Evolution of the Clinical Microbiology Laboratory
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Journal of Microbiology, Immunology and Infection
JOURNAL OF MICROBIOLOGY, IMMUNOLOGY AND INFECTION AUTHOR INFORMATION PACK TABLE OF CONTENTS XXX . • Description p.1 • Impact Factor p.1 • Abstracting and Indexing p.2 • Editorial Board p.2 • Guide for Authors p.4 ISSN: 1684-1182 DESCRIPTION . Journal of Microbiology, Immunology and Infection, launched in 1968, is the official bi-monthly publication of the Taiwan Society of Microbiology, the Chinese Society of Immunology, the Infectious Diseases Society of Taiwan and the Taiwan Society of Parasitology. The journal is an open access journal, committed to disseminating information on the latest trends and advances in microbiology, immunology, infectious diseases and parasitology. Articles on clinical or laboratory investigations of relevance to microbiology, immunology, infectious diseases, parasitology and other related fields that are of interest to the medical profession are eligible for consideration. Article types considered include perspectives, review articles, original articles, brief reports and correspondence. The Editorial Board of the Journal comprises a dedicated team of local and international experts in the field of microbiology, immunology, infectious diseases and parasitology. All members of the Editorial Board actively guide and set the direction of the journal. With the aim of promoting effective and accurate scientific information, an expert panel of referees constitutes the backbone of the peer- review process in evaluating the quality and content of manuscripts submitted for publication. JMII is open access and indexed in SCIE, PubMed, MEDLINE, EMBASE, Scopus, AIDS & Cancer Reseach, CABI, BIOSIS Previews, Biological Abstracts, EBSCOhost, CancerLit, Reactions Weekly (online), Chemical Abstracts, HealthSTAR, Global Health, ProQuest. Benefits to authors We also provide many author benefits, such as free PDFs, a liberal copyright policy, special discounts on Elsevier publications and much more. -

Biofilms and Biodiversity: an Interactive Exploration of Aquatic
Journal of Industrial Microbiology & Biotechnology (2000) 24, 334–338 2000 Society for Industrial Microbiology 1367-5435/00 $15.00 www.nature.com/jim Biofilms and biodiversity: an interactive exploration of aquatic microbial biotechnology and ecology JA Frederick1, D Jacobs2 and WR Jones3 1Maryland Sea Grant Extension Program, Columbus Center, 701 E Pratt St, Baltimore, MD 21202; 2Maryland Sea Grant, 0112 Skinner Hall, College Park, MD 20742; 3Center of Marine Biotechnology, University of Maryland Biotechnology Institute, 701 E Pratt St, Baltimore, MD 21202, USA The study of biofilms provides a unique educational opportunity to examine ecosystems, biodiversity and appli- cations of environmental biotechnology. There are many variables that could be studied for measuring the interac- tions between bacterial biofilms and invertebrate biodiversity as a method for assessing the health of aquatic eco- systems. These interactions also lend themselves to an easily replicated model system which can be used to reach a wide audience with an educational opportunity for students as well as a professional development opportunity for teachers. At the foundation of the research are invaluable basic microbiology skills: strain collection, isolation, cultivation and characterization. Through the additional process of characterizing, identifying and enumerating invertebrate organisms that attach to bacterial biofilms in aquatic ecosystems, there evolved a multidisciplinary class laboratory activity that has found broad application. This activity is captivating not only to undergraduate microbiology students but to middle and high school students and their teachers. The demand for information about the activity has led to the development of a truly interactive web-based lesson, which in turn has resulted in additional inquiries and further refinement of the lesson as an undergraduate independent research course. -

Get App Journal Flyer
IMPACT Indexed in: FACTOR PubMed 4.128 an Open Access Journal by MDPI The Hellenic Society Mikrobiokosmos (MBK) and Spanish Society for Nitrogen Fixation (SEFIN) are affiliated with Microorganisms IMPACT Indexed in: FACTOR PubMed 4.128 an Open Access Journal by MDPI Editor-in-Chief Message from the Editor-in-Chief Prof. Dr. Martin von Bergen “Microorganism” merges the idea of the very small with the idea of the evolving reproducing organism is a unifying principle for the discipline of microbiology. Our journal recognizes the broadly diverse yet connected nature of microorganisms and provides an advanced publishing forum for original articles from scientists involved in high-quality basic and applied research on any prokaryotic or eukaryotic microorganism, and for research on the ecology, genomics and evolution of microbial communities as well as that exploring cultured microorganisms in the laboratory. Author Benefits Open Access Unlimited and free access for readers No Copyright Constraints Retain copyright of your work and free use of your article Impact Factor 4.128 (2020 Journal Citation Reports®) Thorough and Rapid Peer-Review Coverage by Leading Indexing Services Science Citation Index Expanded - Web of Science (Clarivate Analytics), BIOSIS Previews (Clarivate Analytics), PubMed (NLM), Scopus (Elsevier) No Space Constraints, No Extra Space or Color Charges No restriction on the length of the papers, number of figures or colors Major Forum for Readers Interested in Diverse Aspects of Microorganisms Discounts on Article Processing Charges (APC) If you belong to an institute that participates with the MDPI Institutional Open Access Program (IOAP) Aims and Scope Microorganisms publishes original research, reviews, short communications, and commentaries. -

Microbiology and Immunology 1
Microbiology and Immunology 1 Microbiology and Programs Immunology Undergraduate Programs of Study Chair Major • Li Wu • Major in Microbiology (Bachelor of Science) Director, Undergraduate Studies Minor • Richard J. Roller • Minor in Microbiology Director, Graduate Studies • Timothy L. Yahr Graduate Programs of Study Undergraduate major: microbiology (B.S.) Majors Undergraduate minor: microbiology • Master of Science in Microbiology Graduate degrees: M.S. in microbiology; Ph.D. in microbiology • Doctor of Philosophy in Microbiology Faculty: https://medicine.uiowa.edu/microbiology/people/ primary-appointments Facilities Website: https://medicine.uiowa.edu/microbiology/ The Department of Microbiology and Immunology is Study in the Department of Microbiology and Immunology situated on the University of Iowa health sciences campus, is dedicated to the branch of biological sciences that where it shares the Bowen Science Building with the investigates the smallest living things: microbes that include Departments of Anatomy and Cell Biology, Biochemistry bacteria, archaea, fungi, algae, protozoa, and viruses. It and Molecular Biology, Molecular Physiology and Biophysics, is coupled with immunology that includes the study of the and Neuroscience and Pharmacology. Laboratory space and protective responses of higher organisms to disease-causing modern equipment are available for teaching and research. microbes and cancers, and mistakes in immune function. Microbiology and immunology often interact in humans at the microbiome, those microbes that live with humans on their Courses skin and mucosal surfaces, and yet must be restricted from causing diseases by the immune system. Microbiology and Immunology Microbiology and immunology are at the forefront of the Courses modern biological revolution. Microbes are experimental subjects of choice for examining genetic and biological MICR:2157 General Microbiology 3 s.h. -

Top Peer Reviewed Journals – Microbiology
Top Peer Reviewed Journals – Microbiology Presented to Iowa State University Presented by Thomson Reuters Microbiology The subject discipline for Microbiology is made of 5 narrow subject categories from the Web of Science. The 5 categories that make up Microbiology are: 1. Microbiology 4. Parasitology 2. Microscopy 5. Virology 3. Mycology The chart below provides an ordered view of the top peer reviewed journals within the 1st quartile for Microbiology based on Impact Factors (IF), three year averages and their quartile ranking. Journal 2009 IF 2010 IF 2011 IF Average IF NATURE REVIEWS MICROBIOLOGY 17.64 20.68 21.18 19.83 CLINICAL MICROBIOLOGY REVIEWS 14.69 13.5 16.12 14.77 Cell Host & Microbe 13.02 13.72 13.5 13.41 ANNUAL REVIEW OF MICROBIOLOGY 12.8 12.41 14.34 13.18 MICROBIOLOGY AND MOLECULAR 12.58 12.22 13.01 12.60 BIOLOGY REVIEWS FEMS MICROBIOLOGY REVIEWS 9.78 11.79 10.96 10.84 PLoS Pathogens 8.97 9.07 9.12 9.05 ADVANCES IN MICROBIAL PHYSIOLOGY 5.75 8.55 9.87 8.06 CURRENT OPINION IN MICROBIOLOGY 7.86 7.71 7.92 7.83 TRENDS IN MICROBIOLOGY 6.89 7.5 7.91 7.43 REVIEWS IN MEDICAL VIROLOGY 7.44 5.6 7.2 6.75 ISME Journal 6.39 6.15 7.37 6.64 CRITICAL REVIEWS IN MICROBIOLOGY 5.34 6.27 5.81 CELLULAR MICROBIOLOGY 5.72 5.62 5.45 5.60 Advances in Parasitology 6.23 4.39 5.31 mBio 5.31 5.31 Retrovirology 4.1 5.23 6.47 5.27 JOURNAL OF VIROLOGY 5.15 5.18 5.4 5.24 MOLECULAR MICROBIOLOGY 5.36 4.81 5.01 5.06 TRENDS IN PARASITOLOGY 4.29 4.9 5.14 4.78 ADVANCES IN VIRUS RESEARCH 5.52 4.83 3.97 4.77 ANTIMICROBIAL AGENTS AND 4.8 4.67 4.84 4.77 CHEMOTHERAPY -
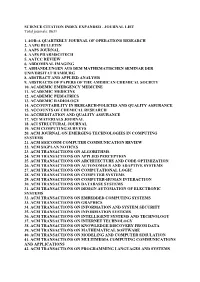
SCIENCE CITATION INDEX EXPANDED - JOURNAL LIST Total Journals: 8631
SCIENCE CITATION INDEX EXPANDED - JOURNAL LIST Total journals: 8631 1. 4OR-A QUARTERLY JOURNAL OF OPERATIONS RESEARCH 2. AAPG BULLETIN 3. AAPS JOURNAL 4. AAPS PHARMSCITECH 5. AATCC REVIEW 6. ABDOMINAL IMAGING 7. ABHANDLUNGEN AUS DEM MATHEMATISCHEN SEMINAR DER UNIVERSITAT HAMBURG 8. ABSTRACT AND APPLIED ANALYSIS 9. ABSTRACTS OF PAPERS OF THE AMERICAN CHEMICAL SOCIETY 10. ACADEMIC EMERGENCY MEDICINE 11. ACADEMIC MEDICINE 12. ACADEMIC PEDIATRICS 13. ACADEMIC RADIOLOGY 14. ACCOUNTABILITY IN RESEARCH-POLICIES AND QUALITY ASSURANCE 15. ACCOUNTS OF CHEMICAL RESEARCH 16. ACCREDITATION AND QUALITY ASSURANCE 17. ACI MATERIALS JOURNAL 18. ACI STRUCTURAL JOURNAL 19. ACM COMPUTING SURVEYS 20. ACM JOURNAL ON EMERGING TECHNOLOGIES IN COMPUTING SYSTEMS 21. ACM SIGCOMM COMPUTER COMMUNICATION REVIEW 22. ACM SIGPLAN NOTICES 23. ACM TRANSACTIONS ON ALGORITHMS 24. ACM TRANSACTIONS ON APPLIED PERCEPTION 25. ACM TRANSACTIONS ON ARCHITECTURE AND CODE OPTIMIZATION 26. ACM TRANSACTIONS ON AUTONOMOUS AND ADAPTIVE SYSTEMS 27. ACM TRANSACTIONS ON COMPUTATIONAL LOGIC 28. ACM TRANSACTIONS ON COMPUTER SYSTEMS 29. ACM TRANSACTIONS ON COMPUTER-HUMAN INTERACTION 30. ACM TRANSACTIONS ON DATABASE SYSTEMS 31. ACM TRANSACTIONS ON DESIGN AUTOMATION OF ELECTRONIC SYSTEMS 32. ACM TRANSACTIONS ON EMBEDDED COMPUTING SYSTEMS 33. ACM TRANSACTIONS ON GRAPHICS 34. ACM TRANSACTIONS ON INFORMATION AND SYSTEM SECURITY 35. ACM TRANSACTIONS ON INFORMATION SYSTEMS 36. ACM TRANSACTIONS ON INTELLIGENT SYSTEMS AND TECHNOLOGY 37. ACM TRANSACTIONS ON INTERNET TECHNOLOGY 38. ACM TRANSACTIONS ON KNOWLEDGE DISCOVERY FROM DATA 39. ACM TRANSACTIONS ON MATHEMATICAL SOFTWARE 40. ACM TRANSACTIONS ON MODELING AND COMPUTER SIMULATION 41. ACM TRANSACTIONS ON MULTIMEDIA COMPUTING COMMUNICATIONS AND APPLICATIONS 42. ACM TRANSACTIONS ON PROGRAMMING LANGUAGES AND SYSTEMS 43. ACM TRANSACTIONS ON RECONFIGURABLE TECHNOLOGY AND SYSTEMS 44. -

History of the Department of Microbiology 1868 – 2009
June 2015 HISTORY OF THE DEPARTMENT OF MICROBIOLOGY 1868 – 2009 University of Illinois at Urbana-Champaign 1 A HISTORY OF THE DEPARTMENT OF MICROBIOLOGY 1868 – 2009 This 141 year history of the Department of Microbiology includes an article (Chapter 1), written and published in 1959 by the Department, which covers the period 1868 to 1959. I joined the Department in 1953, and my recounting of the Department’s history includes personal observations as well as anecdotes told to me by H. O. Halvorson and others. Later I realized what a unique experience it had been to join a first-class department, and I resolved to play a role in maintaining its research stature. Ralph Wolfe 2 Department of Microbiology History of the Headship: 1950 – 1959 Halvor Halvorson 1960 – 1963 Kim Atwood 1963 – 1972 Leon Campbell 1972 – 1982 Ralph DeMoss 1982 – 1987 Samuel Kaplan 1987 – 1990 Jordan Konisky 1990 – 1991 Ralph Wolfe (Acting Head) 1991 – 1997 Charles Miller 1997 – 2002 John Cronan 2003 – 2004 Jeffrey Gardner (Acting Head) 2005 – Present John Cronan 3 Organization of the History of the Department In Chapters 2 to 6 the data are divided into Academic Decades, each containing the following sections: Section I, an overview of the decade; Section II, some events for each year of the decade; Section III, a summary of the research interests, honors received, publications, and invited off-campus lectures or seminars for each faculty member. These data have been obtained from the annual reports of the faculty submitted to the departmental secretary. 4 CHAPTER 1 1868 – 1959 During this time period the name of the Department was Department of Bacteriology (Anecdotes by Ralph Wolfe) A SHORT HISTORY OF THE DEPARTMENT OF BACTERIOLOGY H. -

The Twilight Zones of Microbiology John Postgate
The twilight zones of microbiology John Postgate Professor John In 1674, Antoni Leeuwenhoek first described happy with that? Nor am I. But the probabilities are that Postgate, FRS, ●to the Royal Society his microscopic animal- we shall have to come to terms with it, just as mid- author of the well cules, creatures so small as to be invisible to the twentieth-century microbiologists had eventually to known book naked eye. His findings were received with lively accept that, contrary to the orthodoxy of the time, Microbes and Man, interest, but they made no radical impact, because bacteria possessed chromosomes. creatures close to the limits of optical resolution were So, are prions alive? That may seem a silly question, Honorary Member already known, and his protozoa were on the margin of because it has long been obvious that linguistically the and former President that limit. It was his letter of October, 1676, which borders of animate and inanimate matter are fuzzy, and of the Society, astonished the Society, for the ‘tiny eels’ he saw, which we that around those borders the term ‘living’ becomes looks at why the now call bacteria, were vastly smaller than even those imprecise. Yet fuzzy terminology leads to fuzzy ‘twilight zones of earlier creatures. The subsequent story is now history. thinking; we cannot wait for a precise definition of life, microbiology’ should Suddenly, size-range of living things had been extended so we need an operational consensus on how elementary not be ignored. downwards by two orders of magnitude of length. It was a biological entity can be and still be regarded as alive. -

Chapter 1—The Science of Microbiology
Chapter 1—The Science of Microbiology MULTIPLE CHOICE 1. Lister used phenol to a. disprove the theory of spontaneous generation. b. prevent the infection in wounds. c. sterilize surgical instruments. d. stimulate bacterial growth. ANS: B OBJ: TYPE: Knowledge 2. The bacterium that causes the bubonic plague is a. Bacillus subtilis. b. Escherichia coli. c. Pseudomonas aeruginosa. d. Yersinia pestis. ANS: D OBJ: TYPE: Knowledge 3. The Irish potato famine was caused by a a. bacterium. b. fungus. c. protozoan. d. virus. ANS: B OBJ: TYPE: Knowledge 4. Select the characteristic that all microorganisms have in common. a. They are bacteria. b. They are organisms used in biological research. c. They are pathogens. d. They are too small to be seen with the unaided eye. ANS: D OBJ: TYPE: Knowledge 5. A microbe is used to produce erythropoietin, a hormone that signals the production of red blood cells in the bone marrow of the human body. The production of this hormone is an advance mainly from the field of _____________ microbiology. a. agricultural b. environmental c. industrial d. pathogenic ANS: C OBJ: TYPE: Comprehension 6. Select the incorrect association. a. algae/eukaryotes b. archaea/prokaryotes c. bacteria/prokaryotes d. protozoa/not microscopic ANS: D OBJ: TYPE: Comprehension 7. Select the incorrect statement about a virus. a. It contains DNA or RNA. b. It has a protein coat. c. It is a cellular organism. d. It is visible through the electron microscope. ANS: C OBJ: TYPE: Comprehension 8. Select the correct statement about bacteria. a. Most are multicellular. b. None exhibit motility. -

Cell Biology, Immunology & Microbiology
Cell Biology, Immunology & Microbiology Student Handbook 2019-2020 The information provided in this document serves to supplement the requirements of the Graduate School of Biomedical Sciences detailed in the UNTHSC Catalog with requirements specific to the discipline of Cell Biology, Immunology & Microbiology. CBIM Discipline Handbook (6/3/19) 1 Table of Contents Page Description of the Cell Biology, Immunology & Microbiology Discipline .............................................................. 3 Graduate Faculty and Their Research .............................................. 4 Requirements ................................................................................. 13 Required Courses ...................................................................... 13 Journal Club and Seminar Courses ........................................... 13 Works in Progress ..................................................................... 13 Elective Courses ....................................................................... 13 Sample Degree Plans ..................................................................... 15 Advancement to Candidacy ........................................................... 18 CBIM Discipline Handbook (6/3/19) 2 Cell Biology, Immunology & Microbiology Discipline Rance E. Berg, PhD, Graduate Advisor Research and Education Building – RES-202N 817-735-2121 [email protected] Graduate Faculty: Allen; Berg; Borejdo; Clark; Fudala; I. Gryczynski; Z. Gryczynski; He; Hodge; Jones; Krishnamoorthy; P. Mathew; S. -

AUTHOR GUIDELINES Molecular Microbiology Updated June 2020
AUTHOR GUIDELINES Molecular Microbiology updated June 2020 Sections 1. Aims and Scope 2. Submission Process 3. Article Types 4. Peer Review Process 5. After Acceptance 1. Aims and Scope Molecular Microbiology publishes studies of Bacteria, Archaea, eukaryotic microorganisms, and their viruses. Research papers should lead to a deeper understanding of the molecular principles underlying basic physiological processes or mechanisms. Appropriate topics include gene expression and regulation, pathogenicity and virulence, physiology and metabolism, synthesis of macromolecules (proteins, nucleic acids, lipids, polysaccharides, etc.), cell and structural biology, subcellular organization, membrane biogenesis and function, traffic and transport, cell-cell communication and signaling pathways, evolution and gene transfer. Articles focused on host responses (cellular or immunological) to pathogens or on microbial ecology should be directed to our sister journals Cellular Microbiology and Environmental Microbiology, respectively. Molecular Microbiology editorial team has experience in all areas of research covered by the journal. Authors should generally choose the Editor whose interests are closest to their own (see below) but may select another editor if they wish. Editors will reassign papers if they consider that there is a conflict of interest, that another Editor would be more appropriate, or that the chosen Editor cannot handle the manuscript in a timely fashion, in which case the authors will be informed. If in doubt, authors should submit -

Microbiology and Molecular Genetics 1
Microbiology and Molecular Genetics 1 For certification and completion of the BS degree, students will take MICROBIOLOGY AND one year of clinical internship in program accredited by the National Accrediting Agency for Clinical Laboratory Science (NAACLS) and MOLECULAR GENETICS affiliated with Oklahoma State University. Students have the options of the following hospitals/programs: Comanche County Memorial Hospital, Microbiology/Cell and Molecular Biology Lawton, OK; St. Francis Hospital, Tulsa, OK; Mercy Hospital, Ada, OK; Mercy Hospital, Ardmore, OK. Microbiology is the hands-on study of bacteria, viruses, fungi and algae and their many relationships to humans, animals, plants and the Medical Laboratory Science is unique in allowing students to enter environment. Cell and molecular biology bridges the fields of chemistry, the health profession directly after obtaining a BS degree. Clinical biochemistry and biology as it seeks to understand life and cellular laboratory scientists comprise the third-largest segment of the healthcare processes at the molecular level. Microbiologists apply their knowledge professions and are an important member of the healthcare team, to infectious diseases and pathogenic mechanisms; food production working alongside doctors and nurses. Students who complete and preservation, industrial fermentations which produce chemicals, Microbiology/Cell and Molecular Biology with the MLS option enjoy a drugs, antibiotics, alcoholic beverages and various food products; 100% employment rate upon graduation. biodegradation of toxic chemicals and other materials present in the environment; insect pathology; the exciting and expanding field of Courses biotechnology which endeavors to utilize living organisms to solve GENE 5102 Molecular Genetics important problems in medicine, agriculture, and environmental science; Prerequisites: BIOC 3653 or MICR 3033 and one course in genetics or infectious diseases; and public health and sanitation.