SUST Repository
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anatomy of Small Intestine Doctors Notes Notes/Extra Explanation Please View Our Editing File Before Studying This Lecture to Check for Any Changes
Color Code Important Anatomy of Small Intestine Doctors Notes Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives: At the end of the lecture, students should: List the different parts of small intestine. Describe the anatomy of duodenum, jejunum & ileum regarding: the shape, length, site of beginning & termination, peritoneal covering, arterial supply & lymphatic drainage. Differentiate between each part of duodenum regarding the length, level & relations. Differentiate between the jejunum & ileum regarding the characteristic anatomical features of each of them. Abdomen What is Mesentery? It is a double layer attach the intestine to abdominal wall. If it has mesentery it is freely moveable. L= liver, S=Spleen, SI=Small Intestine, AC=Ascending Colon, TC=Transverse Colon Abdomen The small intestines consist of two parts: 1- fixed part (no mesentery) (retroperitoneal) : duodenum 2- free (movable) part (with mesentery) :jejunum & ileum Only on the boys’ slides RELATION BETWEEN EMBRYOLOGICAL ORIGIN & ARTERIAL SUPPLY مهم :Extra Arterial supply depends on the embryological origin : Foregut Coeliac trunk Midgut superior mesenteric Hindgut Inferior mesenteric Duodenum: • Origin: foregut & midgut • Arterial supply: 1. Coeliac trunk (artery of foregut) 2. Superior mesenteric: (artery of midgut) The duodenum has 2 arterial supply because of the double origin The junction of foregut and midgut is at the second part of the duodenum Jejunum & ileum: • Origin: midgut • Arterial -
Introduction to Anatomy of the Abdomen the Region Between: Diaphragm and Pelvis
Introduction to Anatomy of the Abdomen The region between: Diaphragm and pelvis. Boundaries: • Roof: Diaphragm • Posterior: Lumbar vertebrae, muscles of the posterior abdominal wall • Infrerior: Continuous with the pelvic cavity, superior pelvic aperture • Anterior and lateral: Muscles of the anterior abdominal wall Topography of the Abdomen (PLANES)..1/2 TRANSVERSE PLANES • Transpyloric plane : tip of 9th costal cartilages; pylorus of stomach, L1 vertebra level. • Subcostal plane: tip of 10th costal cartilages, L2-L3 vertebra. • Transtubercular plane: L5 tubercles if iliac crests; L5 vertebra level. • Interspinous plane: anterior superior iliac spines; promontory of sacrum Topography of the Abdomen (PLANES)..2/2 VERTICAL PLANES • Mid-clavicular plane: midpoint of clavicle- mid-point of inguinal ligament. • Semilunar line: lateral border of rectus abdominis muscle. Regions of the Abdomen..1/2 4 2 5 9 regions: • Umbilical (1) 8 1 9 • Epigastric (2) • Hypogastric (Suprapubic) (3) • Right hypochondriacum (4) 6 3 7 • Left hypochondrium (5) • Right Iliac (Inguinal) (6) • Left Iliac (Inguinal) (7) • Right lumbar (8) • Left lumbar (9) Regions of the Abdomen..2/2 1 2 4 Quadrants: • Upper right quadrant (1) 3 4 • Upper left quadrant (2) • Lower right quadrant (3) • Lower left quadrant (4) Dermatomes Skin innervation: • lower 5 intercostal nerves • Subcostal nerve • L1 spinal nerve (ilioinguinal+iliohypogastric nerves). Umbilical region skin = T10 Layers of Anterior Abdominal Wall Skin Fascia: • Superficial fascia: • Superficial fatty layer(CAMPER’S -
5- Small Intestines Edited.Pdf
Small Intestines Lecture (5) . Important . Doctors Notes Please check our Editing File . Notes/Extra explanation هذا العمل مبني بشكل أساسي على عمل دفعة 436 مع المراجعة {ومنْْيتو َ ّكْْع َلْْا ِّْللْفَهُوْْحس بهْ} َ َ َ َ َ َ َ َ َ ُ ُ والتدقيق وإضافة المﻻحظات وﻻ يغني عن المصدر اﻷساسي للمذاكرة . Objectives At the end of the lecture, students should be able to: List the different parts of small intestine. Describe the anatomy of duodenum, jejunum & ileum regarding: the shape, length, site of beginning & termination, peritoneal covering, arterial supply & lymphatic drainage. Differentiate between each part of duodenum regarding the length, level & relations. Differentiate between the jejunum & ileum regarding the characteristic anatomical features of each of them. Abdomen o What is Mesentery? o It is a double layer attach the intestine to abdominal wall. If it has mesentery it is freely moveable. o The small intestines consist of two parts: • Fixed part (without mesentery) (retroperitoneal): duodenum • Free (movable) part (with mesentery): jejunum & ileum Jejunum & ileum Mesentery of SI L= liver, S=Spleen, SI=Small Intestine, AC=Ascending Colon, TC=Transverse Colon To see the second layer you should Abdomen (this slide is not important) remove the parietal peritoneum of posterior abdominal wall. The second layer consists of: Dr.ahmed fathalla’s notes: We you remove the anterior 1- ascending colon - any structure invaginates the abdominal wall, you will find 2- cecum peritoneum has a certain the most superficial 3- descending colon degree of mobility 4- duodenum structures are: 5- pancreas - we have three levels related to 1- liver abdominal structures: 2- stomach 6- spleen 1- (Part of the GIT) it is mobile and 3- transvers colon And behind the 2nd layer, there are completely covered by the 4- small intestine) the other non-GIT structures like peritoneum, because it has kidney, Aorta and IVC invaginated the peritoneum. -

Unit #2 - Abdomen, Pelvis and Perineum
UNIT #2 - ABDOMEN, PELVIS AND PERINEUM 1 UNIT #2 - ABDOMEN, PELVIS AND PERINEUM Reading Gray’s Anatomy for Students (GAFS), Chapters 4-5 Gray’s Dissection Guide for Human Anatomy (GDGHA), Labs 10-17 Unit #2- Abdomen, Pelvis, and Perineum G08- Overview of the Abdomen and Anterior Abdominal Wall (Dr. Albertine) G09A- Peritoneum, GI System Overview and Foregut (Dr. Albertine) G09B- Arteries, Veins, and Lymphatics of the GI System (Dr. Albertine) G10A- Midgut and Hindgut (Dr. Albertine) G10B- Innervation of the GI Tract and Osteology of the Pelvis (Dr. Albertine) G11- Posterior Abdominal Wall (Dr. Albertine) G12- Gluteal Region, Perineum Related to the Ischioanal Fossa (Dr. Albertine) G13- Urogenital Triangle (Dr. Albertine) G14A- Female Reproductive System (Dr. Albertine) G14B- Male Reproductive System (Dr. Albertine) 2 G08: Overview of the Abdomen and Anterior Abdominal Wall (Dr. Albertine) At the end of this lecture, students should be able to master the following: 1) Overview a) Identify the functions of the anterior abdominal wall b) Describe the boundaries of the anterior abdominal wall 2) Surface Anatomy a) Locate and describe the following surface landmarks: xiphoid process, costal margin, 9th costal cartilage, iliac crest, pubic tubercle, umbilicus 3 3) Planes and Divisions a) Identify and describe the following planes of the abdomen: transpyloric, transumbilical, subcostal, transtu- bercular, and midclavicular b) Describe the 9 zones created by the subcostal, transtubercular, and midclavicular planes c) Describe the 4 quadrants created -

Pin Point Your Insides Bernard Anastasi M
Pin Point Your Insides Bernard Anastasi M. D. Every medical student knows the approximate whereabouts of the important organs. However, the aim of these diagrams i~ to enable the ~tudellt to map out, in the order given,a series ot important points in relation to bone and plane landmarks from which the surface projection of internal organs can be accurately obtained and remembered. Reference: Gray's Anatomy. '-..------ o pI. a. ne HEART LIVER Left Border apex beat - 5th intercostal space, 9cm from Lower Border: • right 10th costal cartilage. • median plane, below and medial to left nipple. • fundus of gall bladder - 4.5cm to right of upper point - lower border of 2nd costal median plane, below 9th right costal cartilage. • cartilage, 1.2cm from sternal margin. • crosses infrasternal angle at intersection of Right Border upper point - upper border of 3rd costal median and transpyloric planes. • cartilage, 1.2cm from sternal margin. • tip of 8th left costal cartilage. widest point - 4th intercostal space, 3.7cm Upper Border: • left end - below and medial to left nipple. • from medilln plane. • passes through xiphisternal joint. lower point - 6th costal cartilage. • right end - below right nipple. Lower Border: • passes through xiphisternal angle. 21 m idaxil/a".y lira e LUNGS AND PLEURAE Right Lung and Pleura: • lower edge of neck of 1st rib. • sterno-clavicular joint. • sternal an~le in midline. • xiphisternal joint. • 7th costal cartilage. • 8th rib in midaxillary line (lung). • T. 10 (lung). • T. 12 (Pleura) • 10th rib in midaxillary line (pleura). Left Lung and Pleura: N.B. same as right, except: • diverge laterally at level of 4th costal cartilage. -

L1 Esophagus & Stomach.Pdf
MIND MAP C6 • The esophagus begins as continuation of pharynx • Site of 1st esophageal constriction Dr. Ahmed Kamal T4 • Sternal angle Esophagus & Stomach • Crossing of esophagus with the aortic arch & the left main bronchus (2nd 22, 23 relations ,24 blood supply constriction) Khan academy medicine T10 • The esophagus pierces the diaphragm to join stomach Esophagus & Stomach • 3rd constriction Anatomy Zone T11 The end of esophagus 3D Anatomy Tutorial L1 Transpyloric plane (site of pyloric canal) [email protected] ESOPHAGUS Constitutes 3 parts ① Cervical ② Thoracic (longest part) ③ Abdominal (shortest part) It’s a 25cm long tubular structure extending from the Pharynx at C6 and it pierces the diaphragm at T10 and joins the stomach. In the thorax, it passes downward and to the left through superior mediastinum then to posterior mediastinum. At the level of the sternal angle, the aortic arch pushes the esophagus again to the midline. Diaphragmatic opening: . Esophagus . 2 Vagi . Branches of Left gastric vessels . Lymphatic vessels Fibers from the right crus of the diaphragm form a sling around the esophagus. Relations Part Anterior Posterior Laterally Cervical Trachea and Vertebral column Lobes of the Thyroid gland the recurrent laryngeal nerves Thoracic ① Trachea ① Bodies of the On the Right side: ② Left recurrent thoracic • Right mediastinal vertebrae laryngeal pleura nerve ② Thoracic duct ③ Azygos vein • Terminal part of the ③ Left principal ④ Right posterior bronchus azygos vein. intercostal arteries On the Left side: ④ Pericardium ⑤ Descending ⑤ Left atrium thoracic aorta (at • Left mediastinal the lower end) pleura • Left subclavian artery • Aortic arch • Thoracic duct Abdomen Left lobe of liver Left crus of diaphragm ___________ Cervical part of Esophagus Thoracic part of Esophagus Anterior Posterior R Lateral L Barium X-ray of the upper gastrointestinal tract Left atrium The esophagus is closely related to the left atrium. -

1 Anatomy of the Abdominal Wall 1
Chapter 1 Anatomy of the Abdominal Wall 1 Orhan E. Arslan 1.1 Introduction The abdominal wall encompasses an area of the body boundedsuperiorlybythexiphoidprocessandcostal arch, and inferiorly by the inguinal ligament, pubic bones and the iliac crest. Epigastrium Visualization, palpation, percussion, and ausculta- Right Left tion of the anterolateral abdominal wall may reveal ab- hypochondriac hypochondriac normalities associated with abdominal organs, such as Transpyloric T12 Plane the liver, spleen, stomach, abdominal aorta, pancreas L1 and appendix, as well as thoracic and pelvic organs. L2 Right L3 Left Visible or palpable deformities such as swelling and Subcostal Lumbar (Lateral) Lumbar (Lateral) scars, pain and tenderness may reflect disease process- Plane L4 L5 es in the abdominal cavity or elsewhere. Pleural irrita- Intertuber- Left tion as a result of pleurisy or dislocation of the ribs may cular Iliac (inguinal) Plane result in pain that radiates to the anterior abdomen. Hypogastrium Pain from a diseased abdominal organ may refer to the Right Umbilical Iliac (inguinal) Region anterolateral abdomen and other parts of the body, e.g., cholecystitis produces pain in the shoulder area as well as the right hypochondriac region. The abdominal wall Fig. 1.1. Various regions of the anterior abdominal wall should be suspected as the source of the pain in indi- viduals who exhibit chronic and unremitting pain with minimal or no relationship to gastrointestinal func- the lower border of the first lumbar vertebra. The sub- tion, but which shows variation with changes of pos- costal plane that passes across the costal margins and ture [1]. This is also true when the anterior abdominal the upper border of the third lumbar vertebra may be wall tenderness is unchanged or exacerbated upon con- used instead of the transpyloric plane. -
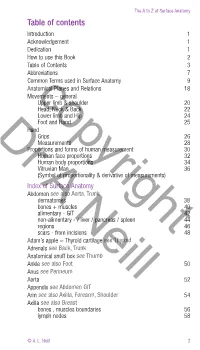
Pages-From-A-Z-Of-Surface-Anatomy-Excerpts-With-WM.Pdf
The A to Z of Surface Anatomy Table of contents Introduction 1 Acknowledgement 1 Dedication 1 How to use this Book 2 Table of Contents 3 Abbreviations 7 Common Terms used in Surface Anatomy 9 Anatomical Planes and Relations 18 Movements – general copyrightUpper limb & shoulder 20 Head, Neck & Back 22 Lower limb and Hip 24 Foot and Hand 25 Hand Grips 26 Dr Measurements 28 Proportions and forms of human measurement 30 Human face proportions 32 Human body proportions 34 Vitruvian Man 36 (Symbol of proportionality & derivative of measurements) IndexA of Surface Anatomy Abdomen see also Aorta, Trunk dermatomes 38 bones + muscles 40 alimentary - GIT 42 non-alimentary Neill- / liver / pancreas / spleen 44 regions 46 scars - from incisions 48 Adam’s apple = Thyroid cartilage see Thyroid Adrenals see Back, Trunk Anatomical snuff box see Thumb Ankle see also Foot 50 Anus see Perineum Aorta 52 Appendix see Abdomen GIT Arm see also Axilla, Forearm, Shoulder 54 Axilla see also Breast bones , muscles boundaries 56 lymph nodes 58 © A. L. Neill 3 The A to Z of Surface Anatomy Back lower 60 upper see Chest Belly see Abdomen Belly button see Abdomen Bladder see Kidneys, Pelvis, Uterus Breast see also Axilla arterial 62 lymphatic & venous 63 Buttock see Gluteum Caecum see Abdomen GIT Carpal tunnelcopyright see Hand Chest Wall see also Abdomen, Lungs great vessels 64 heart 65 heart valves sounds 66 incision or marks = scars 67 Drlungs & pleura 68 Cubital Fossa 72 Diaphragm + assoc structures see also Oesophagus 74 Duodenum see Abdomen GIT Kidneys Ear 76 Elbow see arm, cubital fossa, forearm Eye A 78 Face arteries 82 bones see also TMJ 88 Facial N 90 muscles Neill 92 veins 94 Femoral triangle contents & borders 96 muscles & bones 98 Finger see Hand Flexor Retinaculum see Hand Foot dorsum bones 100 tendons 102 sole fascia / muscle layers 104 bones / dermatomes 109 Forearm bones 112 muscles 114 4 © A. -

ABDOMEN 1. Regarding Divisions of Anterior Abdominal Wall
ABDOMEN 1. Regarding divisions of anterior abdominal wall: A. Midclavicular line joins the midpoint of clavicle to the midpoint of inguinal ligament. B. Intertubercular plane joins the ischial tuberosities. c. Transpyloric plane lies at the lowest costal margin. D. All of the above is false. E. All of the above is true. 2. Regarding inguinal ligament: A. It attaches to anterior superior iliac spine & pubic tubercle. B. It is the lower rolled in aponeurotic edge of internal oblique. c. It attaches to fascia lata. D. Inguinal canal occupies the whole length inguinal ligament. E. All of the above. 3. Regarding the rectus sheath: A. It lies wholly anterior to rectus abdominis between the costal margin & the arcuate line. B. It encloses the rectus abdominis between the costal margin & the arcuate line. C. The arcuate (semicircular) line is the lower free margin of internal oblique D. Semilunar line is the blood less groove which internal oblique aponeurosis splits to enclose rectus abdominis E. All of the above 4. Which of the following is FALSE regarding anterior abdominal wall? A. Neurovascular plane lies between the internal oblique & transversus abdominis layers B. Anterior cutaneous nerve is the branch of posterior intercostal nerve (T7-11). c. External oblique is supplied by the lateral cutaneous branch of posterior intercostal nerve (T7-11). D. Anastomosis of superior & inferior epigastric artery represents the communication between the internalthoracic & external iliac arteries E. Lymph nodes lie within the neurovascular plane. 5. Melanoma on the leftiliac fossa may spread to: A. pectoral lymph nodes B. medial group of inguinal lymph nodes C. -
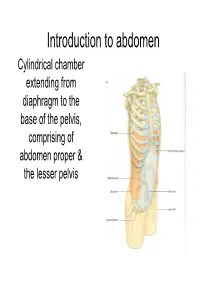
Introduction to Abdoman
Introduction to abdomen Cylindrical chamber extending from A diaphragm to the base of the pelvis, comprising of abdomen proper & the lesser pelvis -+------- Lower limb • Abdomen proper & lesser pelvis communicate with each other at the plane of inlet into lesser pelvis (upper border of pubic symphysis,pubic crests, arcuate line of innominate bones,sacral promontary) pelvis Pelvic inlet Inguinal ligament • Contents of Abdomen proper:- Most of the digestive tube, Liver, pancreas, spleen, kidneys, ureters (in part), supra renal gland & various blood &lymph vessels lymph nodes &nerves • Contents of lesser pelvis:- Terminal parts of ureters, urinary bladders, the sigmoid colon, rectum some coils of ileum, internal genitalia, blood & lymph vesels, lymph nodes & nerves Functions • Houses & protects major viscera Rib cage Assists in breathing of Relaxation of diaphragm diaphragm Relaxation of abdominal muscles Contraction of abdominal muscles Expiration Inspiration Changes in the intra abdominal pressure Laryngeai cav'ity c·1os 1erd Cr0ntrac ion of abdominal wal I ncrease in intra- abdominal pressure _..l,....._ Mictu ·ition Child birth Defecation Component parts ony Frame,vork of Abdomen • Wall- Skeletal elements Muscles • Muscles:- Superficial fascia • Anteriorly a Fatty layer Membranous layer (Camper's) (Scarpa's) segmented Transversalis fascia muscle Rectus [=E<trapedtoceru..; abdominis Parietal peritoneum Visceral peritoneum • Anterolateraly External oblique, internal oblique & trasversus abdominis ~.34 Transverse section showing the layers of the abdominal wa ll. Po~ t ei·i 01· .--\. lJcl 0111in a] \,-a]] • Posteriorly- Quadratus lumborum, psoas major & iliacus Abdominal regions Subcostal plane Midclavicular planes ,7 I I Left lowe ( I. _ quadr;mt Transumbilical plane Median plane Transtubercular plane Regions on anterior abdominal wall vertic~I plane Left ve rtical p,lane ' Hypochondriac Hypochondriac L / ' / ' ,/ '' / ' ✓ ' Subcostal plane ,-.;;'-~_,,:;.....,,,___ --i--------------~+-----'_ ......;;_..,,___. -
Anatomy of the Pancreas and the Spleen
BASIC SCIENCE Relations Anatomy of the pancreas and The pancreatic head lies in the C-curve of the duodenum. Infer- omedially, it sends out its uncinate process, that hooks around the spleen the superior mesenteric vessels, as these descend from behind the pancreas into the mesenteric root. Anteriorly, the lesser sac Harold Ellis separates it from the posterior aspect of the stomach. A collection of fluid into the lesser sac following an episode of acute pancreatitis results in a so-called ‘pseudocyst of the pancreas’. To Abstract the left, the tail of the gland abuts against the spleen. Superiorly, The pancreas comprises a head, uncinate process, neck, body and tail. It lies the tortuous splenic artery runs along the upper border of the retroperitoneally, roughly at the transpyloric plane, separated from the pancreas (Figure 2) and constitutes its main blood supply, stomach in front by the lesser sac. Its tail abuts onto the spleen. It has a (perhaps it would be better named the ‘pancreatico-splenic ar- rich blood supply, from the superior and inferior pancreatico-duodenal tery’, which would prevent examination candidates forgetting arteries and, particularly, from the tortuous splenic artery, which lies the most important artery supplying the pancreas!). Posteriorly, along its superior border. Its corresponding veins drain into the portal sys- from right to left, the gland lies on the inferior vena cava, the tem. It has both exocrine (digestive enzymes), and endocrine secretory func- commencement of the portal vein, the aorta and superior tions, the latter, most importantly, being the secretion of insulin from the mesenteric vessels, the left crus of the diaphragm, the left kidney, islet cells. -

EPIGASTRIC / EPIGASTRIUM the Abdomen Is Divided Into Nine
EPIGASTRIC / EPIGASTRIUM The abdomen is divided into nine regions, by imaginary planes, two horizontal and two sagittal. Horizontal Planes: (1) Upper transverse = transpyloric plane (halfway between the jugular notch and the upper border of the symphysis pubis) - this indicates the margin of the transpyloric plane, which in most cases cuts through the pylorus. (2) Lower transverse = transtubercular plane (midway between the upper transverse and the upper border of the symphysis pubis) - it corresponds to that passing through the iliac tubercles By means of these horizontal planes the abdomen is divided into three zones named from above: subcostal, umbilical, and hypogastric zones. Sagittal Planes: Each of the three zones is further subdivided into three regions by the two sagittal planes, which are indicated on the surface by a right and a left lateral line drawn vertically through points halfway between the anterior superior iliac spines and the middle line: (1) Upper zone: middle region = epigastric & two lateral regions = right and left hypochondriac (2) Middle zone: central region = umbilical & the two lateral regions = right and left lumbar (3) Lower zone: middle region = hypogastric or pubic & two lateral = right and left iliac or inguinal IN SUMMARY – the epigastric or epigastrium is the middle region in the upper zone of the abdomen: SOLAR PLEXUS The Celiac Plexus (Plexus Cœliacus; Solar Plexus): The celiac plexus, the largest of the three sympathetic plexuses, is situated at the level of the upper part of the first lumbar vertebra and is composed of two large ganglia, the celiac ganglia, and a dense net-work of nerve fibers uniting them together.