Failure of Labetalol to Prevent Hypertension Due to Clonidine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

TRANDATE® (Labetalol Hydrochloride) Tablets
NDA 18716/S-026 Page 2 PRODUCT INFORMATION TRANDATE® (labetalol hydrochloride) Tablets DESCRIPTION: Trandate Tablets are adrenergic receptor blocking agents that have both selective alpha1-adrenergic and nonselective beta-adrenergic receptor blocking actions in a single substance. Labetalol hydrochloride (HCl) is a racemate chemically designated as 2-hydroxy-5-[1-hydroxy-2-[(1 methyl-3-phenylpropyl)amino]ethyl]benzamide monohydrochloride, and it has the following structure: Labetalol HCl has the empirical formula C19H24N2O3•HCl and a molecular weight of 364.9. It has two asymmetric centers and therefore exists as a molecular complex of two diastereoisomeric pairs. Dilevalol, the R,R′ stereoisomer, makes up 25% of racemic labetalol. Labetalol HCl is a white or off-white crystalline powder, soluble in water. Trandate Tablets contain 100, 200, or 300 mg of labetalol HCl and are taken orally. The tablets also contain the inactive ingredients corn starch, FD&C Yellow No. 6 (100- and 300-mg tablets only), hydroxypropyl methylcellulose, lactose, magnesium stearate, pregelatinized corn starch, sodium benzoate (200-mg tablet only), talc (100-mg tablet only), and titanium dioxide. CLINICAL PHARMACOLOGY: Labetalol HCl combines both selective, competitive, alpha1-adrenergic blocking and nonselective, competitive, beta-adrenergic blocking activity in a single substance. In man, the ratios of alpha- to beta-blockade have been estimated to be approximately 1:3 and 1:7 following oral and intravenous (IV) administration, respectively. Beta2-agonist activity has been demonstrated in animals with minimal beta1-agonist (ISA) activity detected. In animals, at doses greater than those required for alpha- or beta-adrenergic blockade, a membrane stabilizing effect has been demonstrated. -

Pain Management Opioid Safety a Quick Reference Guide (2014)
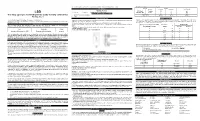
Pain Management Opioid Safety A Quick Reference Guide (2014) VA Academic Detailing Service Real Provider Resources Real Patient Results Your Partner in Enhancing Veteran Health Outcomes VA Academic Detailing Service Email Group: [email protected] VA Academic Detailing Service SharePoint Site: https://vaww.portal2.va.gov/sites/ad Opioids: A Practical Guide for Clinicians Example Risk Assessment Tool: Opioid Risk Tool (ORT)1 Item Score if Female Item Score if Male Alcohol 1 3 1. Family history of substance abuse Illegal drugs 2 3 Prescription drugs 4 4 Alcohol 3 3 2. Personal history of substance abuse Illegal drugs 4 4 Prescription drugs 5 5 3. Age (mark box if 16–45) 1 1 4. History of preadolescent sexual abuse 3 0 Attention deficit disorder obsessive compulsive disorder 2 2 5. Psychological disease Bipolar Schizophrenia Depression 1 1 Total Risk Category: 0–3 Low Risk of aberrant behaviors; 4–7 Moderate Risk of aberrant behaviors; ≥8 High Risk of aberrant behaviors Assess risk of aberrant behaviors before initiating opioid medications; the ORT or other rating tools can assist with this process but can overestimate risk thus should not be used as only reason to decline opioid prescription. 1 Opioids Risk Classification10-11 Risk Condition/Situation • Diagnosis with concordant physical exam, medical imaging, laboratory findings • High levels of pain acceptance and active coping strategies Low • Well motivated patient willing to participate in multimodal treatment plan (no moderate to high risk • Attempting to function -
New Zealand Data Sheet 1. Product Name
NEW ZEALAND DATA SHEET 1. PRODUCT NAME Norvir 100 mg tablets. 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each film-coated tablet contains 100 mg ritonavir. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM White film-coated oval tablets debossed with the corporate Abbott "A" logo and the Abbott-Code “NK”. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications NORVIR is indicated for use in combination with appropriate antiretroviral agents or as monotherapy if combination therapy is inappropriate, for the treatment of HIV-1 infection in adults and children aged 12 years and older. For persons with advanced HIV disease, the indication for ritonavir is based on the results for one study that showed a reduction in both mortality and AIDS defining clinical events for patients who received ritonavir. Median duration of follow-up in this study was 6 months. The clinical benefit from ritonavir for longer periods of treatment is unknown. For persons with less advanced disease, the indication is based on changes in surrogate markers in controlled trials of up to 16 weeks duration (see section 5.1 Pharmacodynamic properties). 4.2 Dose and method of administration General Dosing Guidelines Prescribers should consult the full product information and clinical study information of protease inhibitors if they are co-administered with a reduced dose of ritonavir. The recommended dose of NORVIR is 600 mg (six tablets) twice daily by mouth, and should be given with food. NORVIR tablets should be swallowed whole and not chewed, broken or crushed. NORVIR DS 29 April 2020 Page 1 of 37 Version 35 Paediatric population Ritonavir has not been studied in patients below the age of 12 years; hence the safety and efficacy of ritonavir in children below the age of 12 have not been established. -

Adrenoceptors Regulating Cholinergic Activity in the Guinea-Pig Ileum 1978) G.M
- + ! ,' Br. J. Pharmac. (1978), 64, 293-300. F'(O t.,," e reab- ,ellular PHARMACOLOGICAL CHARACTERIZATION OF THE PRESYNAPTIC _-ADRENOCEPTORS REGULATING CHOLINERGIC ACTIVITY IN THE GUINEA-PIG ILEUM 1978) G.M. Departmentof Pharmacology,Allen and HzmburysResearchLimited, Ware, Hertfordshire,SG12 ODJ I The presynaptic ct-adrenoceptors located on the terminals of the cholinergic nerves of the guinea- pig myenteric plexus have been characterized according to their sensitivities to at-adrenoceptor agonists and antagonists. 2 Electrical stimulation of the cholinergic nerves supplying the longitudinal muscle of the guinea-pig ! ileum caused a twitch response. Clonidine caused a concentration-dependent inhibition of the twitch i response; the maximum inhibition obtained was 80 to 95_o of the twitch response. Oxymetazoline and xylazine were qualitatively similar to clonidine but were about 5 times less potent. Phenylephrine and methoxamine also inhibited the twitch response but were at least 10,000 times less potent than clonidine. 3 The twitch-inhibitory effects of clonidine, oxymetazoline and xylazine, but not those of phenyl- ephrine or methoxamine, were reversed by piperoxan (0.3 to 1.0 lag/ml). 4 Lysergic acid diethylamide (LSD) inhibited the twitch response, but also increased the basal tone of the ileum. Mepyramine prevented the increase in tone but did not affect the inhibitory action of LSD. Piperoxan or phentolamine only partially antagonized the inhibitory effect of LSD. 5 Phentolamine, yohimbine, piperoxan and tolazoline were potent, competitive antagonists of the inhibitory effect of clonidine with pA2 values of 8.51, 7.78, 7.64 and 6.57 respectively. 6 Thymoxamine was a weak antagonist of clonidine; it also antagonized the twitch-inhibitory effect of morphine. -

Urine Drug Testing – Ordering and Interpretation The
URINE DRUG TESTING – ORDERING AND INTERPRETATION Created by: Dr. Daniel Berland, M.D. THE TESTS Enzyme linked immunoassay (EIA) kits • Screening test for illicit substances amphetamine/methamphetamine, (marijuana, PCP, cocaine, “opiates” (morphine/codeine) • Inexpensive, fast, point of care or lab • Detects class of substance, not specific medication • Will be negative for hydrocodone, hydromorphone, oxycodone, methadone, buprenorphine, benzodiazepines (particularly clonazepam) unless specific test kit for those meds is in use. Ask your lab! • High false positive rates caused by numerous prescribed or OTC meds Gas chromatography/Mass Spectroscopy (GCMS) • More expensive, labor intensive • Confirming test identifies specific meds and their metabolites. Use to confirm patient is taking prescribed meds and not taking non-prescribed meds • High sensitivity, but you must tell the lab what you seek (patient is taking) • False positives still occur ** Human Urine: T ~98 deg; > 90 deg for 15 min. pH 4.5-8; SG 1.002-1.03. Ur Cr > 20 mg/dL ** WHAT TO ORDER • Test for illicit drug use: EIA • Test to confirm taking prescribed meds: GCMS (EIA is OK if your lab runs the test for each med – they usually do not – ask!) • Test to check for use of non-prescribed medication: GCMS POSSIBLE OUTCOMES OF TESTING • Presence of illicit substance: Use by patient; false result related to prescribed or OTC med exposure • Presence of non-prescribed medication: Illicit use by patient; false positive testing – cross-reaction or possible known metabolite (e.g., morphine -

Management of Postnatal Hypertension - Top Tips
Management of postnatal hypertension - top tips FOLLOW UP PLAN Follow up Hypertensive disorder Chronic Gestational Pre - Severe pre- hypertension hypertension eclampsia eclampsia/ Mild/ HELLP/ Moderate Eclampsia Initial follow up Community midwife and general practitioner BP frequency At least once 3- At least once Every 1-2 days for 2 wks 5 days post 3-5 days post as above birth then as birth clinically Then as indicated clinically indicated Acceptable BP Aim BP should be <150/100 mmHg. BP <140/90 If not on antihypertensives commence if BP≥ 150/100 Suitable Labetalol, nifedipine, enalapril, atenolol, antihypertensives AVOID DIURETICS STOP METHYLDOPA WITHIN 2 DAYS OF DELIVERY When to reduce/ NA If BP<130/80 If BP<130/80 reduce stop If not seen reduce antihypertensive before needs If BP < 140/ If BP <140/ 90 consider GP review at 90 consider reducing 2wks post birth reducing Convert back to If not seen prepregnancy before needs antihypertensive GP review at as indicated 2wks post birth 6 weeks GP/ pre GP GP Hospital cons follow up pregnancy care clinic team POSTNATAL REVIEW AT POSTNATAL REVIEW 6-8 weeks after birth Offer medical review Offer specialist assessment if antihypertensives still needed Rpt Plt, transaminases, creatinine if indicated Carry out urine dipstick test If proteinuria still ≥ 1+ offer further review at 3 months to assess kidney function – consider offering renal referral. Give advice re: recurrence risks – see table below: Advise women to maintain BMI 18.5-24.9 kg/m2 H.Yeeles/S. Rutter July 14 Management of postnatal -
(LSD) Test Dip Card (Urine) • Specimen Collection Container % Agreement 98.8% 99
frozen and stored below -20°C. Frozen specimens should be thawed and mixed before testing. GC/MS. The following results were tabulated: Method GC/MS MATERIALS Total Results Results Positive Negative Materials Provided LSD Rapid Positive 79 1 80 LSD • Test device • Desiccants • Package insert • Urine cups Test Dip card Negative 1 99 100 Materials Required But Not Provided Total Results 80 100 180 One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) • Specimen collection container % Agreement 98.8% 99. % 98.9% • Timer Package Insert DIRECTIONS FOR USE Analytical Sensitivity This Instruction Sheet is for testing of Lysergic acid diethylamide. Allow the test device, and urine specimen to come to room temperature [15-30°C (59-86°F)] prior to testing. A drug-free urine pool was spiked with LSD at the following concentrations: 0 ng/mL, -50%cutoff, -25%cutoff, cutoff, A rapid, one step test for the qualitative detection of Lysergic acid diethylamide and its metabolites in human urine. 1) Remove the test device from the foil pouch. +25%cutoff and +50%cutoff. The result demonstrates >99% accuracy at 50% above and 50% below the cut-off For forensic use only. 2) Remove the cap from the test device. Label the device with patient or control identifications. concentration. The data are summarized below: INTENDED USE 3) Immerse the absorbent tip into the urine sample for 10-15 seconds. Urine sample should not touch the plastic Lysergic acid diethylamide (LSD) Percent of Visual Result The One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) is a lateral flow chromatographic device. -

Study of Methyl Dopa Versus Labetalol in Management of Preeclampsia and Gestational Hypertension
logy & Ob o st ec e tr n i y c s G Dharwadkar et al., Gynecol Obstet (Sunnyvale) 2014, 4:9 Gynecology & Obstetrics DOI; 10.4172/2161-0932.1000242 ISSN: 2161-0932 Research Article Open Access Study of Methyl Dopa Versus Labetalol in Management of Preeclampsia and Gestational Hypertension Dharwadkar MN1, Kanakamma MK1, Dharwadkar SN2*, Rajagopal K1, Gopakumar C3, Divya James Fenn J4 and Balachandar V3,5 1Department of Obstetrics and Gynaecology, Yenepoya Medical College and teaching Hospital, Yenepoya University, Deralakatte, Mangalore, Karnataka 575022, India 2Department of Zoology, K.L.E’s. S. Nijalingappa College, KLE Medical University (Health), Bangalore, Karnataka 560010, India 3Department of Human Genetics Molecular Biology, Bharathiar University, Coimbatore, India 4Post Graduate Student, Department of Obstetrics and Gynaecology, Sree Balaji Medical College and Hospital, Chennai 600044, Tamil Nadu, India 5Human Molecular Genetics Laboratory, Department of Zoology, Bharathiar University, Coimbatore, India Abstract Objective: To assess the efficacy and safety of labetalol compared with methyldopa in the management of mild and moderate cases of pregnancy-induced hypertension (PIH). Methods: Eighty patients with PIH were randomly allocated to receive either labetalol (group A) or methyldopa (group B). Administration of drugs with respect to Age, Gravid Status, Blood Pressure, Urine albumin Levels, Side Effects, Drug dosage, Additional Treatment, Prolongation of Pregnancy, New born Screening Test (NST), mode of termination, Indication of caesarean section, Perinatal safety and APGAR scores were studied. The statistical level of significance was taken at P<0.05. Results: A labetalol has been very effective in control as well as earlier onset of action in patients with methyl dopa. -

One Step Multi-Drug Screen Test Cup Package Insert
Fentanyl (FEN) Fentanyl 300 the treatment of seizure disorders and alcohol withdrawal. Risk of physical dependence increases if One Step Multi-Drug Screen Test Cup Benzodiazepines are taken regularly (e.g., daily) for more than a few months, especially at higher Fentanyl (FEN) Fentanyl 200 than normal doses. Stopping abruptly can bring on such symptoms as trouble sleeping, Package Insert Fentanyl (FEN) Fentanyl 100 gastrointestinal upset, feeling unwell, loss of appetite, sweating, trembling, weakness, anxiety and changes in perception. Only trace amounts (less than 1%) of most Benzodiazepines are excreted Cotinine (COT) Cotinine 200 Package insert for testing of any combination of the following drugs: Methamphetamine, unaltered in the urine; most of the concentration in urine is conjugated drug. The detection period Amphetamine, Cocaine, Morphine, Ecstasy, EDDP (Methadone Metabolites), Tricyclic 6-Monoacetylmorphine (6-MAM) 6-Monoacetylmorphine 10 for the Benzodiazepines in the urine is 3-7 days. Antidepressants, Oxycodone, Barbiturates, Buprenorphine, Phencyclidine, K2 (Synthetic Methaqualone (MQL) Methaqualone 300 Cannabinoid), Ketamine, Methaqualone, Methadone, Fentanyl, Tramadol, Ethyl Glucuronide, OXYCODONE (OXY) Cotinine, 6-Monoacetylmorphine, Methylenedioxypyrovalerone, Lysergic acid diethylamide, Ketamine (KET) Ketamine 1,000 Oxycodone, [4,5-epoxy-14-hydroxy-3-methoxy-17-methyl-morphinan-6-one, Marijuana and Benzodiazepines. Ketamine (KET) Ketamine 100 dihydrohydroxycodeinone] is a semi-synthetic opioid agonist derived from thebaine, -

Hypertensive Urgency (Asymptomatic Severe Hypertension): Considerations for Management
www.RxFiles.ca ‐ updated June 2016 RxFiles Q&A Summary K Krahn , L Regier UofS BSP Student 2014 BSP, BA HYPERTENSIVE URGENCY (ASYMPTOMATIC SEVERE HYPERTENSION): CONSIDERATIONS FOR MANAGEMENT Hypertension is one of the most common chronic medical conditions in Canada. More than one in five Canadians has hypertension and the lifetime risk of developing hypertension is 90%.1 With the addition of comorbid conditions and other risk factors, hypertensive cases can quickly become even more complex. Hypertensive crises include hypertensive urgencies & emergencies. Optimal management lacks conclusive evidence. The rate of associated major adverse cardiovascular events in asymptomatic patients seen in the office are very low.13 Since rapid treatment of hypertensive urgency is not required, some prefer to call it asymptomatic severe hypertension. 1,2,3 ,4,5,6,7,8,9 WHAT IS HYPERTENSIVE URGENCY & HOW DOES IT COMPARE TO HYPERTENSIVE EMERGENCY? The term hypertensive crises can be further divided into hypertensive urgency and hypertensive emergency. The distinction between these two conditions is outlined below.8 Differentiating between these scenarios is essential before initiating treatment. URGENCY 2‐9 EMERGENCY 2‐9 Blood Pressure (mmHg) >180 systolic &/or >120 ‐ >130 CHEP diastolic No Yes: currently experiencing (e.g. aortic dissection, angina/ACS, stroke, Target Organ Damage* encephalopathy, acute renal failure, pulmonary edema, eclampsia) Asymptomatic; or severe headache, shortness Shortness of breath, chest pain, numbness/weakness, change in Symptoms of breath, nosebleeds, severe anxiety vision, back pain, difficulty speaking *Note: Signs of end‐organ damage/dysfunction may occur at a lower blood pressure in pregnant & pediatric patients Initial Patient Work‐Up to Differentiate between Urgency and Emergency: Verify blood pressure (BP) reading(s). -

Comparison of Methyldopa and Labetalol in Control of Blood
International Journal of Clinical Obstetrics and Gynaecology 2019; 3(5): 372-379 ISSN (P): 2522-6614 ISSN (E): 2522-6622 © Gynaecology Journal Comparison of methyldopa and labetalol in control of www.gynaecologyjournal.com 2019; 3(5): 372-379 blood pressure in preeclampsia Received: 16-07-2019 Accepted: 20-08-2019 Dr. Suryarao Prashant Dwarkanath and Dr. Katakdhond Shriraj Shanmukh Dr. Suryarao Prashant Dwarkanath Assistant Professor, Obstetrics & DOI: https://doi.org/10.33545/gynae.2019.v3.i5f.378 Gynaecology Department, Dr D Y Patil Medical College, Pimpri, Pune, Maharashtra, India Abstract Background: Preeclampsia is a leading cause of maternal and perinatal morbidity and mortality in Dr. Katakdhond Shriraj Shanmukh developing world. Assistant Professor, Obstetrics & Materials and Methods: 188 eligible patients were randomly assigned to receive treatment with either Gynaecology Department, Dr. D Y labetalol or methyldopa. Patil Medical College, Pimpri, Observation and Results: Proteinuria was drop down to 8.51 % after treatment with labetalol. There were Pune, Maharashtra, India 14 cases of IUGR in methyldopa group as compared to 4 cases in labetalol group. Patients with labetalol group delivered at term were 82.97 % whereas in methyldopa group 76.59%. There was no significant difference in Apgar score between two groups. Need of nicu in labetalol group was 6% as compared to 7% in methyldopa group. Drowsiness was the most common side effect observed in methyldopa group while very few cases of adverse effects in labetalol group. Conclusion: Our study suggests that labetalol is better than methyldopa in treatment of hypertension in pregnancy and has good perinatal and maternal outcome. Keywords: Preeclampsia, labetalol, methyldopa, maternal and perinatal outcome Introduction The hypertensive disorders of pregnancy are common medical complications of gestation and continue to be responsible for the high maternal and perinatal mortality and morbidity [1]. -

Adult Intravenous Medications
Revised 9/08 ADULT INTRAVENOUS MEDICATIONS STANDARD AND MAXIMUM ALLOWABLE CONCENTRATIONS, GUIDELINES FOR CONTINUOUS OR TITRATED INFUSIONS MEDICATION STANDARD MAXIMUM CONC./ DOSING MONITORING/COMMENTS ADMIXTURE INFUSION INSTRUCTIONS Adenosine 6 mg/2 mL vial Give undiluted directly into 6 mg initially. If SVT not ECG, heart rate, blood pressure (Adenocard®) (3 mg/mL) given undiluted vein over 1-2 seconds. resolved in 1-2 minutes, may Administer as proximal as follow with 12 mg dose. If Extremely short half life: possible to trunk (i.e., not in not resolved in 1-2 minutes, < 10 seconds Slows conduction time through the AV node, interrupting the re-entry lower arm, hand, lower leg, may follow with an Not effective for converting A. pathways through the AV node, or foot). If administered additional 12 mg dose. flutter, A. fib, or ventricular restoring normal sinus rhythm. through IV line, administer tachycardia. as close to pts heart as Contraindicated if symptomatic Onset of action: immediate Duration: seconds possible. NS flush must be bradycardia, sick sinus given rapidly, immediately syndrome, 2nd or 3rd degree AV following injection of block (unless pt. has functioning adenosine pacemaker) Amiodarone Load: Dilute 150 mg (3mL) in Peripheral line: Up to 2 Load: 150 mg/100 mL over Telemetry monitoring, BP (Cordarone®) 100 mL D5W (1.5 mg/mL) mg/mL 10 minutes. (hypotension occurs frequently (PVC bag suitable for loading (Not to eXceed 30 mg/mL) with initial rates), HR Antiarrhythmic agent that dose) (Concentrations over 2 (arrhythmias: AV block, depresses conduction velocity, mg/mL administered for THEN bradycardia, VT/VF, torsades de slows AV node conduction, raises Maintenance infusion: longer than 1 hour must be pointes), electrolytes the threshold for VF, and eXhibits Dilute 900 mg (18 mL) in infused via central line) Infusion: 1 mg/min for 6 some α and β blockade activity.