The Use of Cadaveric Skin Allografts in the Management of Extensive Wounds
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Transplantation and Hepatic Pathology University of Pittsburgh Medical Center November, 2007
Resident Handbook Division of Transplantation and Hepatic Pathology University of Pittsburgh Medical Center November, 2007 For private use of residents only- not for public distribution Table of Contents Anatomic Transplantation Pathology Rotation Clinical Responsibilities of the Division ........................................................3 Categorizations of Specimens and Structure of Signout.................................3 Resident Responsibilities................................................................................4 Learning Resources.........................................................................................4 Transplantation Pathology on the World-Wide Web......................................4 Weekly Schedule ............................................................................................6 Staff Locations and Telephone Numbers........................................................7 Background Articles Landmarks in Transplantation ........................................................................8 Trends in Organ Donation and Transplantation US 1996-2005.....................18 Perspectives in Organ Preservation………....................................................26 Transplant Tolerance- Editorial……………………………………….…….36 Kidney Grading Systems Banff 2005 Update……………………….....................................................42 Banff 97 Components (I t v g etc.) ................................................................44 Readings Banff 05 Meeting Report………………………………………...................47 -
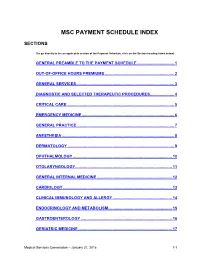
Msc Payment Schedule Index
MSC PAYMENT SCHEDULE INDEX SECTIONS (To go directly to the an applicable section of the Payment Schedule, click on the Section heading listed below) GENERAL PREAMBLE TO THE PAYMENT SCHEDULE .................................. 1 2. OUT-OF-OFFICE HOURS PREMIUMS ............................................................... 2 3. GENERAL SERVICES ......................................................................................... 3 4. DIAGNOSTIC AND SELECTED THERAPEUTIC PROCEDURES ...................... 4 5. CRITICAL CARE .................................................................................................. 5 6. EMERGENCY MEDICINE .................................................................................... 6 7. GENERAL PRACTICE ......................................................................................... 7 8. ANESTHESIA ...................................................................................................... 8 9. DERMATOLOGY ................................................................................................. 9 10. OPHTHALMOLOGY .......................................................................................... 10 11. OTOLARYNGOLOGY ........................................................................................ 11 12. GENERAL INTERNAL MEDICINE .................................................................... 12 13. CARDIOLOGY ................................................................................................... 13 14. CLINICAL IMMUNOLOGY AND ALLERGY -

Skin Grafts in Cutaneous Oncology* Enxertia De Pele Em Oncologia
RevABDV81N5.qxd 07.11.06 17:07 Page 465 465 Artigo de Revisão Enxertia de pele em oncologia cutânea* Skin grafts in cutaneous oncology* José Anselmo Lofêgo Filho1 Paula Dadalti2 Diogo Cotrim de Souza3 Paulo Roberto Cotrim de Souza4 Marcos Aurélio Leiros da Silva5 Cristina Maeda Takiya6 Resumo: Em oncologia cutânea depara-se freqüentemente com situações em que a confec- ção de um enxerto é uma boa alternativa para o fechamento do defeito cirúrgico. Conhecer aspectos referentes à integração e contração dos enxertos é fundamental para que os cirur- giões dermatológicos procedam de maneira a não contrariar princípios básicos do trans- plante de pele. Os autores fazem uma revisão da classificação e fisiologia dos enxertos de pele, acrescendo considerações cirúrgicas determinantes para o sucesso do procedimento. Palavras-chave: Neoplasias cutâneas; Transplante de pele; Transplante homólogo Abstract: In cutaneous oncology, there are many situations in which skin grafts could be a good alternative for closing surgical defect. Dermatological surgeons should have enough knowledge about graft integration and contraction in order to not contradict the basic prin- ciples of skin transplantation. The authors review skin graft classification and physiology and make some surgical considerations on successful procedures. Keywords: Skin neoplasms; Skin transplantation; Transplantation, homologous INTRODUÇÃO Enxerto é parte de um tecido vivo transplanta- tológica. São simples quando apresentam um único do de um lugar para outro no mesmo organismo ou tipo de tecido e compostos quando constituídos de em organismos distintos.1 Contudo, a utilização da dois ou mais tipos de tecidos. Em oncologia cutânea, terminologia enxerto para designar uma modalidade um enxerto composto é usado quando o defeito cirúrgica, apesar de errônea, tornou-se coloquial. -

AMRITA HOSPITALS AMRITA AMRITA HOSPITALS HOSPITALS Kochi * Faridabad (Delhi NCR) Kochi * Faridabad (Delhi NCR)
AMRITA HOSPITALS HOSPITALS AMRITA AMRITA AMRITA HOSPITALS HOSPITALS Kochi * Faridabad (Delhi NCR) Kochi * Faridabad (Delhi NCR) A Comprehensive A Comprehensive Overview Overview A Comprehensive Overview AMRITA INSTITUTE OF MEDICAL SCIENCES AIMS Ponekkara P.O. Kochi, Kerala, India 682 041 Phone: (91) 484-2801234 Fax: (91) 484-2802020 email: [email protected] website: www.amritahospitals.org Copyright@2018 AMRITA HOSPITALS Kochi * Faridabad (Delhi-NCR) A COMPREHENSIVE OVERVIEW A Comprehensive Overview Copyright © 2018 by Amrita Institute of Medical Sciences All rights reserved. No portion of this book, except for brief review, may be reproduced, stored in a retrieval system, or transmitted in any form or by any means —electronic, mechanical, photocopying, recording, or otherwise without permission of the publisher. Published by: Amrita Vishwa Vidyapeetham Amrita Institute of Medical Sciences AIMS Ponekkara P.O. Kochi, Kerala 682041 India Phone: (91) 484-2801234 Fax: (91) 484-2802020 email: [email protected] website: www.amritahospitals.org June 2018 2018 ISBN 1-879410-38-9 Amrita Institute of Medical Sciences and Research Center Kochi, Kerala INDIA AMRITA HOSPITALS KOCHI * FARIDABAD (DELHI-NCR) A COMPREHENSIVE OVERVIEW 2018 Amrita Institute of Medical Sciences and Research Center Kochi, Kerala INDIA CONTENTS Mission Statement ......................................... 04 Message From The Director ......................... 05 Our Founder and Inspiration Sri Mata Amritanandamayi Devi .................. 06 Awards and Accreditations ......................... -

Clinical Considerations in Facial Transplantation
CLINICAL CONSIDERATIONS IN FACIAL TRANSPLANTATION by Anthony Renshaw A thesis submitted in fulfilment of the requirements of University College London for the degree of Doctor of Medicine January 2011 Department of Plastic and Reconstructive Surgery, Academic Division of Surgical & Interventional Sciences, University College London 1 Declaration I, Anthony Renshaw, confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated in the thesis The copyright of this thesis rests with the author and no quotation from it or information derived from it may be published without the prior written consent of the author. …………………………………………………………. 2 Abstract Facial transplantation has emerged as the next step on the reconstructive ladder for severe facial disfigurement. Clinical issues surrounding facial tissue donation are examined, comprising pre-transplant facial vessel delineation; pre-operative aesthetic matching; and attitudes towards donation. An anatomical study of 200 consecutive facial and transverse facial vessels was performed using colour Doppler ultrasound. Facial vessels were measured at three landmarks and their branching pattern documented. The facial artery main branch was detected at the lower mandibular border in 99.5% of cases, the accompanying facial vein in 97.5%. The transverse facial artery was present in 75.5% of cases, the vein found in 58%. When the facial artery was undetectable, there was transverse facial artery dominance. When the facial vein was absent it was replaced with a transverse facial vein. This provides valuable pre-operative information regarding vessel status. A quantitative eleven- point skin tonal matching scheme is described using digital analysis of facial imagery. -

78581/2020/Estt-Ne Hr
105 78581/2020/ESTT-NE_HR 1| T a r i f f - AIMS 106 78581/2020/ESTT-NE_HR INDEX 1. General Information ( Section A) 3 i. Out Patient Department ii. Ambulance Charges 2. General Information ( Section B) 5 i. Bed charges ii. In patient Consultation fees iii. Billing Of Surgery Anesthesia and OT Charges iv. Billing Of Surgery /Procedure/ others 3. LAB 9 4. Outsouce Lab 16 5. Blood Bank 64 6. Imaging & Radiodiagnosis 65 7. Non – Invasive Lab 80 8. Anesthesia 82 9. Cardiology and Cardiac Surgery 84 10. Critical Care Services 89 11. Baby Care 91 12. Common Procedure 94 13 Dental 94 14 Dermatology 101 15 E N T 105 16 Gastroenterology 110 17 Maxillo Facial Surgery 113 18 Nephrology 116 19 Neuro Diagnostic Lab 118 20 Oncology 112 21 Ophthalmology 136 22 Orthopedies 142 23 OBS & Gynaecology 149 24 Physiotherapy 154 25 Respiratory Medicine 156 26 Surgery & Major Procedures i. General Surgery 158 ii. Pediatric Surgery 165 iii. PlasticSurgery 170 iv. Neuro Surgery 182 27 Urology 185 28 Interventional Radiology 192 29 Interventional Pain Management 194 30 Paediatric Cardiac Surgery 197 31 Bed Side Service Charges200 2| T a r i f f - AIMS 107 78581/2020/ESTT-NE_HRSection – A GENERAL INFORMATION OUT PATIENT DEPARTMENT OPD Consultations: Superspeciality OPD Consultation * Rs. 700 Specialty OPD Consultation** Rs. 400 to 800 Note: OPD Timing Monday- Saturday ( 8:00AM – 7:00PM) *Super specialty Departments – Cardiac Surgery, Cardiology, Neurology, Neurosurgery, Oncology, Respiratory Medicine, Urology, Plastic Surgery, Gastroenterology, Endocrinology, Paediatric -

Skin Grafting in the Dog Elroy C
Volume 19 | Issue 3 Article 1 1957 Skin Grafting in the Dog Elroy C. Jensen Iowa State College Follow this and additional works at: https://lib.dr.iastate.edu/iowastate_veterinarian Part of the Small or Companion Animal Medicine Commons, and the Veterinary Anatomy Commons Recommended Citation Jensen, Elroy C. (1957) "Skin Grafting in the Dog," Iowa State University Veterinarian: Vol. 19 : Iss. 3 , Article 1. Available at: https://lib.dr.iastate.edu/iowastate_veterinarian/vol19/iss3/1 This Article is brought to you for free and open access by the Journals at Iowa State University Digital Repository. It has been accepted for inclusion in Iowa State University Veterinarian by an authorized editor of Iowa State University Digital Repository. For more information, please contact [email protected]. SKIN GRAFTING In The Dog Elroy C. J,ensen, D.V.M. THERE are several histological factors the arm instead of from the forehead. which have made skin grafting pos This technique is now known as the Ital sible in man and animals. First, the com ian method of rhinoplasty. Free skin parative ease which epithelium can regen grafting started early in the 19th century erate is a factor. This new growth of tis by two charlatans which is related by sue occurs either from the periphery of a Baroni, the physi'Ologist, "A woman wound or it may result from proliferation named Gamba Curat, in order to show of the external root sheath of the hair the efficiency of an ointment she was sel follicles providing the dermis has not been ling, cut a piece of skin from her thigh completely destroyed. -

Role of Ia-Like Products of the Main Histocompatibility Complex in Conditioning Skin Allograft Survival in Man
Role of Ia-Like Products of the Main Histocompatibility Complex in Conditioning Skin Allograft Survival in Man J. Dausset, … , T. Meo, F. T. Rapaport J Clin Invest. 1979;63(5):893-901. https://doi.org/10.1172/JCI109389. Research Article This report correlates the survival time of 93 intrafamilial skin allografts performed under conditions of main histocompatibility complex (HLA) haploidentity with donor-recipient compatibility for products of the HLA-A, -B, -C, and - DR, as well as C3 proactivator, Glyoxalase I, and P loci located on the human 6th chromosome. Incompatibilities for HLA- A and -B (and to a lesser extent for HLA-C) and(or) for HLA-DR products exerted a strong influence upon the fate of skin allografts. When HLA-A and -B were considered alone, the most compatible group of grafts had a mean survival time of 15.8 d, as compared with 11.3 d for the most incompatible transplants. HLA-DR compatibility alone was associated with a mean survival time of 15.3 d, whereas HLA-DR-incompatible grafts had a mean survival time of 11.5 d. Incompatibilities for C3 proactivator, Glyoxalase I, and P did not have a significant effect upon graft survival. There was no evidence of an association between donor-recipient incompatibility at HLA-A, -B, or -C or at HLA-DR; such incompatibilities occurred independently of each other, in spite of the state of linkage disequilibrium known to exist between HLA-B and -DR. Incompatibilities for HLA-A, -B, and for HLA-DR exerted a potent additive effect upon graft survival. -

Historic Landmarks in Clinical Transplantation: Conclusions from the Consensus Conference at the University of California, Los Angeles
World J. Surg.24, 834-843, 2000 DOl: 10.1007/5002680010134 WORLD Journal of SURGERY © .lOOO by rhe Societe Internationale J(" Ch!wrgie Historic Landmarks in Clinical Transplantation: Conclusions from the Consensus Conference at the University of California, Los Angeles Carl G. Groth, M.D., Ph.D.,l Leslie B. Brent, B.Sc., Ph.D} Roy Y. Caine, M.D} Jean B. Dausset, M.D., Ph.D.,4 Robert A. Good, M.D., Ph.D.,s Joseph E. Murray, M.D.,6 Norman E. Shumway, M.D., Ph.D} Robert S. Schwartz, M.D} Thomas E. Starzl, M.D., Ph.D} Paul I. Terasaki, Ph.D.,l° E. Donnall Thomas, M.D}l Jon J. van Rood, M.D., Ph.DY 1Department of Transplantation Surgery, Karolinska Institute, Huddinge Hospital, SE-141 86 Huddinge, Sweden 230 Hugo Road, Tufnell Park, London N19 5EU, UK 'Department of Surgery, University of Cambridge, Douglas House Annexe, 18 Trumpington Road, Cambridge CB2 ZAH, UK "Foundation Jean Dausset-C.E.P.H., 27 rue Juliette Dodu, 75010 Paris Cedex, France 5Department of Pediatrics, Division of Allergy and Immunology, All Children's Hospital, 801 Sixth Street South, SI. Petersburg, Florida 33701, USA "Department of Surgery, Brigham and Women's Hospital, 75 Francis Street, Boston, Massachusetts 02115, USA 'Department of Cardiothoracic Surgery, Falk Cardiovascular Research Center, Stanford University School of Medicine, 300 Pasteur Drive, Stanford, California 94305-5247, USA 'The New England Journal of Medicine, 10 Shattuck Street, Boston, Massachusetts 02115-6094, USA 9Department of Surgery, University of Pittsburgh, School of Medicine, Thomas E. Starzl Transplantation Institute, 3601 Fifth Avenue, Pittsburgh, Pennsylvania 15213, USA 1012835 Parkyns Street, Los Angeles, California 90049, USA lIDepartment of Medicine, Fred Hutchinson Cancer Research Center, 1100 Fairview Avenue N, PO Box 19024, Seattle, Washington 98109-1024, USA 12Department of Immunohematology and Blood Bank, University Medical Center, PO Box 9600, 2300 RC Leiden, The Netherlands Abstract. -

SKIN GRAFTS and SKIN SUBSTITUTES James F Thornton MD
SKIN GRAFTS AND SKIN SUBSTITUTES James F Thornton MD HISTORY OF SKIN GRAFTS ANATOMY Ratner1 and Hauben and colleagues2 give excel- The character of the skin varies greatly among lent overviews of the history of skin grafting. The individuals, and within each person it varies with following highlights are excerpted from these two age, sun exposure, and area of the body. For the sources. first decade of life the skin is quite thin, but from Grafting of skin originated among the tilemaker age 10 to 35 it thickens progressively. At some caste in India approximately 3000 years ago.1 A point during the fourth decade the thickening stops common practice then was to punish a thief or and the skin once again begins to decrease in sub- adulterer by amputating the nose, and surgeons of stance. From that time until the person dies there is their day took free grafts from the gluteal area to gradual thinning of dermis, decreased skin elastic- repair the deformity. From this modest beginning, ity, and progressive loss of sebaceous gland con- skin grafting evolved into one of the basic clinical tent. tools in plastic surgery. The skin also varies greatly with body area. Skin In 1804 an Italian surgeon named Boronio suc- from the eyelid, postauricular and supraclavicular cessfully autografted a full-thickness skin graft on a areas, medial thigh, and upper extremity is thin, sheep. Sir Astley Cooper grafted a full-thickness whereas skin from the back, buttocks, palms of the piece of skin from a man’s amputated thumb onto hands and soles of the feet is much thicker. -

Quantitative Analysis of the Kidney Allocation Policy in USA A
Quantitative Analysis of the Kidney Allocation Policy in USA A dissertation presented to the faculty of the Russ College of Engineering and Technology of Ohio University In partial fulfilment of the requirements for the degree Doctor of Philosophy Philip Appiah – Kubi May 2015 © 2015 Philip Appiah – Kubi. All Rights Reserved. 2 This dissertation titled Quantitative Analysis of the Kidney Allocation Policy in USA by PHILIP APPIAH – KUBI has been approved for the Department of Mechanical and Systems Engineering the Russ College of Engineering and Technology by Namkyu Park Associate Professor of Industrial and Systems Engineering Dennis Irwin Dean, Russ College of Engineering and Technology 3 ABSTRACT APPIAH-KUBI, PHILIP, Ph.D., May 2015, Mechanical and Systems Engineering Quantitative Analysis of the Kidney Allocation Policy in USA Director of Dissertation: Namkyu Park Kidney transplantation has become the preferred treatment option for people suffering from end stage renal disease (ESRD) since the successful kidney transplantation conducted by Dr. Joseph E. Murray in 1954. However, most ESRD patients are unable to undergo kidney transplantation due to the scarcity of cadaveric and living donor kidneys. People suffering from ESRD are enlisted on a kidney waiting list and prioritized based on a point scoring system. This scoring system attempts to balance equity and efficiency. For this reason the first kidney allocation policy in the United States was based on waiting time. However, this led to underutilization of kidneys. The Organ Procurement and Transplantation Network (OPTN) which is the body in charge of organ procurement and allocation has come out with a new kidney allocation policy which came into effect on December 4, 2014. -

Biju Krushak Kalyan Yojana Detailed Guidelines Government of Odisha
Biju Krushak Kalyan Yojana Detailed Guidelines Government of Odisha Directorate of Agriculture and Food Production, Department of Agriculture ___________ (as on 1 December 2013) 1 nd (2 Edition) 2 GOVERNMENT OF ODISHA BIJU KRUSHAK KALYAN YOJANA A number of studies have revealed that risk owing to low level of health security is endemic for Farmers and their family members, especially those in unorganized sector. The vulnerability of these Farmers and their family members increases when they have to pay out of pocket for their medical care with no subsidy or support. On the one hand, such a farm family does not have the financial resources to bear the cost of medical treatment; on the other, the public owned health infrastructure is unable to cope up with the demand. Large number of persons borrows money or sells assets to pay for treatment in hospitals. Thus, Health Insurance can be a way of overcoming financial handicaps, improving access to quality medical care and providing financial protection against high medical expenses. The “Biju Krushak Kalyan Yojana” announced by the Government of Odisha attempts to address such issues. For effective operation of the scheme, partnership is envisaged between the Insurance Company, public and the private sector hospitals and the State agencies. State Government/Nodal Agency will assist the Insurance Company in networking with the Government/Private hospitals, fixing of treatment protocol and costs, treatment authorization, so that the cost of administering the scheme is kept at the lowest, while making full use of the resources available in the Government/Private health systems. Public hospitals, including ESI hospitals and such private hospitals fulfilling minimum qualifications in terms of availability of inpatient medical beds, laboratory, equipments, operation theatres, smart card reader etc.