Jon Van Rood the Pioneer and His Personal View on the Early
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Immunosuppressive Effects in Infection
I Volume 63 January 1970 I1I J- 6 JAN'7O Section of Clinical ~~~~~~~~~ Immunology & Allergy President Professor Sir Michael Woodruff FRCS FRS Meeting April 14 1969 Immunosuppressive Effects in Infection Dr M H Salaman Measles: In 1908 von Pirquet noticed that the (Department ofPathology, Royal College tuberculin reaction in tuberculous children be- ofSurgeons oJ England, came negative during an attack of measles, and London) that afterwards tuberculosis often advanced rapidly. Later work has confirmed his observa- Immunodepression by tions on tuberculin sensitivity by more sensitive Mammalian Viruses and Plasmodia methods (Mellman & Wetton 1963, Brody & McAlister 1964, Starr & Berkovitch 1964), and it Depression of immune responses by viruses is has been shown (Smithwick & Berkovitch 1966) receiving increasing though much belated atten- that measles virus, added to lymphocytes of tion. Early reports (von Pirquet 1908, Bloomfield tuberculin-positive patients, prevents the mito- & Mateer 1919) were forgotten and the subject genic response to tuberculin PPD, but not the neglected till 1960 when Old and his colleagues response to phytohmmagglutinin (PHA). noticed that the hmemolysin response to sheep erythrocytes (SE) was depressed in mice infected Rubella: In infants with congenital rubella there with Friend's leukeemogenic virus (FV), and is no gross defect of antibody formation, but their Gledhill (1961) found that FV and Moloney virus lymphocytes do not respond to PHA (Alford both enhanced the pathogenicity of mouse 1965, Bellanti et al. 1965, Soothill et al. 1966). hepatitis virus. Since then reports of immuno- Normal lymphocytes treated with rubella virus in depression by a wide variety of viruses, both vitro lose their PHA-responsiveness. -

Transplantation and Hepatic Pathology University of Pittsburgh Medical Center November, 2007
Resident Handbook Division of Transplantation and Hepatic Pathology University of Pittsburgh Medical Center November, 2007 For private use of residents only- not for public distribution Table of Contents Anatomic Transplantation Pathology Rotation Clinical Responsibilities of the Division ........................................................3 Categorizations of Specimens and Structure of Signout.................................3 Resident Responsibilities................................................................................4 Learning Resources.........................................................................................4 Transplantation Pathology on the World-Wide Web......................................4 Weekly Schedule ............................................................................................6 Staff Locations and Telephone Numbers........................................................7 Background Articles Landmarks in Transplantation ........................................................................8 Trends in Organ Donation and Transplantation US 1996-2005.....................18 Perspectives in Organ Preservation………....................................................26 Transplant Tolerance- Editorial……………………………………….…….36 Kidney Grading Systems Banff 2005 Update……………………….....................................................42 Banff 97 Components (I t v g etc.) ................................................................44 Readings Banff 05 Meeting Report………………………………………...................47 -
The History of the First Kidney Transplantation
165+3 14 mm "Service to society is the rent we pay for living on this planet" The History of the Joseph E. Murray, 1990 Nobel-laureate who performed the first long-term functioning kidney transplantation in the world First Kidney "The pioneers sacrificed their scientific life to convince the medical society that this will become sooner or later a successful procedure… – …it is a feeling – now I am Transplantation going to overdo - like taking part in creation...” András Németh, who performed the first – a European Overview Hungarian renal transplantation in 1962 E d i t e d b y : "Professor Langer contributes an outstanding “service” to the field by a detailed Robert Langer recording of the history of kidney transplantation as developed throughout Europe. The authoritative information is assembled country by country by a generation of transplant professionals who knew the work of their pioneer predecessors. The accounting as compiled by Professor Langer becomes an essential and exceptional reference document that conveys the “service to society” that kidney transplantation has provided for all mankind and that Dr. Murray urged be done.” Francis L. Delmonico, M.D. Professor of Surgery, Harvard Medical School, Massachusetts General Hospital Past President The Transplantation Society and the Organ Procurement Transplant Network (UNOS) Chair, WHO Task Force Organ and Tissue Donation and Transplantation The History of the First Kidney Transplantation – a European Overview European a – Transplantation Kidney First the of History The ISBN 978-963-331-476-0 Robert Langer 9 789633 314760 The History of the First Kidney Transplantation – a European Overview Edited by: Robert Langer SemmelweisPublishers www.semmelweiskiado.hu Budapest, 2019 © Semmelweis Press and Multimedia Studio Budapest, 2019 eISBN 978-963-331-473-9 All rights reserved. -
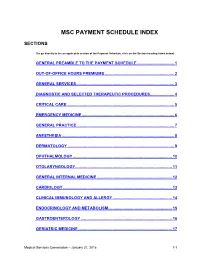
Msc Payment Schedule Index
MSC PAYMENT SCHEDULE INDEX SECTIONS (To go directly to the an applicable section of the Payment Schedule, click on the Section heading listed below) GENERAL PREAMBLE TO THE PAYMENT SCHEDULE .................................. 1 2. OUT-OF-OFFICE HOURS PREMIUMS ............................................................... 2 3. GENERAL SERVICES ......................................................................................... 3 4. DIAGNOSTIC AND SELECTED THERAPEUTIC PROCEDURES ...................... 4 5. CRITICAL CARE .................................................................................................. 5 6. EMERGENCY MEDICINE .................................................................................... 6 7. GENERAL PRACTICE ......................................................................................... 7 8. ANESTHESIA ...................................................................................................... 8 9. DERMATOLOGY ................................................................................................. 9 10. OPHTHALMOLOGY .......................................................................................... 10 11. OTOLARYNGOLOGY ........................................................................................ 11 12. GENERAL INTERNAL MEDICINE .................................................................... 12 13. CARDIOLOGY ................................................................................................... 13 14. CLINICAL IMMUNOLOGY AND ALLERGY -

Skin Grafts in Cutaneous Oncology* Enxertia De Pele Em Oncologia
RevABDV81N5.qxd 07.11.06 17:07 Page 465 465 Artigo de Revisão Enxertia de pele em oncologia cutânea* Skin grafts in cutaneous oncology* José Anselmo Lofêgo Filho1 Paula Dadalti2 Diogo Cotrim de Souza3 Paulo Roberto Cotrim de Souza4 Marcos Aurélio Leiros da Silva5 Cristina Maeda Takiya6 Resumo: Em oncologia cutânea depara-se freqüentemente com situações em que a confec- ção de um enxerto é uma boa alternativa para o fechamento do defeito cirúrgico. Conhecer aspectos referentes à integração e contração dos enxertos é fundamental para que os cirur- giões dermatológicos procedam de maneira a não contrariar princípios básicos do trans- plante de pele. Os autores fazem uma revisão da classificação e fisiologia dos enxertos de pele, acrescendo considerações cirúrgicas determinantes para o sucesso do procedimento. Palavras-chave: Neoplasias cutâneas; Transplante de pele; Transplante homólogo Abstract: In cutaneous oncology, there are many situations in which skin grafts could be a good alternative for closing surgical defect. Dermatological surgeons should have enough knowledge about graft integration and contraction in order to not contradict the basic prin- ciples of skin transplantation. The authors review skin graft classification and physiology and make some surgical considerations on successful procedures. Keywords: Skin neoplasms; Skin transplantation; Transplantation, homologous INTRODUÇÃO Enxerto é parte de um tecido vivo transplanta- tológica. São simples quando apresentam um único do de um lugar para outro no mesmo organismo ou tipo de tecido e compostos quando constituídos de em organismos distintos.1 Contudo, a utilização da dois ou mais tipos de tecidos. Em oncologia cutânea, terminologia enxerto para designar uma modalidade um enxerto composto é usado quando o defeito cirúrgica, apesar de errônea, tornou-se coloquial. -

Drug Shortages Prompt Doctors, Societies to Consider Non-Profit
Vol. 37 No. 33 Sept. 9, 2011 SPECIAL ISSUE © Copyright 2011 The Cancer Letter Inc. All rights reserved. Price $395 Per Year. To subscribe, call 800-513-7042 or visit www.cancerletter.com. PO Box 9905 Washington DC 20016 Telephone 202-362-1809 Drug Shortages Prompt Doctors, Societies To Consider Non-Profit Pharma Company By Paul Goldberg The market hasn’t been working very well in producing enough generic drugs lately. The government hasn’t done much to correct the problem, either. FDA Approvals: This year alone, as many as 180 different generic drugs have been Agency Approves affected by shortages. In oncology, drugs in short supply include cytarabine, daunorubicin, Two New Pairs of doxorubicin, leucovorin, 5-FU, cisplatin and paclitaxel. Drugs and To solve the problem, several players in oncology are considering Diagnostic Tests novel ways to produce generic drugs, as well as drugs that have no chance . Page 8 to become blockbusters, or for that matter, even modest sellers. One group of prominent oncologists is circulating a proposal—and trying Obituaries: (Continued to page 2) Fritz Bach, 77 The Duke Scandal: William Wolff, 94 Duke Researchers Retract Paper From Blood; . Page 9 Dozens of Retractions of Potti's Work Expected By Conor Hale In Brief: The journal Blood published a retraction by a group of scientists Gilbertson Named including former Duke University researcher Anil Potti—continuing a cascade Director of St. Jude; of retractions of the group’s work over the past several months. Lowe To Be Chief of Additional retractions of papers published by Potti during his time at MSKCC Geoffrey Duke are in the works, university officials said. -

AMRITA HOSPITALS AMRITA AMRITA HOSPITALS HOSPITALS Kochi * Faridabad (Delhi NCR) Kochi * Faridabad (Delhi NCR)
AMRITA HOSPITALS HOSPITALS AMRITA AMRITA AMRITA HOSPITALS HOSPITALS Kochi * Faridabad (Delhi NCR) Kochi * Faridabad (Delhi NCR) A Comprehensive A Comprehensive Overview Overview A Comprehensive Overview AMRITA INSTITUTE OF MEDICAL SCIENCES AIMS Ponekkara P.O. Kochi, Kerala, India 682 041 Phone: (91) 484-2801234 Fax: (91) 484-2802020 email: [email protected] website: www.amritahospitals.org Copyright@2018 AMRITA HOSPITALS Kochi * Faridabad (Delhi-NCR) A COMPREHENSIVE OVERVIEW A Comprehensive Overview Copyright © 2018 by Amrita Institute of Medical Sciences All rights reserved. No portion of this book, except for brief review, may be reproduced, stored in a retrieval system, or transmitted in any form or by any means —electronic, mechanical, photocopying, recording, or otherwise without permission of the publisher. Published by: Amrita Vishwa Vidyapeetham Amrita Institute of Medical Sciences AIMS Ponekkara P.O. Kochi, Kerala 682041 India Phone: (91) 484-2801234 Fax: (91) 484-2802020 email: [email protected] website: www.amritahospitals.org June 2018 2018 ISBN 1-879410-38-9 Amrita Institute of Medical Sciences and Research Center Kochi, Kerala INDIA AMRITA HOSPITALS KOCHI * FARIDABAD (DELHI-NCR) A COMPREHENSIVE OVERVIEW 2018 Amrita Institute of Medical Sciences and Research Center Kochi, Kerala INDIA CONTENTS Mission Statement ......................................... 04 Message From The Director ......................... 05 Our Founder and Inspiration Sri Mata Amritanandamayi Devi .................. 06 Awards and Accreditations ......................... -

Clinical Considerations in Facial Transplantation
CLINICAL CONSIDERATIONS IN FACIAL TRANSPLANTATION by Anthony Renshaw A thesis submitted in fulfilment of the requirements of University College London for the degree of Doctor of Medicine January 2011 Department of Plastic and Reconstructive Surgery, Academic Division of Surgical & Interventional Sciences, University College London 1 Declaration I, Anthony Renshaw, confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated in the thesis The copyright of this thesis rests with the author and no quotation from it or information derived from it may be published without the prior written consent of the author. …………………………………………………………. 2 Abstract Facial transplantation has emerged as the next step on the reconstructive ladder for severe facial disfigurement. Clinical issues surrounding facial tissue donation are examined, comprising pre-transplant facial vessel delineation; pre-operative aesthetic matching; and attitudes towards donation. An anatomical study of 200 consecutive facial and transverse facial vessels was performed using colour Doppler ultrasound. Facial vessels were measured at three landmarks and their branching pattern documented. The facial artery main branch was detected at the lower mandibular border in 99.5% of cases, the accompanying facial vein in 97.5%. The transverse facial artery was present in 75.5% of cases, the vein found in 58%. When the facial artery was undetectable, there was transverse facial artery dominance. When the facial vein was absent it was replaced with a transverse facial vein. This provides valuable pre-operative information regarding vessel status. A quantitative eleven- point skin tonal matching scheme is described using digital analysis of facial imagery. -

78581/2020/Estt-Ne Hr
105 78581/2020/ESTT-NE_HR 1| T a r i f f - AIMS 106 78581/2020/ESTT-NE_HR INDEX 1. General Information ( Section A) 3 i. Out Patient Department ii. Ambulance Charges 2. General Information ( Section B) 5 i. Bed charges ii. In patient Consultation fees iii. Billing Of Surgery Anesthesia and OT Charges iv. Billing Of Surgery /Procedure/ others 3. LAB 9 4. Outsouce Lab 16 5. Blood Bank 64 6. Imaging & Radiodiagnosis 65 7. Non – Invasive Lab 80 8. Anesthesia 82 9. Cardiology and Cardiac Surgery 84 10. Critical Care Services 89 11. Baby Care 91 12. Common Procedure 94 13 Dental 94 14 Dermatology 101 15 E N T 105 16 Gastroenterology 110 17 Maxillo Facial Surgery 113 18 Nephrology 116 19 Neuro Diagnostic Lab 118 20 Oncology 112 21 Ophthalmology 136 22 Orthopedies 142 23 OBS & Gynaecology 149 24 Physiotherapy 154 25 Respiratory Medicine 156 26 Surgery & Major Procedures i. General Surgery 158 ii. Pediatric Surgery 165 iii. PlasticSurgery 170 iv. Neuro Surgery 182 27 Urology 185 28 Interventional Radiology 192 29 Interventional Pain Management 194 30 Paediatric Cardiac Surgery 197 31 Bed Side Service Charges200 2| T a r i f f - AIMS 107 78581/2020/ESTT-NE_HRSection – A GENERAL INFORMATION OUT PATIENT DEPARTMENT OPD Consultations: Superspeciality OPD Consultation * Rs. 700 Specialty OPD Consultation** Rs. 400 to 800 Note: OPD Timing Monday- Saturday ( 8:00AM – 7:00PM) *Super specialty Departments – Cardiac Surgery, Cardiology, Neurology, Neurosurgery, Oncology, Respiratory Medicine, Urology, Plastic Surgery, Gastroenterology, Endocrinology, Paediatric -

160528 Dr. Edgar Franke
Prof. Dr. J. Floege • Rheinisch-Westfälische Technische Hochschule Aachen Universitätsklinikum • Medizinische Klinik II • Pauwelsstr. 30 • 52074 Aachen Geschäftsstelle Seumestr. 8 10245 Berlin Dr. Edgar Franke Ausschuss für Gesundheit Telefon: 030 52137269 Deutscher Bundestag Telefax: 030 52137270 Platz der Republik 1 E-Mail: [email protected] 11011 Berlin www.dgfn.eu Berlin, 29.5.2016 Vorstand: Prof. Dr. J. Floege (Präsident) Rheinisch-Westfälische Sehr geehrter Herr Dr. Franke, Technische Hochschule Aachen Universitätsklinikum Medizinische Klinik II, die Dt. Gesellschaft für Nephrologie bedankt sich für die Gelegenheit Nephrologie und Klinische einer Stellungnahme zum geplanten Transplantationsregister. Immunologie Pauwelsstr. 30 Wir begrüßen die Initiative eines bundesweiten Transplantationsregisters 52074 Aachen ausdrücklich, möchten aber unter Bezugnahme auf das mit Frau Prof. Dr. Elke Telefon: 0241 8089530 Schäffner am 15.4.16 geführte Obleutegespräch an dieser Stelle erneut auf Telefax: 0241 8082446 E-Mail: [email protected] einen Umstand hinweisen, der unserer Ansicht nach in dem bisherigen Gesetzesentwurf zu kurz greift, die Verknüpfung eines Prof. Dr. K. Amann Transplantationsregisters mit einem Dialyseregister. Prof. Dr. M. D. Alscher Prof. Dr. A. Kribben Aus folgenden Gründen halten wir eine solche Datenverknüpfung für Dr. T. Weinreich unerlässlich: Kuratorium: • Die Nephrologie ist in der Transplantationslandschaft einzigartig, da es Prof. Dr. A. Kribben flächendeckend und jahre/jahrzehntelang Nierenersatzverfahren gibt, die (Vorsitzender) -

Transplant Chronicles
Transplant Chronicles Volume 6 A publication for transplant recipients of all organs and their families, Number 1 published by the National Kidney Foundation, Inc. ow could I look down into believed we had a chance, and I hisH crib one more time knowing their responses were “like finding God would take him from me? a needle in a haystack,” or like This is my first grandchild who I “winning the lottery.” Not only are Hurt wanted so very much. blood type and cross match very important, the size of the donor My Cody was born with a heart plays a big part, too. His hypoplastic left heart, meaning he little chest would only accommo- So Bad only had two chambers instead of date a heart maybe four months the normal four. He was born at older than Cody, and his time was by Joyce Rasmussen Unity Hospital, transferred to running out. Children's Hospital, then a week later transferred to the University Cody already had lived longer of Minnesota, where for five weeks than the doctors thought, but we hoped and prayed for a heart soon it would be too late. I was transplant. Soon I was filled with trying to keep my kids’ emotions doubts and anger, which aroused down so that when the time came many questions. How could this for us to say goodbye to our dear beautiful child be created with little Cody, we could thank God only half a heart? His heart for the short time we had with monitor told me he heard and him and accept his decision. -

American Osler Society
49th Annual Meeting of the American Osler Society Sir William Osler, quoting Leigh Hunt, “Abou Ben Adhem” Sunday, May 12th – Wednesday May 15th, 2019 Hotel Omni Mont-Royal Montréal, Canada Hotel Omni Mont-Royal 49th Annual Meeting of the AMERICAN OSLER SOCIETY Sunday, May 12th – Wednesday, May 15th, 2019 Hotel Omni Mont-Royal Montréal, Canada Credit: Karen Koshof The Osler Niche contains the ashes of Sir William Osler and Lady Osler, as well as those of Osler’s dear cousin and first Librarian of the Osler Library, W.W. Francis. The Niche was designed with Osler’s wishes in mind. Its realization was not far off the vision imagined by Osler’s alter ego Egerton Yorrick Davis in “Burrowings of a Bookworm”: I like to think of my few books in an alcove of a fire-proof library in some institution that I love; at the end of the alcove an open fire-place and a few easy chairs, and on the mantelpiece an urn with my ashes and my bust or portrait through which my astral self, like the Bishop at St. Praxed’s, could peek at the books I have loved, and enjoy the delight with which kindred souls still in the flesh would handle them. Course Objectives Upon conclusion of this program, participants should be able to: Describe new research findings in the history of medicine. Outline the evolution of medicine in a particular disease. List professional contributions made by others in medicine. Intended Audience The target audience includes physicians and others interested in Osler, medical history and any of the medically oriented humanities who research and write on a range of issues.