Norbuprenorphine Pharmacokinetics and Pharmacodynamics: First in Man Evaluation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cleveland Clinic Laboratories
Cleveland Clinic Laboratories Quantitative Urine Pain Management Drug Measurement with HPLC-MS/MS Background Information enzymatic hydrolysis is much milder, but needs longer incubation time to achieve sufficient (>80%) hydrolysis Pain management drugs are among the most prescribed efficiency.7 medications, and they are also the most abused class of prescription drugs.1-2 Therefore, many states including Ohio Cleveland Clinic Laboratories offer an HPLC-MS/MS method have enacted laws governing the prescription of pain for quantitative screening of 11 pain management drugs and management drugs. Patients enrolled in pain management five other commonly abused drugs in urine.8 In this method, programs need to be monitored for compliance, which total drug concentration is measured after enzymatic hydroly- means appropriate use of prescribed drugs and abstinence sis. This assay also includes an adulteration test using urine from non-prescribed drugs. test strips to ensure specimen quality. In addition to pain management, this test can also be used for monitoring Urine is the most commonly used specimen in monitoring patient compliance in rehabilitation programs. pain management and illicit drug use. A single urine specimen can be tested for a number of drugs. Immunoassay (IA) can The high sensitivity of this method is capable of detecting be used as a screening method, but it lacks specificity and drug manufacturing impurities. As an example, codeine is a sensitivity. For example, most immunoassay tests cannot known manufacturing impurity in morphine (~0.04%) and distinguish various opiate drugs and cannot detect oxymor- can be detected by this method.9 3-4 phone at all. -

(12) United States Patent (10) Patent No.: US 8.492,564 B2 Beguin Et Al
USOO8492.564B2 (12) United States Patent (10) Patent No.: US 8.492,564 B2 Beguin et al. (45) Date of Patent: Jul. 23, 2013 (54) SALVINORIN DERIVATIVES AND USES Béguin et al., “Differential signaling properties at the kappa opioid THEREOF receptor of 12-epi-Salvinorin A and its analogues. Bioorg Med Chem Lett. 22: 1023-1026, 2012. (75) Inventors: Cecile Beguin, Lexington, MA (US); Béguin et al., “Modification of the furan ring of salvinorin A: iden Justin Stephen Potuzak, Millis, MA tification of a selective partial agonist at the kappa opioid receptor.” 17: 1370-1380, Epub Dec. 14, 2008. (US); Thomas Anthony Munro, Béguinet al., "N-Methylacetamide Analog of Salvinorin A: A Highly Cambridge, MA (US); Katharine K. Potent and Selective K-Opioid Receptor Agonist with Oral Efficacy.” Duncan, San Diego, CA (US); William J. Pharmacol. Exp. Ther, 324; 188-195 (2008). A. Carlezon, Lincoln, MA (US); Bruce Béguin et al., “Synthesis and In Vitro Evaluation of Salvinorin A M. Cohen, Lexington, MA (US); Analogues: Effect of Configuration at C(2) and Substitution at Lee-yuan Liu-Chen, Media, PA (US) C(18).” Bioorg. Med. Chem. Lett. 16:4679-4685 (2006). Béguin et al., “Synthesis and InVitro Pharmacological Evaluation of (73) Assignees: The McLean Hospital Corporation, Salvinorin A Analogues Modified at C(2).” Bioorg. Med. Chem. Lett. Belmont, MA (US); Temple University 15:2761-2765 (2005). School of Medicine, Philadelphia, PA Bigham et al., “Divinatorins A-C, New Neoclerodane Diterpenoids from the Controlled SageSalvia divinorum,'.J. Nat. Prod 66: 1242 (US) 1244 (2003). Bikbulatov et al., “Short synthesis of a novel class of salvinorin A (*) Notice: Subject to any disclaimer, the term of this analogs with hemiacetalic structure.” Tetrahedron Lett. -

ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update
The ASAM NATIONAL The ASAM National Practice Guideline 2020 Focused Update Guideline 2020 Focused National Practice The ASAM PRACTICE GUIDELINE For the Treatment of Opioid Use Disorder 2020 Focused Update Adopted by the ASAM Board of Directors December 18, 2019. © Copyright 2020. American Society of Addiction Medicine, Inc. All rights reserved. Permission to make digital or hard copies of this work for personal or classroom use is granted without fee provided that copies are not made or distributed for commercial, advertising or promotional purposes, and that copies bear this notice and the full citation on the fi rst page. Republication, systematic reproduction, posting in electronic form on servers, redistribution to lists, or other uses of this material, require prior specifi c written permission or license from the Society. American Society of Addiction Medicine 11400 Rockville Pike, Suite 200 Rockville, MD 20852 Phone: (301) 656-3920 Fax (301) 656-3815 E-mail: [email protected] www.asam.org CLINICAL PRACTICE GUIDELINE The ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update 2020 Focused Update Guideline Committee members Kyle Kampman, MD, Chair (alpha order): Daniel Langleben, MD Chinazo Cunningham, MD, MS, FASAM Ben Nordstrom, MD, PhD Mark J. Edlund, MD, PhD David Oslin, MD Marc Fishman, MD, DFASAM George Woody, MD Adam J. Gordon, MD, MPH, FACP, DFASAM Tricia Wright, MD, MS Hendre´e E. Jones, PhD Stephen Wyatt, DO Kyle M. Kampman, MD, FASAM, Chair 2015 ASAM Quality Improvement Council (alpha order): Daniel Langleben, MD John Femino, MD, FASAM Marjorie Meyer, MD Margaret Jarvis, MD, FASAM, Chair Sandra Springer, MD, FASAM Margaret Kotz, DO, FASAM George Woody, MD Sandrine Pirard, MD, MPH, PhD Tricia E. -

2019 Opioid Overdose County-Level Data Tables
Opioid Overdose Surveillance Preliminary County Level Data Tables Georgia, 2019 These data describe fatal (mortality) and nonfatal (morbidity) opioid-involved overdoses in Georgia during 2019, including those related to prescription opioids and illicit opioids such as heroin, fentanyl, and fentanyl analogs. Opioid overdose data were analyzed by the Georgia Department of Public Health (DPH) Epidemiology Program, Drug Surveillance Unit, using Georgia hospitalization and emergency department (ED) visit discharge data, and DPH Vital Records death data. Contents Case Definitions and Data Source Information ....................................................................................................................................................................................... 2 Year-by-Year Data Tables ....................................................................................................................................................................................................................... 5 Demographics Data Tables ...................................................................................................................................................................................................................... 6 County Level Data Tables........................................................................................................................................................................................................................ 7 For more information: • Georgia overdose -

The Importance of Norbuprenorphine Cross Reactivity In
The importance of norbuprenorphine cross-reactivity in a buprenorphine urine immunoassay 1Michael Vincent, 1Kim Huynh, 2James Bourland, 1 Guohong Wang, 1Cynthia Coulter, 1Christine Moore 1Immunalysis Corporation, Pomona, CA 2 Ameritox LLC, Midland, TX Introduction Methods Results and Discussion Summary Buprenorphine, an opiate antagonist is In the MCG assay: since extensive cross- At the concentrations described, the metabolized by N-dealkylation to reactivity with opiates and opiate MCG 20ng/mL performance of the assays was as follows: norbuprenorphine, followed by glucuronide glucuronides has been observed, the use of + - conjugation of both buprenorphine (BUP) and an elevated cut-off concentration of 30ng/mL IMM MCG IMM 5ng/mL 49 13 norbuprenorphine (nor-BUP) for excretion in rather than 5ng/mL has been suggested (1). + Sensitivity 100% 79% urine. 1 37 Specificity 97% 97% Immunoassays which do not detect • MCG screening cut-off set to 20ng/mL as - norbuprenorphine are subject to higher false proposed by a reference laboratory rather LC-MS/MS 5 ng/mL Accuracy 99% 86% negative rates since not all specimens from than 30ng/mL as suggested in the literature, buprenorphine users contain the parent drug. in an attempt to minimize both false + - When compliance testing is the main goal of an application, a high false negative rate due negatives due to non-detection of nor-BUP; IMM 5ng/mL + 62 1 Objectives and false positives due to cross-reactivity to the inability to detect the metabolite norbuprenorphine is a drawback. In 515 with opiates and other glucuronides 0 37 •To evaluate the analytical performance of - specimens taken from daily users of BUP the two commercially available urine • IMM screening cut-off set to the IMM positive rates for BUP, Nor-BUP, BUP-gluc buprenorphine immunoassays: Immunalysis 14 specimens were discrepant using the MCG and Nor-BUP gluc were 1.2%, 63.9%, 89.9% recommendation of 5ng/mL (since no opioid assay. -

WO 2012/109445 Al 16 August 2012 (16.08.2012) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2012/109445 Al 16 August 2012 (16.08.2012) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/485 (2006.01) A61P 25/04 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, (21) International Application Number: CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, PCT/US20 12/024482 DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, (22) International Filing Date: HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, ' February 2012 (09.02.2012) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SC, SD, (26) Publication Language: English SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 13/024,298 9 February 201 1 (09.02.201 1) US (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant (for all designated States except US): QRX- GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, PHARMA LTD. -

Drug Plasma Half-Life and Urine Detection Window | January 2019
500 Chipeta Way | Salt Lake City, UT 84108-1221 Phone: (800) 522-2787 | Fax: (801) 583-2712 www.aruplab.com | www.arupconsult.com DRUG PLASMA HALF-LIFE AND URINE DETECTION WINDOW | JANUARY 2019 URINE- PLASMA DRUG, DRUG METABOLITE(S)* COMMON TRADE AND STREET NAMES, NOTES DETECTION HALF-LIFEt WINDOWt STIMULANTS Benzedrine, dexedrine, Adderall, Vyvanse, speed; could be methamphetamine Amphetamine 7–34 hours 1–5 days metabolite; if so, typically < 30 percent of parent Cocaine Coke, crack; parent drug rarely observed due to short half-life 0.7–1.5 hours < 1 day Benzoylecgonine Cocaine metabolite 5.5–7.5 hours 1–2 days Desoxyn, methedrine, Vicks inhaler (D- and L-isomers not resolved; low concentrations Methamphetamine expected if the source is Vicks); selegeline (Atapryl, Carbex, Eldepryl, Zelapar) 6–17 hours 1–5 days metabolite Methylenedioxyamphetamine (MDA) MDA 11–17 hours 1–3 days Methylenedioxyethylamphetamine (MDEA) MDEA, MDE, Eve 6–11 hours 1–3 days Methylenedioxymethamphetamine (MDMA) MDMA, XTC, ecstasy, Molly 6–10 hours 1–3 days Methylphenidate Ritalin, Concerta, Focalin, Metadate, Methylin 1.4–4.2 hours < 1 day Ritalinic acid Methylphenidate metabolite 1.8–2.5 hours < 1 day Phentermine Adipex-P, Lomaira, Qsymia 19–24 hours 1–5 days OPIOIDS Buprenorphine Belbuca, Buprenex, Butrans, Suboxone, Subutex, Sublocade, Zubsolv 26–42 hours 1–7 days Norbuprenorphine, Glucuronides Buprenorphine metabolites 15–150 hours 1–14 days Included in many preparations; morphine metabolite; may be a contaminant if < 2 Codeine 1.9–3.9 hours 1–3 days percent of morphine Fentanyl Actiq, Duragesic, Fentora, Lazanda, Sublimaze, Subsys, Ionsys 3–12 hours 1–3 days Norfentanyl Fentanyl metabolite 9–10 hours 1–3 days Heroin Diacetylmorphine, dope, smack, dust; parent drug not detected. -
Prediction of Drug Interactions with Methadone, Buprenorphine and Oxycodone from in Vitro Inhibition of Metabolism
The author(s) shown below used Federal funds provided by the U.S. Department of Justice and prepared the following final report: Document Title: Prediction of Drug Interactions with Methadone, Buprenorphine and Oxycodone from In Vitro Inhibition of Metabolism Author(s): David E. Moody, Ph.D. Document No.: 250127 Date Received: July 2016 Award Number: 2011-DN-BX-K532 This report has not been published by the U.S. Department of Justice. To provide better customer service, NCJRS has made this federally funded grant report available electronically. Opinions or points of view expressed are those of the author(s) and do not necessarily reflect the official position or policies of the U.S. Department of Justice. February 2016 Research and Development in Forensic Toxicology Prediction of drug interactions with methadone, buprenorphine and oxycodone from in vitro inhibition of metabolism Final Technical Report Submitted electronically to: U.S. Department of Justice Office of Justice Programs National Institute of Justice Prepared by: David E. Moody. Ph.D. Director of the Center for Human Toxicology, and Research Professor of Pharmacology and Toxicology [email protected] / 801-581-5117 NIJ Award Number: 2011-DN-BX-K532 Reporting Period: January 1, 2012 to December 31, 2015 Recipient Organization: University of Utah 75 South 2000 East, Room 222 Salt Lake City, UT 84112-8930 Organizational DUNS: 0090953650000 EIN: 876000525 This document is a research report submitted to the U.S. Department of Justice. This report has not been published by the Department. Opinions or points of view expressed are those of the author(s) and do not necessarily reflect the official position or policies of the U.S. -

(12) Patent Application Publication (10) Pub. No.: US 2014/0144429 A1 Wensley Et Al
US 2014O144429A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2014/0144429 A1 Wensley et al. (43) Pub. Date: May 29, 2014 (54) METHODS AND DEVICES FOR COMPOUND (60) Provisional application No. 61/887,045, filed on Oct. DELIVERY 4, 2013, provisional application No. 61/831,992, filed on Jun. 6, 2013, provisional application No. 61/794, (71) Applicant: E-NICOTINE TECHNOLOGY, INC., 601, filed on Mar. 15, 2013, provisional application Draper, UT (US) No. 61/730,738, filed on Nov. 28, 2012. (72) Inventors: Martin Wensley, Los Gatos, CA (US); Publication Classification Michael Hufford, Chapel Hill, NC (US); Jeffrey Williams, Draper, UT (51) Int. Cl. (US); Peter Lloyd, Walnut Creek, CA A6M II/04 (2006.01) (US) (52) U.S. Cl. CPC ................................... A6M II/04 (2013.O1 (73) Assignee: E-NICOTINE TECHNOLOGY, INC., ( ) Draper, UT (US) USPC ..................................................... 128/200.14 (21) Appl. No.: 14/168,338 (57) ABSTRACT 1-1. Provided herein are methods, devices, systems, and computer (22) Filed: Jan. 30, 2014 readable medium for delivering one or more compounds to a O O Subject. Also described herein are methods, devices, systems, Related U.S. Application Data and computer readable medium for transitioning a Smoker to (63) Continuation of application No. PCT/US 13/72426, an electronic nicotine delivery device and for Smoking or filed on Nov. 27, 2013. nicotine cessation. Patent Application Publication May 29, 2014 Sheet 1 of 26 US 2014/O144429 A1 FIG. 2A 204 -1 2O6 Patent Application Publication May 29, 2014 Sheet 2 of 26 US 2014/O144429 A1 Area liquid is vaporized Electrical Connection Agent O s 2. -
Report Format 6000 Laboratory Report P.O
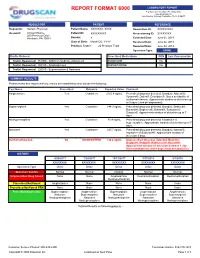
REPORT FORMAT 6000 LABORATORY REPORT P.O. Box 347, Horsham, PA 19044-0347 www.drugscan.com Lab Director: Anthony Costantino, Ph.D., F-ABFT REQUESTOR PATIENT REFERENCE Requestor: Sample Physician Patient Name: XXXXXXX, XXXX Requisition ID: XXXXXXXXX Account: Account Name Patient ID: XXXXXXXXX Accessioning ID: XXXXXXXX 200 Precision Drive Horsham, PA 19044 Gender: X Collected Date: June 01, 2018 Date of Birth: Month DD, YYYY Received Date: June 02, 2018 Previous Tests*: 24 Previous Tests Reported Date: June 04, 2018 Specimen Type: URINE Profile Ordered Prescribed Medications PRN Last Consumption Test(s) Requested: 651000 - Addiction Medicine Adolescent SUBOXONE No Test(s) Requested: 602100 - Amphetamines AMPHETAMINE No Test(s) Requested: 620010 - Buprenorphine & Naloxone SUMMARY RESULTS Please review this report carefully; results are noted below and include the following: Test Name Prescribed Outcome Reported Value Comment Amphetamine Yes Consistent 2303.8 ng/mL 3UHVFULEHGGUXJZDVGHWHFWHG%UDQG V $GGHUDOO 9\YDQVH'LGUH['H[HGULQH$OVRDPHWDEROLWHRI methamphetamine. Approximate window of detection up to 9 days (urine pH dependent). Buprenorphine Yes Consistent 144.3 ng/mL 3UHVFULEHGGUXJZDVGHWHFWHG%UDQG V %HOEXFD %XQDYDLO%XSUHQH[%XWUDQV6XER[RQH 6XEXWH[$SSUR[LPDWHZLQGRZRIGHWHFWLRQXSWR days. Norbuprenorphine Yes Consistent 88.4 ng/mL Prescribed drug was detected. Metabolite of buprenorphine. Approximate window of detection up to 7 days. Naloxone Yes Consistent 325.7 ng/mL 3UHVFULEHGGUXJZDVGHWHFWHG%UDQG V 1DUFDQ ,QJUHGLHQWRI6XER[RQH$SSUR[LPDWHZLQGRZRI -

Review Memorandum
510(k) SUBSTANTIAL EQUIVALENCE DETERMINATION DECISION SUMMARY ASSAY ONLY TEMPLATE A. 510(k) Number: k060527 B. Purpose for Submission: Clearance of a new device. C. Measurand: Buprenorphine and Norbuprenorphine D. Type of Test: Qualitative, visually read, immunochromatographic test E. Applicant: Alfa Scientific Designs, Inc. F. Proprietary and Established Names: Instant-View, Instant-Confirmatory, or Instant-Confirmatory Buprenorphine/Norbuprenorphine Urine Test (Cassette and Dip-Strip) G. Regulatory Information: 1. Regulation section: 21 CFR §862.3650, Opiate Test System 2. Classification: Class II 3. Product code: DJG 4. Panel: Toxicology (91) H. Intended Use: 1. Intended use(s): This device is a qualitative immunoassay intended to detect buprenorphine (BUP) and its metabolite, norbuprenorphine (NBUP) in human urine. Results are preliminary positive when the combination of the concentrations of BUP and NBUP is greater than 10 ng/ml. It is for health care professional use only. This test provides only a preliminary result. A more specific alternate chemical method must be used in order to obtain a confirmed analytical result. Gas Chromatography / Mass Spectrometry (GC/MS) or High Performance Liquid Chromatography (HPLC) is the preferred confirmatory method. Clinical consideration and professional judgment should be applied to any drug of abuse test result, particularly when preliminary positive results are obtained. 1 2. Indication(s) for use: See Intended Use above. 3. Special conditions for use statement(s): A positive test result does not always mean an individual has taken the drug illegally as the drug can be administered legally. 4. Special instrument requirements: Not applicable. The device is a visually read single-use device. -

Forensics Market
FORENSICS MARKET A FORENSIC TOXICOLOGY METHOD FOR THE DETERMINATION OF DESOMORPHINE, HEROIN, METHADONE, BUPRENORPHINE AND METABOLITES IN URINE USING LC/MS QQQ Desomorphine, also known by its street name Krokodil, is an emerging synthetic opioid, used as a heroin substitute and produced by back street illicit laboratories. Author Peter JW Stone Agilent Technologies Inc., 5301 Stevens Creek Blvd, Santa Clara, CA, 95051, USA. ABSTRACT The analytical measurement of opioid panels commonly 6-Monoacetylmorphine-D6 Heroin-D9 include a number of compounds such as heroin, methadone Buprenorphine-D4 Methadone-D9 and buprenorphine. Research methods with sufficient flexibility are of value to respond to the need to measure Desomorphine-D3 Norbuprenorphine-D3 new compounds resulting from clandestine production. EDDP-D3 INTRODUCTION Table 1 – Internal Standards Utilized Desomorphine, also known by its street name Krokodil, is HPLC Method Parameters (Agilent 1290 system): an emerging synthetic opioid, used as a heroin substitute Agilent Poroshell 120 EC and produced by back street illicit laboratories. Little or Column: C18, 2.1 x 50mm (2.7μm) no literature exists presently describing an analytical approach to determining desomorphine in samples. Column temperature: 55°C Injection volume: 1 uL This application brief describes the development of an LC/MS QQQ research method that aims to rapidly Autosampler temp: 4°C screen for to and measure desomorphine together with Needle wash: flushport (100% metha- heroin, buprenorphine, methadone and their metabolites nol), 5 sec 6-acetylmorphine, norbuprenorphine and EDDP. A = 5mM NH4for- Mobile phase: mate/0.01% formic acid A three minute analytical research method has been in water developed with results obtained for five batches of spiked B = 0.01% formic acid in urine samples over the linear concentration range of methanol 1-5000ng/ml.