -

Worldwide Differences in COVID-19-Related Mortality T I G O
DOI: 10.1590/1413-81232020256.1.11112020 2403 AR Worldwide differences in COVID-19-related mortality T I G O Diferenças nas taxas de mortalidade por COVID-19 AR T ao redor do mundo IC LE Pedro Curi Hallal (https://orcid.org/0000-0003-1470-6461) 1 Abstract Mortality statistics due to COVID-19 Resumo Neste artigo, são comparadas as esta- worldwide are compared, by adjusting for the tísticas de mortalidade por COVID-19 no mun- size of the population and the stage of the pan- do, ajustando-se para o tamanho da população e demic. Data from the European Centre for Dise- para o estágio da pandemia em cada país. Foram ase Control and Prevention, and Our World in utilizados dados dos websites do Centro para o Data websites were used. Analyses are based on Controle e Prevenção de Doenças da Europa e do number of deaths per one million inhabitants. In Our World in Data. As análises são baseadas no order to account for the stage of the pandemic, the número de mortes por um milhão de habitantes. baseline date was defined as the day in which the Para levar em consideração o estágio da pandemia, 10th death was reported. The analyses included definiu-se como linha de base a data da décima 78 countries and territories which reported 10 morte em cada país. As análises incluíram 78 pa- or more deaths by April 9. On day 10, India had íses e territórios com 10 ou mais mortes relatadas 0.06 deaths per million, Belgium had 30.46 and até o dia 09 de abril.