Drug Interactions and Lethal Drug Combinations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Definition of Controlled Substance Schedules
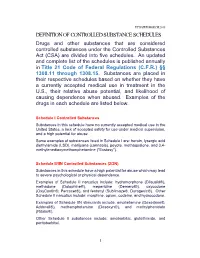
UPDATED MARCH 2018 DEFINITION OF CONTROLLED SUBSTANCE SCHEDULES Drugs and other substances that are considered controlled substances under the Controlled Substances Act (CSA) are divided into five schedules. An updated and complete list of the schedules is published annually in Title 21 Code of Federal Regulations (C.F.R.) §§ 1308.11 through 1308.15. Substances are placed in their respective schedules based on whether they have a currently accepted medical use in treatment in the U.S., their relative abuse potential, and likelihood of causing dependence when abused. Examples of the drugs in each schedule are listed below. Schedule I Controlled Substances Substances in this schedule have no currently accepted medical use in the United States, a lack of accepted safety for use under medical supervision, and a high potential for abuse. Some examples of substances listed in Schedule I are: heroin, lysergic acid diethylamide (LSD), marijuana (cannabis), peyote, methaqualone, and 3,4- methylenedioxymethamphetamine ("Ecstasy"). Schedule II/IIN Controlled Substances (2/2N) Substances in this schedule have a high potential for abuse which may lead to severe psychological or physical dependence. Examples of Schedule II narcotics include: hydromorphone (Dilaudid®), methadone (Dolophine®), meperidine (Demerol®), oxycodone (OxyContin®, Percocet®), and fentanyl (Sublimaze®, Duragesic®). Other Schedule II narcotics include: morphine, opium, codeine, and hydrocodone. Examples of Schedule IIN stimulants include: amphetamine (Dexedrine®, Adderall®), methamphetamine (Desoxyn®), and methylphenidate (Ritalin®). Other Schedule II substances include: amobarbital, glutethimide, and pentobarbital. 1 Schedule III/IIIN Controlled Substances (3/3N) Substances in this schedule have a potential for abuse less than substances in Schedules I or II and abuse may lead to moderate or low physical dependence or high psychological dependence. -

Comparison of Short-And Long-Acting Benzodiazepine-Receptor Agonists
J Pharmacol Sci 107, 277 – 284 (2008)3 Journal of Pharmacological Sciences ©2008 The Japanese Pharmacological Society Full Paper Comparison of Short- and Long-Acting Benzodiazepine-Receptor Agonists With Different Receptor Selectivity on Motor Coordination and Muscle Relaxation Following Thiopental-Induced Anesthesia in Mice Mamoru Tanaka1, Katsuya Suemaru1,2,*, Shinichi Watanabe1, Ranji Cui2, Bingjin Li2, and Hiroaki Araki1,2 1Division of Pharmacy, Ehime University Hospital, Shitsukawa, Toon, Ehime 791-0295, Japan 2Department of Clinical Pharmacology and Pharmacy, Neuroscience, Ehime University Graduate School of Medicine, Shitsukawa, Toon, Ehime 791-0295, Japan Received November 7, 2007; Accepted May 15, 2008 Abstract. In this study, we compared the effects of Type I benzodiazepine receptor–selective agonists (zolpidem, quazepam) and Type I/II non-selective agonists (zopiclone, triazolam, nitrazepam) with either an ultra-short action (zolpidem, zopiclone, triazolam) or long action (quazepam, nitrazepam) on motor coordination (rota-rod test) and muscle relaxation (traction test) following the recovery from thiopental-induced anesthesia (20 mg/kg) in ddY mice. Zolpidem (3 mg/kg), zopiclone (6 mg/kg), and triazolam (0.3 mg/kg) similarly caused an approximately 2-fold prolongation of the thiopental-induced anesthesia. Nitrazepam (1 mg/kg) and quazepam (3 mg/kg) showed a 6- or 10-fold prolongation of the anesthesia, respectively. Zolpidem and zopiclone had no effect on the rota-rod and traction test. Moreover, zolpidem did not affect motor coordination and caused no muscle relaxation following the recovery from the thiopental-induced anesthesia. However, zopiclone significantly impaired the motor coordination at the beginning of the recovery. Triazolam significantly impaired the motor coordination and muscle relaxant activity by itself, and these impairments were markedly exacerbated after the recovery from anesthesia. -

Red with Nitrazepam and Placebo in Acute Emergency Driving Situations and in Monotonous Simulated Driving
109 A 1986 The Carry-over Effects of Triazolam Compa- red with Nitrazepam and Placebo in Acute Emergency Driving Situations and in Mono- tonous Simulated Driving Hans Laurell and Jan Törnroos Reprint from Acta Pharmacologica et toxicologica 1986 v Väg06/7 Efi/( Statens väg- och trafikinstitut (VTI) * 581 01 Linköping [St]tlltet Swedish Road and Traffic Research Institute * S-581 01 Linköping Sweden Acta pharmacol. et toxicol. 1986, 58, 182186. From the National Swedish Road and Traffic Research Institute, (V.T.I.), S-58 101 Linköping, Sweden The Carry-over Effects of Triazolam Compared with Nitrazepam and Placebo in Acute Emergency Driving Situations and in Monotonous Simulated Driving Hans Laurell and Jan Törnros (Received October 9, 1985; Accepted January 9, 1986) Abstract: Eighteen healthy volunteers of both sexes, aged 2034, were tested in the morning while undertaking real car driving avoidance manoeuvres and during monotonous simulated driving after 1 and 3 nights of medication with triazolam 0.25 mg, nitrazepam 5 mg or placebo. The study was a double-blind, randomized, cross-over study, where a minimum of 7 days wash-out separated the 3 treatment periods. Nitrazepam was found to impair performance in the simulated task after 1 but not after 3 nights of medication. Performance in the triazolam condition was not signicantly different from the other conditions on this task on either day. However, after one night of medication triazolam tended to score worse than placebo but better than nitrazepam. In real car driving a tendency was noted for nitrazepam to score worst, whereas the difference between placebo and triazolam was hardly noticeable. -

Calculating Equivalent Doses of Oral Benzodiazepines
Calculating equivalent doses of oral benzodiazepines Background Benzodiazepines are the most commonly used anxiolytics and hypnotics (1). There are major differences in potency between different benzodiazepines and this difference in potency is important when switching from one benzodiazepine to another (2). Benzodiazepines also differ markedly in the speed in which they are metabolised and eliminated. With repeated daily dosing accumulation occurs and high concentrations can build up in the body (mainly in fatty tissues) (2). The degree of sedation that they induce also varies, making it difficult to determine exact equivalents (3). Answer Advice on benzodiazepine conversion NB: Before using Table 1, read the notes below and the Limitations statement at the end of this document. Switching benzodiazepines may be advantageous for a variety of reasons, e.g. to a drug with a different half-life pre-discontinuation (4) or in the event of non-availability of a specific benzodiazepine. With relatively short-acting benzodiazepines such as alprazolam and lorazepam, it is not possible to achieve a smooth decline in blood and tissue concentrations during benzodiazepine withdrawal. These drugs are eliminated fairly rapidly with the result that concentrations fluctuate with peaks and troughs between each dose. It is necessary to take the tablets several times a day and many people experience a "mini-withdrawal", sometimes a craving, between each dose. For people withdrawing from these potent, short-acting drugs it has been advised that they switch to an equivalent dose of a benzodiazepine with a long half life such as diazepam (5). Diazepam is available as 2mg tablets which can be halved to give 1mg doses. -

Drug-Facilitated Sexual Assault Panel, Blood
DRUG-FACILITATED SEXUAL ASSAULT PANEL, BLOOD Blood Specimens (Order Code 70500) Alcohols Analgesics, cont. Anticonvulsants, cont. Antihistamines, cont. Ethanol Phenylbutazone Phenytoin Cyclizine Amphetamines Piroxicam Pregabalin Diphenhydramine Amphetamine Salicylic Acid* Primidone Doxylamine BDB Sulindac* Topiramate Fexofenadine Benzphetamine Tapentadol Zonisamide Guaifenesin Ephedrine Tizanidine Antidepressants Hydroxyzine MDA Tolmetin Amitriptyline Loratadine MDMA Tramadol Amoxapine Oxymetazoline* Mescaline* Anesthetics Bupropion Pyrilamine Methcathinone Benzocaine Citalopram Tetrahydrozoline Methamphetamine Bupivacaine Clomipramine Triprolidine Phentermine Etomidate Desipramine Antipsychotics PMA Ketamine Desmethylclomipramine 9-hydroxyrisperidone Phenylpropanolamine Lidocaine Dosulepin Aripiprazole Pseudoephedrine Mepivacaine Doxepin Buspirone Analgesics Methoxetamine Duloxetine Chlorpromazine Acetaminophen Midazolam Fluoxetine Clozapine Baclofen Norketamine Fluvoxamine Fluphenazine Buprenorphine Pramoxine* Imipramine Haloperidol Carisoprodol Procaine 1,3-chlorophenylpiperazine (mCPP) Mesoridazine Cyclobenzaprine Rocuronium Mianserin* Norclozapine Diclofenac Ropivacaine Mirtazapine Olanzapine Etodolac Antibiotics Nefazodone Perphenazine Fenoprofen Azithromycin* Nordoxepin Pimozide Hydroxychloroquine Chloramphenicol* Norfluoxetine Prochlorperazine Ibuprofen Ciprofloxacin* Norsertraline Quetiapine Ketoprofen Clindamycin* Nortriptyline Risperidone Ketorolac Erythromycin* Norvenlafaxine Thioridazine Meclofenamic Acid* Levofloxacin* Paroxetine -

Treatment of Myoclonus with Pheneturide
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.41.7.598 on 1 July 1978. Downloaded from Journal ofNeurology, Neurosurgery, andPsychiatry, 1978, 41, 598-602 Treatment of myoclonus with pheneturide C. D. WARD From the Royal Hospital, Sheffield S U M M A R Y Twenty-one patients with various forms of myoclonus are presented. Phena- cemide was given to five patients with considerable benefit to three, but with serious toxic effects in two. Another acetylurea derivative, pheneturide, was given to 19 patients and was well tolerated. Myoclonus was completely or substantially controlled in 12 patients. The term "myoclonus" may be applied to very between 1965 and 1976. They had displayed myo- abrupt involuntary movements which are neur- clonic jerks and had been treated with phena- onally determined, asynergic, and arrhythmic. An cemide or pheneturide. Of these patients, 16 were assortment of involuntary movements share these seen personally for review and three responded to characteristics but differ in their relationship to a questionnaire. Records of outpatient follow-up movement, relaxation, posture, or sensory stimuli, were available for one patient who had died and Protected by copyright. and in their anatomical disposition (Gasaut, 1968); for one who could not be traced. All had given a they may involve parts of muscles, whole muscles, history of repeated, instantaneous involuntary or, more usually, muscle groups. Such movements, movements and had reported at least one of the collectively termed myoclonus, are seen in a wide following: sudden jerks of the arms causing ob- variety of pathological conditions (Halliday, 1967) jects to fly out of the hands; sudden interruption and may often be associated with epilepsy. -

Intermittent Treatment of Febrile Convulsions with Nitrazepam Michel Vanasse, Pierre Masson, Guy Geoffroy, Albert Larbrisseau and Pierre C
LE JOURNAL CANADIEN DES SCIENCES NEUROLOGIQUES Intermittent Treatment of Febrile Convulsions with Nitrazepam Michel Vanasse, Pierre Masson, Guy Geoffroy, Albert Larbrisseau and Pierre C. David ABSTRACT: Intermittent oral or rectal administration of diazepam for the prophylactic treatment of febriie convulsions has given results comparable to the continuous use of phenobarbital while limiting side effects and risks of toxicity. Since we believe that nitrazepam is a better anticonvulsant than diazepam, we performed a study to evaluate the effectiveness of this medication in the prophylactic treatment of febrile convulsions. Nitrazepam was given only when the children had fever and almost exclusively in children with a high risk of recurrence (less than 12 months of age at first convulsion; atypical convulsion; one or several previous convulsions). Thirty one children with a high risk of recurrence received nitrazepam. The rate of recurrence in this group was 19.3% after a follow-up of 16 months, compared to 45.8% in 24 children who also had a high risk of recurrence but in whom the parents refused the medication or gave it inadequately (p<0.05). Fifty one children with a low risk of recurrence also were evaluated and followed for at least 12 months (mean 15.4 months). Six were treated with nitrazepam, mostly because of parental anxiety, and none had a recurrence; of the 45 untreated children in this group, 6 (13.6%) had another convulsion. These results show the efficiency of nitrazepam in the prophylactic treatment of febrile convulsions. RESUME: L'utilisation intermittente du diazepam par voie orale ou rectale pour le traitement prophylactique des convulsions febriles a donne d'aussi bons resultats que l'utilisation continue du phenobarbital. -

FINAL STUDY PROTOCOL Utilisation of Antiepileptic Medicines in Girls
FINAL STUDY PROTOCOL Utilisation of antiepileptic medicines in girls and women of childbearing potential - a study in three European countries Prepared for the European Medicines Agency May 2017 Version 2.0 Approved 15th May 2017 EUROmediSAFE Consortium 1 TABLE OF CONTENTS Page 1. Background 3 2. Aims 4 3. Data sources 5 4. Methods 6 5. Statistical analyses 12 6. Sample size 15 7. Strengths and limitations 15 8. Study report and manuscript 17 9. Communication of study results 17 10. Ethical and data access approvals 17 11. Milestones 18 12. Quality control 18 13. Data access, storage and sharing 18 14. Protocol authors 20 15. Amendments and deviations from the protocol 20 Appendix I 21 2 1. BACKGROUND In October 2013, the Medicines and Healthcare Regulatory Authority issued a referral into the use of sodium valproate in girls and women of childbearing potential, following new evidence in the literature relating to an increased risk of neurodevelopmental disorders in children exposed to sodium valproate in-utero. The review was carried out by the Pharmacovigilance Risk Assessment Committee (PRAC) and in October 2014 the PRAC adopted its recommendation. Following completion of the review, a letter was sent to healthcare professionals in January 2015 informing them of the changes in the recommendations for valproate prescribing. The recommendations resulting from the review included that Valproate and related substances should not be used in female children, women of childbearing potential and pregnant women unless alternative treatments are ineffective or not tolerated. Valproate and related substances should be contraindicated in prophylaxis of migraine attacks in pregnancy and women of childbearing potential who are not using effective methods of contraception during treatment with valproate. -

Commonly Abused Prescription and Otc Medications
C OMMONLY A BUSED P RESCRIPTION AND OTC MEDIcaTIONS Substance Examples of Commercial and Street Names DEPRESSANTS barbiturates Amytal, Nembutal, Seconal, Phenobarbital; barbs, reds, red birds, phennies, tooies, yellows, yellow jackets Benzodiazepines Ativan, Halcion, Librium, Valium, Xanax; candy, downers, sleeping (other than flunitrazepam) pills, tranks Flunitrazepam Rohypnol; forget-me pill, Mexican Valium, R2, Roche, roofies, (associated with sexual assaults; roofinol, rope, rophies not sold in US, but may be brought in) OPIOIDS AND MORPHINE DERIVATIVES codeine Empirin with Codeine, Fiorinal with Codeine, Robitussin A-C, Tylenol with Codeine; Captain Cody, Cody, schoolboy; (with glutethimide) doors & fours, loads, pancakes and syrup fentanyl and fentanyl analogs Actiq (oral), Duragesic (patch), Sublimaze; Apache, China girl, China white, dance fever, goodfella, jackpot, murder 8, TNT, Tango & Cash morphine Roxanol, Duramorph; M, Miss Emma, monkey, white stuff oxycodone HCL Oxycontin; Oxy, O.C., killer hydrocodone bitartrate, acetaminophen Vicodin; vike, Watson-387 STIMULANTS amphetamine Biphetamine, Dexedrine, Adderall; bennies, black beauties, crosses, hearts, LA turnaround, speed, truck drivers, uppers methylphenidate Ritalin; JIF, MPH, R-ball, Skippy, the smart drug, vitamin R (safe & effective for treatment of ADHD) OVER-THE-COUNTER (OTC) MEDICATION Dextromethorphan (DXM) Found in any cold medicine with “DM” or “Tuss” in the title or name; Orange Crush, Triple C’s, C-C-C, Red Devils, Skittles, Dex, Vitamin D, Robo, Robo-trippin’, -

Chloral Hydrate: Summary Report
Chloral Hydrate: Summary Report Item Type Report Authors Yuen, Melissa V.; Gianturco, Stephanie L.; Pavlech, Laura L.; Storm, Kathena D.; Yoon, SeJeong; Mattingly, Ashlee N. Publication Date 2020-02 Keywords Compounding; Food, Drug, and Cosmetic Act, Section 503B; Food and Drug Administration; Outsourcing facility; Drug compounding; Legislation, Drug; United States Food and Drug Administration; Chloral Hydrate Rights Attribution-NoDerivatives 4.0 International Download date 26/09/2021 09:06:16 Item License http://creativecommons.org/licenses/by-nd/4.0/ Link to Item http://hdl.handle.net/10713/12087 Summary Report Chloral Hydrate Prepared for: Food and Drug Administration Clinical use of bulk drug substances nominated for inclusion on the 503B Bulks List Grant number: 2U01FD005946 Prepared by: University of Maryland Center of Excellence in Regulatory Science and Innovation (M-CERSI) University of Maryland School of Pharmacy February 2020 This report was supported by the Food and Drug Administration (FDA) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award (U01FD005946) totaling $2,342,364, with 100 percent funded by the FDA/HHS. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement by, the FDA/HHS or the U.S. Government. 1 Table of Contents REVIEW OF NOMINATION ..................................................................................................... 4 METHODOLOGY ................................................................................................................... -

The Risk of Specific Congenital Anomalies in Relation to Newer Antiepileptic Drugs
Drugs - Real World Outcomes (2016) 3:131–143 DOI 10.1007/s40801-016-0078-1 REVIEW ARTICLE The Risk of Specific Congenital Anomalies in Relation to Newer Antiepileptic Drugs: A Literature Review 1 2 1 Josta de Jong • Ester Garne • Lolkje T. W. de Jong-van den Berg • Hao Wang1 Published online: 24 May 2016 Ó The Author(s) 2016. This article is published with open access at Springerlink.com Abstract found. The signals for associations between topiramate and Background More information is needed about possible cleft lip with/without cleft palate and hypospadias were associations between the newer anti-epileptic drugs considered strong. Associations between lamotrigine and (AEDs) in the first trimester of pregnancy and specific anencephaly and transposition of great vessels were found congenital anomalies of the fetus. within one study and were not supported by other studies. Objectives We performed a literature review to find sig- No signals were found for the other newer AEDs, or the nals for potential associations between newer AEDs information was too limited to provide such a signal. (lamotrigine, topiramate, levetiracetam, gabapentin, Conclusion In terms of associations between monotherapy oxcarbazepine, eslicarbazepine, felbamate, lacosamide, with a newer AED in the first trimester of pregnancy and a pregabalin, retigabine, rufinamide, stiripentol, tiagabine, specific congenital anomaly, the signals for topiramate and vigabatrin, and zonisamide) and specific congenital cleft lip with/without cleft palate and hypospadias should anomalies. be investigated further. Methods We searched PubMed and EMBASE to find observational studies with pregnancies exposed to newer AEDs and detailed information on congenital anomalies. Key Points The congenital anomalies in the studies were classified according to the congenital anomaly subgroups of Euro- Information was found on specific congenital pean Surveillance of Congenital Anomalies (EUROCAT). -

Antiepileptic Drugs: Evolution of Our Knowledge and Changes in Drug Trials
ILAE 110th anniversary review paper* Epileptic Disord 2019; 21 (4): 319-29 Antiepileptic drugs: evolution of our knowledge and changes in drug trials Emilio Perucca Past President of the International League Against Epilepsy Division of Clinical and Experimental Pharmacology, Department of Internal Medicine and Therapeutics, University of Pavia, Pavia and IRCCS Mondino Foundation, Pavia, Italy Received April 30, 2019; Accepted June 01, 2019 ABSTRACT – Clinical trials provide the evidence needed for rational use of medicines. The evolution of drug trials follows largely the evolution of regulatory requirements. This article summarizes methodological changes in antiepileptic drug trials and associated advances in knowledge starting from 1938, the year phenytoin was introduced and also the year when evi- dence of safety was made a requirement for the marketing of medicines in the United States. The first period (1938-1969) saw the introduction of over 20 new drugs for epilepsy, many of which did not withstand the test of time. Only few well controlled trials were completed in that period and trial designs were generally suboptimal due to methodological constraints. The intermediate period (1970-1988) did not see the introduction of any major new medication, but important therapeutic advances took place due to improved understanding of the properties of available drugs. The value of therapeutic drug monitoring and monotherapy were recognized dur- ing the intermediate period, which also saw major improvements in trial methodology. The last period (1989-2019) was dominated by the introduc- tion of second-generation drugs, and further evolution in the design of monotherapy and adjunctive-therapy trials. The expansion of the pharma- cological armamentarium has improved opportunities for tailoring drug treatment to the characteristics of the individual.