Clinical Considerations in Facial Transplantation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Transplantation and Hepatic Pathology University of Pittsburgh Medical Center November, 2007
Resident Handbook Division of Transplantation and Hepatic Pathology University of Pittsburgh Medical Center November, 2007 For private use of residents only- not for public distribution Table of Contents Anatomic Transplantation Pathology Rotation Clinical Responsibilities of the Division ........................................................3 Categorizations of Specimens and Structure of Signout.................................3 Resident Responsibilities................................................................................4 Learning Resources.........................................................................................4 Transplantation Pathology on the World-Wide Web......................................4 Weekly Schedule ............................................................................................6 Staff Locations and Telephone Numbers........................................................7 Background Articles Landmarks in Transplantation ........................................................................8 Trends in Organ Donation and Transplantation US 1996-2005.....................18 Perspectives in Organ Preservation………....................................................26 Transplant Tolerance- Editorial……………………………………….…….36 Kidney Grading Systems Banff 2005 Update……………………….....................................................42 Banff 97 Components (I t v g etc.) ................................................................44 Readings Banff 05 Meeting Report………………………………………...................47 -
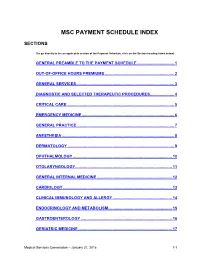
Msc Payment Schedule Index
MSC PAYMENT SCHEDULE INDEX SECTIONS (To go directly to the an applicable section of the Payment Schedule, click on the Section heading listed below) GENERAL PREAMBLE TO THE PAYMENT SCHEDULE .................................. 1 2. OUT-OF-OFFICE HOURS PREMIUMS ............................................................... 2 3. GENERAL SERVICES ......................................................................................... 3 4. DIAGNOSTIC AND SELECTED THERAPEUTIC PROCEDURES ...................... 4 5. CRITICAL CARE .................................................................................................. 5 6. EMERGENCY MEDICINE .................................................................................... 6 7. GENERAL PRACTICE ......................................................................................... 7 8. ANESTHESIA ...................................................................................................... 8 9. DERMATOLOGY ................................................................................................. 9 10. OPHTHALMOLOGY .......................................................................................... 10 11. OTOLARYNGOLOGY ........................................................................................ 11 12. GENERAL INTERNAL MEDICINE .................................................................... 12 13. CARDIOLOGY ................................................................................................... 13 14. CLINICAL IMMUNOLOGY AND ALLERGY -

Skin Grafts in Cutaneous Oncology* Enxertia De Pele Em Oncologia
RevABDV81N5.qxd 07.11.06 17:07 Page 465 465 Artigo de Revisão Enxertia de pele em oncologia cutânea* Skin grafts in cutaneous oncology* José Anselmo Lofêgo Filho1 Paula Dadalti2 Diogo Cotrim de Souza3 Paulo Roberto Cotrim de Souza4 Marcos Aurélio Leiros da Silva5 Cristina Maeda Takiya6 Resumo: Em oncologia cutânea depara-se freqüentemente com situações em que a confec- ção de um enxerto é uma boa alternativa para o fechamento do defeito cirúrgico. Conhecer aspectos referentes à integração e contração dos enxertos é fundamental para que os cirur- giões dermatológicos procedam de maneira a não contrariar princípios básicos do trans- plante de pele. Os autores fazem uma revisão da classificação e fisiologia dos enxertos de pele, acrescendo considerações cirúrgicas determinantes para o sucesso do procedimento. Palavras-chave: Neoplasias cutâneas; Transplante de pele; Transplante homólogo Abstract: In cutaneous oncology, there are many situations in which skin grafts could be a good alternative for closing surgical defect. Dermatological surgeons should have enough knowledge about graft integration and contraction in order to not contradict the basic prin- ciples of skin transplantation. The authors review skin graft classification and physiology and make some surgical considerations on successful procedures. Keywords: Skin neoplasms; Skin transplantation; Transplantation, homologous INTRODUÇÃO Enxerto é parte de um tecido vivo transplanta- tológica. São simples quando apresentam um único do de um lugar para outro no mesmo organismo ou tipo de tecido e compostos quando constituídos de em organismos distintos.1 Contudo, a utilização da dois ou mais tipos de tecidos. Em oncologia cutânea, terminologia enxerto para designar uma modalidade um enxerto composto é usado quando o defeito cirúrgica, apesar de errônea, tornou-se coloquial. -

3Rd Quarter 2001 Bulletin
In This Issue... Promoting Colorectal Cancer Screening Important Information and Documentaion on Promoting the Prevention of Colorectal Cancer ....................................................................................................... 9 Intestinal and Multi-Visceral Transplantation Coverage Guidelines and Requirements for Approval of Transplantation Facilities12 Expanded Coverage of Positron Emission Tomography Scans New HCPCS Codes and Coverage Guidelines Effective July 1, 2001 ..................... 14 Skilled Nursing Facility Consolidated Billing Clarification on HCPCS Coding Update and Part B Fee Schedule Services .......... 22 Final Medical Review Policies 29540, 33282, 67221, 70450, 76090, 76092, 82947, 86353, 93922, C1300, C1305, J0207, and J9293 ......................................................................................... 31 Outpatient Prospective Payment System Bulletin Devices Eligible for Transitional Pass-Through Payments, New Categories and Crosswalk C-codes to Be Used in Coding Devices Eligible for Transitional Pass-Through Payments ............................................................................................ 68 Features From the Medical Director 3 he Medicare A Bulletin Administrative 4 Tshould be shared with all General Information 5 health care practitioners and managerial members of the General Coverage 12 provider/supplier staff. Hospital Services 17 Publications issued after End Stage Renal Disease 19 October 1, 1997, are available at no-cost from our provider Skilled Nursing Facility -
Exploring Vigilance Notification for Organs
NOTIFY - E xploring V igilanc E n otification for o rgans , t issu E s and c E lls NOTIFY Exploring VigilancE notification for organs, tissuEs and cElls A Global Consultation e 10,00 Organised by CNT with the co-sponsorship of WHO and the participation of the EU-funded SOHO V&S Project February 7-9, 2011 NOTIFY Exploring VigilancE notification for organs, tissuEs and cElls A Global Consultation Organised by CNT with the co-sponsorship of WHO and the participation of the EU-funded SOHO V&S Project February 7-9, 2011 Cover Bologna, piazza del Nettuno (photo © giulianax – Fotolia.com) © Testi Centro Nazionale Trapianti © 2011 EDITRICE COMPOSITORI Via Stalingrado 97/2 - 40128 Bologna Tel. 051/3540111 - Fax 051/327877 [email protected] www.editricecompositori.it ISBN 978-88-7794-758-1 Index Part A Bologna Consultation Report ............................................................................................................................................7 Part B Working Group Didactic Papers ......................................................................................................................................57 (i) The Transmission of Infections ..........................................................................................................................59 (ii) The Transmission of Malignancies ....................................................................................................................79 (iii) Adverse Outcomes Associated with Characteristics, Handling and Clinical Errors -
Bone Grafting, Its Principle and Application: a Review
OSTEOLOGY AND RHEUMATOLOGY Open Journal PUBLISHERS Review Bone Grafting, Its Principle and Application: A Review Haben Fesseha, MVSc, DVM1*; Yohannes Fesseha, MD2 1Department of Veterinary Surgery and Diagnostic Imaging, School of Veterinary Medicine, Wolaita Sodo University, P. O. Box 138, Wolaita Sodo, Ethiopia 2College of Health Science, School of Medicine, Mekelle University, P. O. Box1871, Mekelle, Ethiopia *Corresponding author Haben Fesseha, MVSc, DVM Assistant Professor, Department of Veterinary Surgery and Diagnostic Imaging, School of Veterinary Medicine, Wolaita Sodo University, P. O. Box: 138, Wolaita Sodo, Ethiopia;; E-mail: [email protected] Article information Received: March 3rd, 2020; Revised: March 20th, 2020; Accepted: April 11th, 2020; Published: April 22nd, 2020 Cite this article Fesseha H, Fesseha Y. Bone grafting, its principle and application: A review. Osteol Rheumatol Open J. 2020; 1(1): 43-50. doi: 10.17140/ORHOJ-1-113 ABSTRACT Bone grafting is a surgical procedure that replaces missing bone through transferring bone cells from a donor to the recipient site and the graft could be from a patient’s own body, an artificial, synthetic, or natural substitute. Bone grafts and bone graft substitutes are indicated for a variety of orthopedic abnormalities such as comminuted fractures (due to car accidents, falling from a height or gunshot injury), delayed unions, non-unions, arthrodesis, osteomyelitis and congenital diseases (rickets, abnormal bone development) and are used to provide structural support and enhance bone healing. Autogenous, allogeneic, and artificial bone grafts are common types and sources of grafts and the advancement of allografts, synthetic bone grafts, and new operative techniques may have influenced the use of bone grafts in recent years. -

AMRITA HOSPITALS AMRITA AMRITA HOSPITALS HOSPITALS Kochi * Faridabad (Delhi NCR) Kochi * Faridabad (Delhi NCR)
AMRITA HOSPITALS HOSPITALS AMRITA AMRITA AMRITA HOSPITALS HOSPITALS Kochi * Faridabad (Delhi NCR) Kochi * Faridabad (Delhi NCR) A Comprehensive A Comprehensive Overview Overview A Comprehensive Overview AMRITA INSTITUTE OF MEDICAL SCIENCES AIMS Ponekkara P.O. Kochi, Kerala, India 682 041 Phone: (91) 484-2801234 Fax: (91) 484-2802020 email: [email protected] website: www.amritahospitals.org Copyright@2018 AMRITA HOSPITALS Kochi * Faridabad (Delhi-NCR) A COMPREHENSIVE OVERVIEW A Comprehensive Overview Copyright © 2018 by Amrita Institute of Medical Sciences All rights reserved. No portion of this book, except for brief review, may be reproduced, stored in a retrieval system, or transmitted in any form or by any means —electronic, mechanical, photocopying, recording, or otherwise without permission of the publisher. Published by: Amrita Vishwa Vidyapeetham Amrita Institute of Medical Sciences AIMS Ponekkara P.O. Kochi, Kerala 682041 India Phone: (91) 484-2801234 Fax: (91) 484-2802020 email: [email protected] website: www.amritahospitals.org June 2018 2018 ISBN 1-879410-38-9 Amrita Institute of Medical Sciences and Research Center Kochi, Kerala INDIA AMRITA HOSPITALS KOCHI * FARIDABAD (DELHI-NCR) A COMPREHENSIVE OVERVIEW 2018 Amrita Institute of Medical Sciences and Research Center Kochi, Kerala INDIA CONTENTS Mission Statement ......................................... 04 Message From The Director ......................... 05 Our Founder and Inspiration Sri Mata Amritanandamayi Devi .................. 06 Awards and Accreditations ......................... -

Consent for Bone Grafting
Consent for Bone Grafting Grafting Procedure: __________________________________________________________________________ I understand that bone grafting and barrier membrane procedures include inherent risks such as, but not limited to the following: 1. Pain. Some discomfort is inherent in any oral surgery procedure. Grafting with materials that do not have to be harvested from your body is less painful because they do not require a donor site surgery, but pos-toperative pain is still likely. It can be largely controlled with pain medications and applying a cold compression to the surgical site. 2. Infection. No matter how carefully surgical sterility is maintained, it is possible, because of the existing non-sterile oral environment, for infections to occur post-operatively. At times these may be a serious nature. Should severe swelling occur, particularly accompanied with fever or malaise, professional attention should be received as soon as possible. 3. Bleeding, bruising, and swelling. Some moderate bleeding may last several hours. If profuse, you must contact us as soon as possible. Some swelling is normal, but if severe, you should notify us. Swelling usually starts to subside after about 48 hours. Bruises may persist for a week or so. 4. Loss of all or part of the graft. Success with bone and membrane grafting is high. Nevertheless, it is possible that the graft could fail. Despite meticulous surgery, particulate bone graft materials can migrate out of the surgery site and be lost. A membrane graft could start to dislodge. If so, the doctor should be notified. You compliance is essential to assure success. 5. Types of graft material. -

78581/2020/Estt-Ne Hr
105 78581/2020/ESTT-NE_HR 1| T a r i f f - AIMS 106 78581/2020/ESTT-NE_HR INDEX 1. General Information ( Section A) 3 i. Out Patient Department ii. Ambulance Charges 2. General Information ( Section B) 5 i. Bed charges ii. In patient Consultation fees iii. Billing Of Surgery Anesthesia and OT Charges iv. Billing Of Surgery /Procedure/ others 3. LAB 9 4. Outsouce Lab 16 5. Blood Bank 64 6. Imaging & Radiodiagnosis 65 7. Non – Invasive Lab 80 8. Anesthesia 82 9. Cardiology and Cardiac Surgery 84 10. Critical Care Services 89 11. Baby Care 91 12. Common Procedure 94 13 Dental 94 14 Dermatology 101 15 E N T 105 16 Gastroenterology 110 17 Maxillo Facial Surgery 113 18 Nephrology 116 19 Neuro Diagnostic Lab 118 20 Oncology 112 21 Ophthalmology 136 22 Orthopedies 142 23 OBS & Gynaecology 149 24 Physiotherapy 154 25 Respiratory Medicine 156 26 Surgery & Major Procedures i. General Surgery 158 ii. Pediatric Surgery 165 iii. PlasticSurgery 170 iv. Neuro Surgery 182 27 Urology 185 28 Interventional Radiology 192 29 Interventional Pain Management 194 30 Paediatric Cardiac Surgery 197 31 Bed Side Service Charges200 2| T a r i f f - AIMS 107 78581/2020/ESTT-NE_HRSection – A GENERAL INFORMATION OUT PATIENT DEPARTMENT OPD Consultations: Superspeciality OPD Consultation * Rs. 700 Specialty OPD Consultation** Rs. 400 to 800 Note: OPD Timing Monday- Saturday ( 8:00AM – 7:00PM) *Super specialty Departments – Cardiac Surgery, Cardiology, Neurology, Neurosurgery, Oncology, Respiratory Medicine, Urology, Plastic Surgery, Gastroenterology, Endocrinology, Paediatric -

Informed Consent for Bone Grafting Surgery
INFORMED CONSENT FOR BONE GRAFTING SURGERY BONE GRAFTING The bone grafting procedure involves opening the gums in the area to expose the existing bone. This is then followed by placing bone material in such a manner so as to augment the existing bone horizontally or vertically. A protective barrier or membrane may then placed over the grafted bone for protection. The gums are then closed over and sutured (stitched) in place to completely cover the bone grafted area. A healing time of 4-6 months is then typically allowed for the bone graft to “take”, mature, and integrate with the surrounding native bone. As discussed, the bone graft material and membrane we’ll be using is derived from a donor source (animal or human) or synthetic. The materials I use have been documented to be safe and reliable. Expected Benefits The purpose of bone grafting in your case would be to increase the width of the existing bone to allow for proper implant placement. It may also help to harmonize the esthetics of the region. The amount of volume achieved is influenced by a number of factors. As such, some cases require multiple grafts to achieve the necessary volume in order to place an implant of a specific size. Principal Risks and Complications Although bone grafting of localized areas to increase the width of existing bone has been shown in clinical studies to be a predictable procedure, in some cases, patients do not respond successfully to the procedure and may require revision procedures to attain the desired result. Because each patient's condition is unique, the procedure may not be successful in preserving function or appearance for the long- term. -

Journal of Vaccines, Immunology and Immunopathology Rijkers GT
Journal of Vaccines, Immunology and Immunopathology Rijkers GT. J Vaccines Immunol 5: 148. Review Article DOI: 10.29011/2575-789X.000148 The Arrest of Christ: Autotransplantation from Miracle to Medical Procedure Ger T. Rijkers1,2* 1Department of Science, University College Roosevelt, Lange Noordstraat, CB Middelburg, The Netherlands 2Laboratory for Medical Microbiology and Immunology, St. Elisabeth Hospital, Tilburg, The Netherlands *Corresponding author: GT Rijkers, Department of Science, University College Roosevelt, Lange Noordstraat 1, CB Middelburg, The Netherlands Citation: Rijkers GT (2020) The Arrest of Christ: Autotransplantation from Miracle to Medical Procedure. J Vaccines Immunol 5: 148. DOI: 10.29011/2575-789X.000148 Received Date: 01 January, 2020; Accepted Date: 13 January, 2020; Published Date: 20 January, 2020 Abstract During the arrest of Christ, one of his disciples, Simon Peter, cut off the ear of a servant of Caiaphas. Christ put the ear back, a miracle and the first recorded autotransplantation. Currently, autotransplantation is an established procedure in reconstructive dental and bone surgery. Autotransplantation of splenic fragments can retain spleen function after splenectomy. Following pancreatectomy for chronic pancreatitis or benign or malignant diseases of the pancreas, islet autotransplantation can prevent diabetes. Autotransplantation of hematopoietic stem cells enables reconstitution of hematopoiesis after intense chemo and/or radiotherapy for leukemia and lymphoma. The development of biomedical technology to generate induced pluripotent stem cells, gene editing with CRISPR Cas, and in vitro organoid cultures opens the possibility to treat a wide array of inborn and acquired diseases by autotransplantation. Introduction The Temptation of St. Anthony (1500-1510) is an altarpiece by Jheronimus Bosch. Colorful altarpieces were closed during the Lenten period, the 40 days’ penitential preparation for Eastern, or just during the final week before Eastern, the Holy Week. -

Skin Grafting in the Dog Elroy C
Volume 19 | Issue 3 Article 1 1957 Skin Grafting in the Dog Elroy C. Jensen Iowa State College Follow this and additional works at: https://lib.dr.iastate.edu/iowastate_veterinarian Part of the Small or Companion Animal Medicine Commons, and the Veterinary Anatomy Commons Recommended Citation Jensen, Elroy C. (1957) "Skin Grafting in the Dog," Iowa State University Veterinarian: Vol. 19 : Iss. 3 , Article 1. Available at: https://lib.dr.iastate.edu/iowastate_veterinarian/vol19/iss3/1 This Article is brought to you for free and open access by the Journals at Iowa State University Digital Repository. It has been accepted for inclusion in Iowa State University Veterinarian by an authorized editor of Iowa State University Digital Repository. For more information, please contact [email protected]. SKIN GRAFTING In The Dog Elroy C. J,ensen, D.V.M. THERE are several histological factors the arm instead of from the forehead. which have made skin grafting pos This technique is now known as the Ital sible in man and animals. First, the com ian method of rhinoplasty. Free skin parative ease which epithelium can regen grafting started early in the 19th century erate is a factor. This new growth of tis by two charlatans which is related by sue occurs either from the periphery of a Baroni, the physi'Ologist, "A woman wound or it may result from proliferation named Gamba Curat, in order to show of the external root sheath of the hair the efficiency of an ointment she was sel follicles providing the dermis has not been ling, cut a piece of skin from her thigh completely destroyed.