Guinea Ebola Response Plan II: End of Project Report June 02, 2015–May 31, 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Guinea Ebola Response Plan II: End of Project Report June 02, 2015–May 30, 2016
Guinea Ebola Response Plan II: End of Project Report June 02, 2015–May 30, 2016 Submitted to: United States Agency for International Development under Cooperative Agreement #AID-OAA-A-14-00028 Submitted by: Jhpiego Corporation in cooperation with Save the Children The Maternal and Child Survival Program (MCSP) is a global United States Agency for International Development (USAID) Cooperative Agreement to introduce and support high-impact health interventions with a focus on 24 high-priority countries with the ultimate goal of ending preventable child and maternal deaths within a generation. The Program is focused on ensuring that all women, newborns and children most in need have equitable access to quality health care services to save lives. MCSP supports programming in maternal, newborn and child health, immunization, family planning and reproductive health, nutrition, health systems strengthening, water/sanitation/hygiene, malaria, prevention of mother-to-child transmission of HIV, and pediatric HIV care and treatment. Visit www.mcsprogram.org to learn more. This report is made possible by the generous support of the American people through USAID under the terms of the Cooperative Agreement AID-OAA-A-14-00028. The contents are the responsibility of MCSP and do not necessarily reflect the views of USAID or the United States Government. Guinea Summary Strategic Objectives Support health care workers and facilities to continue to offer high-quality health services in safe environment by strengthening infection prevention and control (IPC) practices through training, supportive supervision, and complementary monitoring and evaluation. June 02, 2015 to November 15, 2015 (approved July 9, 2015; extension approved through Program Dates XXX) PY1 Approved $2,400,000 Budget Geographic 5 prefectures of Boke, Dabola, Dinguiraye, Faranah, and Mandiana Focus Area No. -

“If You Don't Find Anything, You Can't Eat” – Mining Livelihoods and Income, Gender Roles, and Food Choices In
Resources Policy 70 (2021) 101939 Contents lists available at ScienceDirect Resources Policy journal homepage: http://www.elsevier.com/locate/resourpol “If you don’t findanything, you can’t eat” – Mining livelihoods and income, gender roles, and food choices in northern Guinea Ronald Stokes-Walters a,d,*, Mohammed Lamine Fofana b, Joseph Lamil´e Songbono c, Alpha Oumar Barry c, Sadio Diallo c, Stella Nordhagen b,e, Laetitia X. Zhang a, Rolf D. Klemm a,b, Peter J. Winch a a Department of International Health, Johns Hopkins Bloomberg School of Public Health – 615 N Wolfe St, Baltimore, MD, 21205, USA b Helen Keller International – One Dag Hammarskjold Plaza, Floor 2, New York, NY, 10017, United States c Julius Nyerere University of Kankan, Kankan, Guinea d Action Against Hunger USA, One Whitehall St, Second Floor, New York NY, 10004, United States e Global Alliance for Improved Nutrition (GAIN), Rue de Vermont 37-39, 1202, Geneva, Switzerland ARTICLE INFO ABSTRACT Keywords: Artisanal and small-scale mining (ASM) continues to grow as a viable economic activity in sub-Saharan Africa. Artisanal mining The health and environmental impacts of the industry, notably linked to the use of potentially toxic chemicals, Food choice has been well documented. What has not been explored to the same extent is how pressures associated with ASM Women’s workload affect food choices of individuals and families living in mining camps. This paper presents research conducted in Income instability 18 mining sites in northern Guinea exploring food choices and the various factors affecting food decision-making Guinea practices. Two of the most influentialfactors to emerge from this study are income variability and gender roles. -

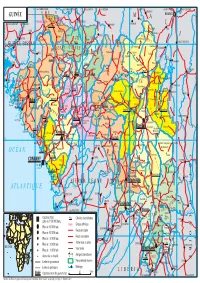
Guinea : Reference Map of Kankan Region (As of 3 March 2015)
Guinea : Reference Map of Kankan Region (as of 3 March 2015) Bankolen Mambifagalena Niagassola Kry Tourelen Berlen Sokoromansa Magadiano Faraboloni Linkekoro KIGNEKOUROU CENTRE Bouyido Malsadou Seourou Konfara 2 Gnembou Tanssa Magnaka KOTE CENTRE Balenda SOUMBARAYA CENTRE Kourelen TALABE CENTRE Dialawassa II Kondoko Djanwely Itipony Dougounta Dora Kourakoda DIBIA CENTRE Djinko Ilimalo Naboun Kanimbakalako Kodougoulen KAKAMA CENTRE Tondo Komagron Kayaga Kignedi Sininko Kadabili Kignero Gnere Sininkoro Badamako Kounsounkoro Yirikelèma Kanikoumbaya SOKORO CENTRE DIATEA CENTRE Dita Salla Tondji1 Koda Kebesabaya Siguirini Sakounou Malea Bembéta Megnèkoma Silabado Diakan Toukönö BOULAN CENTRE Gbèdela MANKADIAN CENTRE Gbörökola Doko Tombani Maragbè Kana Sékela Mansadji Sidao Tonso Banankölö Tomba Doula Amina Amina Kinièba Franwalia Tinko Diatifere Fountou Soumbalakölen Iroda Kounkoun Koda Mainou SARAYA CENTRE Tomboni Sinimbaya KOBEDRA CENTRE MIGNADA CENTRE Bökökö Farani Banora Simbona Bida Tomba Boufe Bandioula FOULATA CENTRE Kintinian Yorola Tougnou Sanouna SEELA CENTRE Bankon MALI Tinkoba Kobada Beretela Sando Noumandiana Kandani Fodela Bèrèko Tabakoro BAMBALA Tabako Madila Moyafara Kourouni Banantamou Siguiri FALAMA BANFARA CENTRE Saint Alexis Dialakoro Nedekoroko Banantou Lansanaya Sakolado Manakoro Farabada Dounin Farabelen Bida Bantambaye Woléwoléya Koda Koda Kogne Tambabougou Gbongoroma Kigne Kokoudouninda Dinguiraye Gbilin Balandougouba KONKOYE CENTRE Waran-Fougou Kiniebakoura DIARRADOU CENTRE Sansani Faradjian Tassiliman Centre Kewoulé -

Région De Kankan 2018
REPUBLIQUE DE GUINEE Travail - Justice- Solidarité MINISTERE DU PLAN ET DU DEVELOPPEMENT ECONOMIQUE La région de Kankan en chiffres Edition 2020 GEOGRAPHIE ET ORGANISATION ADMINISTRATIVE Géographie 0rganisation administrative en 2018 5 préfectures ; 53 sous-préfectures ; 5 communes urbaines, Superficie = 72 145km2 920 districts/quartiers ; 2 117 secteurs 53 communes rurales Source : BSD Ministère de l’administration du territoire et de la décentralisation (Annuaire statistique 2018) Préfectures Sous-préfectures Balandougou, Bate-Nafadji, Boula, Gberedou-Baranama, Karifamoriyah, Koumban, Kankan Mamouroudou, Missamana, Moribayah, Sabadou-Baranama, Tinti-Oulen, Tokounou Kérouané Banankoro, Damaro, Komodou, Kounsankoro, Linko, Sibiribaro, Soromaya Babila, Balato, Banfele, Baro, Cissela, Douako, Doura, Kiniero, Komola-Koura, Koumana, Kouroussa Sanguiana Balandougouba, Dialakoro, Faralako, Kantoumania, Kinieran, Kondianakoro, Koundian, Morodou, Mandiana Niantania, Saladou, Sansando Banko, Doko, Faranwalia, Kiniebakoura, Kintinian, Malea, Naboun, Niagossola, Niandankoro, Siguiri Norassoba, Nounkounkan, Siguirini Source : BSD Ministère de l’administration du territoire et de la décentralisation (Annuaire statistique 2018) STATISTIQUES DEMOGRAPHIQUES Population 1983 1996 2014 Population région de Kankan 640 432 1 011 644 1 972 537 Population de la principale préfecture : Siguiri 161 303 271 224 687 002 Part de la population nationale en 2014 : 18,7 % Rang régional en 2018 : 1/8 Sources : Institut national de la statistique/RGPH Population au 1er -

Scientific Coordinator's Report
P L E C N E W S A N D V I E W S No. 14 NOVEMBER 1999 PRINCIPAL SCIENTIFIC COORDINATOR’S REPORT 1 Highlights of the period April–November 1999 The new trend: helping to restore diversity 2 Demonstrating the value of agrodiversity in Ghana 3 New approaches, new methods, new mind-sets 3 Advances in survey methodology 4 Methodological papers in this issue 4 ‘Vive WAPLEC: Vive le PLEC’: Guinée September 1999 5 The workshop at Pita A visit to Moussaya, upper Niger 5 General remarks 6 MAY 1999 UNU/PLEC-BAG MEETING: SUMMARY AND DATA FORMS 7 D.J. Zarin, with inputs from Guo Huijun, Lewis Enu-Kwesi and Liang Luohui ATTRIBUTES REQUIRED OF THE NEW EXPERT 8 Comments by Professor E. Laing PAPER FROM THE DEMONSTRATION ACTIVITIES ADVISORY TEAM (DAT) 11 DAT facilitating the exchange of experiences in demonstration activities Miguel Pinedo-Vásquez SOME PLEC DEFINITIONS, WITH CODES FOR DATA-BASE PURPOSES 17 from the Editors A DIARY OF MEETINGS ATTENDED BY PLEC MEMBERS, MARCH– 18 NOVEMBER 1999 PAPERS BY PROJECT MEMBERS Mapping of settlements in an evolving PLEC demonstration site in Northern Ghana: an 19 example in collaborative and participatory work The late A.S. Abdulai, E.A. Gyasi and S.K. Kufogbe with assistance of P.K. Adraki, F. Asante, M.A. Asumah, B.Z. Gandaa, B.D. Ofori and A.S. Sumani Agrodiversity highlights in East Africa 25 F. Kaihura, R. Kiome, M. Stocking, A. Tengberg and J. Tumuhairwe An enlargement of PLEC work in Mexico 33 edited from a proposal to PLEC by Carlos Arriaga-Jordán A DIRECTORY OF PLEC DEMONSTRATION SITES, with date of firm 38 establishment, names of cluster leaders and e-mail and fax addresses P L E C N E W S A N D V I E W S No. -

REPUBLIC of GUINEA Labor–Justice–Solidarity
REPUBLIC OF GUINEA Labor–Justice–Solidarity MINISTRY OF AGRICULTURE AND LIVESTOCK NATIONAL STRATEGY FOR THE DEVELOPMENT OF RICE GROWING APRIL 2009 Table of contents LIST OF ACRONYMS AND ABBREVIATIONS 5 SUMMARY 6 I. INTRODUCTION 8 II. REVIEWING THE RICE SECTOR 9 2.1. The policy position of rice 10 2.2 Preferences and demand estimates 10 2.3 Typology and number of rice farmers, processors and marketers 11 2.4. Gender dimensions 13 2.5. Comparative advantage of national rice production 14 III. CHALLENGES AND OPPORTUNITIES 14 3.1. The potential of local rice for rural poverty reduction and economic growth 14 3.2. The land system 15 3.3. Social issues 16 3.4. Trans-border and regional issues 16 3.5. Knowledge and lessons learnt from R&D in rice 16 VI. PRIORITY AREAS AND PERSPECTIVES 17 4.1. Ranking by order of priority in terms of potential contribution to national production 17 4.2. Identification and ranking specific environmental challenges and related opportunities by order of priority 18 4.3. Identification of policy challenges/opportunities 20 4.3.1. Policy challenges 20 4.3.1. Opportunities 21 V. VISION AND FRAMEWORK OF THE NATIONAL RICE STRATEGY 21 5.1. Objectives of rice production 21 5.5.1. Overall target: 21 5.5.2. Quantified objectives: 21 5.2.3. Strategy development phase 23 5.2.4. Key interventions 24 5.2.5 Scientists, technicians and agricultural advisory agents in 2008 and beyond 25 5.2.6. Governance of the Rice Growing Development Strategy 25 5.2.7. -
GUINÉE Gam L BAMAKO PARC NAT
14° vers TAMBACOUNDA vers TAMBACOUNDA 12° vers SARAYA vers KÉNÉBIA 10° vers KITA vers KITA 8° vers KOULIKORO vers SÉGOU S É N É G A L F SIRAKORO bie a GUINÉE Gam l BAMAKO PARC NAT. é M m A DU KONIAGUI é GALÉ FOULAKOUNDA BADIAR KÉDOUGOU g L n i B vers ZIGUINCHOR vers KOLDA F f SAGABARI a Youkounkoun ARABA a k Koundara o B y ba ï G Niagassola SIBI ê Sarébo do a G GABU Guingan m o T i b B Balandou I o i al K m T e F LÉ é R iba ouba A A M ok l i Kifaya Tamgué D A o vers BISSAO o L ro F Á K n 1538 m I BA AT Foulamôri é Balaki I Sou baraya N K A É OUÉLÉSSÉBOUGOU 12° GUINÉE-BISSAO Mali L Boukaria 12° B S m a O a Naboun Kouré alé n l y N E - G U I N É o o KANGABA k Y E N E N k a é XIME O a r M m Madina l Ya béring F a ÉL K andanda Maléa B u B I m n Koumbia Sala bandé Doko o Kounsitél É i a e Siguirini Barrage B bi g è è R al m in Diatif r E de Sélingué vers BISSAO ub Gaoual a f Rio Cor G a IG KANGARÉ BUBA oumb B Banora N é K a Koubia Nafadji n Kintinian é i i Dabalaré F m Malanta ô F o K llé ifa BOUGOUNI Wéndou Mbôrou T Ganiakali Siguiri n Fouta Labé T H Dialakoro o Lélouma ougué A g Tin vers SIKASSO o 1245 U kisso K Hamdallaï Kâkoni F L T E Kiniébakoura K O U A Dinguiraye - G Balandougouba CATIÓ LÉ o U I SANSA g Sélouma N É E o ê Dabiss H rico a Kalinko Koundianakoro n Missira Kankalabé Sangarédi m F YANFOLILA i Chutes arakoba Niandankoro r o e k de Kinkon ka s n Sansalé L A Santou a Pita s i ou i m Sansando c U K B k Ko ola Koura Niantanina a u F O Tén n ié M Niani BADOGO L C ing ilin m é i n GARA O T ta Konsota i T a O io Dobali Djalon B m -
MCHIP Guinea End-Of-Project Report October 2010–June 2014
MCHIP Guinea End-of-Project Report October 2010–June 2014 Submitted on: September 15, 2014 Submitted to: United States Agency for International Development under Coooperative Agreement # GHS-A-00-08-00002-000 Submitted by: Yolande Hyjazi, Rachel Waxman and Bethany Arnold 1 The Maternal and Child Health Integrated Program (MCHIP) is the USAID Bureau for Global Health’s flagship maternal, neonatal and child health (MNCH) program. MCHIP supports programming in maternal, newborn and child health, immunization, family planning, malaria, nutrition, and HIV/AIDS, and strongly encourages opportunities for integration. Cross-cutting technical areas include water, sanitation, hygiene, urban health and health systems strengthening. MCHIP brings together a partnership of organizations with demonstrated success in reducing maternal, newborn and child mortality rates and malnutrition. Each partner will take the lead in developing programs around specific technical areas: Jhpiego, as the Prime, will lead maternal health, family planning/reproductive health, and prevention of mother-to-child transmission of HIV (PMTCT); JSI—child health, immunization, and pediatric AIDS; Save the Children—newborn health, community interventions for MNCH, and community mobilization; PATH—nutrition and health technology; JHU/IIP—research and evaluation; Broad Branch—health financing; PSI—social marketing; and ICF International—continues support for the Child Survival and Health Grants Program (CSHGP) and the Malaria Communities Program (MCP). This report was made possible by the generous support of the American people through the United States Agency for International Development (USAID), under the terms of the Leader with Associates Cooperative Agreement GHS-A-00-08-00002-00. The contents are the responsibility of the Maternal and Child Health Integrated Program (MCHIP) and do not necessarily reflect the views of USAID or the United States Government. -

Manuel Des Codes Et Nomenclatures
M A République de Guinée N U E L D E MINISTERE DU PLAN S INSTITUT NATIONAL DE LA STATISTIQUE C O DIRECTION DE LA COORDINATION ET DE LA D PROGRAMMATION STATISTIQUE E S Projet d’Appui au Renforcement des Capacités Statistiques E T (PARCS) N O M COMPENDIUM E N DES STATISTIQUES C L A MANUEL DES CODES ET NOMENCLATURES T U R E S VOLUME II V o l N°ISBN: 9791092480016 ume Imprimé par II Août 2014 Tél: 622 64 59 31 9791092480016 UNION EUROPEENNE TABLE DES MATIERES ADRESSES ET CONTACTS……………………………………………………….…...….2 AVANT PROPOS……………………………………………………………...………....….3 AVERTISSEMENT………………….………………………………………...………....…..4 PRESENTATION DU MANUEL…………………………………………………………….5 OBJECTIF………………………………………………………………….…………………5 DEMARCHE METHODOLOGIQUE ……………….………………………………………5 A- LES CODES GEOGRAPHIQUES ………………………….……….……….……6 B- CODES DES OCCUPATIONS ET DES BRANCHES D’ACTIVITE……..……14 CODES DES PROFESSIONS ET METIERS……………………………………….…...14 Grand groupe 1 : Membres de l’exécutif et du corps législatif, cadres supérieurs de l’administration publique, dirigeants et cadres supérieurs d’entreprise ………………………………..……………….……………....……14 Grand groupe 2 : Professions intellectuelle et scientifiques …….……....…15 Grand groupe 3 : Professions intermédiaires………………………...………19 Grand groupe 4 : Employé de type administratif ………………………….…23 Grand groupe 5 : Personnel des services et vendeurs de magasin et de marché…………………………………………………………… ……….....… 25 Grand groupe 6 : Agriculteurs et ouvriers qualifiés de l’Agriculture et de la Pêche……………………………………………………….… ………...……....26 Grand groupe 7 : Artisans -

Guinea: Poverty Reduction Strategy Paper
REPUBLIC OF GUINEA Work – Justice – Solidarity Ministry of the Economy, Finances and Planning Poverty Reduction Strategy Paper PRSP–2 (2007–2010) Conakry, August 2007 Permanent Secretariat for the Poverty Reduction Strategy (SP-SRP) Website: www.srp-guinee.org.Telephone: (00224) 30 43 10 80. ACKNOWLEDGEMENTS This document is the fruit of a collective effort that has involved many development stakeholders: executives of regionalized and decentralized structures, civil society organizations, development partners, etc. Warm thanks to all of them. The government would particularly like to acknowledge the grassroots organizations and civil society actors who, despite the difficulties that affected the implementation of the PRSP-I, have renewed their confidence in its action. The lessons learned from the implementation of the PRSP-I have helped in the design and preparation of the document. For this, the government again thanks the development partners who have accompanied it in this exercise and provided technical and financial contributions (EU, GTZ, SCAC, Canadian Cooperation), as well as the team of national experts who carried out field work with dedication and professionalism. Furthermore, without the painstaking work carried out in 2005 and 2006 as part of the process of refining the regional PRSPs, it certainly would not have been possible to prepare this document. The same is true of the work done, mainly in 2006, to evaluate needs aimed at reaching the MDGs. In this regard, we thank the United Nations System, and in particular the UNDP, for its exceptional contribution. Finally, the government extends its most sincere thanks to all those, both named and unnamed, who participated in this collective work. -

1 Republique De Guinee
Évaluation Finale du Projet « Renforcement de la Gestion Décentralisée de l’environnement UNDP-GUINEE 2018 pour répondre aux objectifs des Conventions de Rio en Guinée – RGDE » REPUBLIQUE DE GUINEE ____________________________________________________________________ ____________________________________________________________________________________ « Renforcement de la Gestion Décentralisée de l’Environnement pour répondre aux objectifs des Conventions de Rio en Guinée (RGDE-GIN- PIMS-4963 ; ID : 00093877) » ___________________ Rapport d’Évaluation Finale Soumis au PNUD-Guinée Maison Commune, Commune de Matam, Coléah Corniche Sud, Rue MA 002 Conakry, Guinée Par Dr Syaka SADIO, Consultant International, Chef d’équipe Et Alphonse Ngom, Consultant national Août 2018 1 Évaluation Finale du Projet « Renforcement de la Gestion Décentralisée de l’environnement UNDP-GUINEE 2018 pour répondre aux objectifs des Conventions de Rio en Guinée – RGDE » REMERCIEMENTS Les consultants tiennent à exprimer leurs sincères remerciements aux autorités du gouvernement de la Guinée et particulièrement le Ministère de l’Environnement, des Eaux et Forêts (MEEF) et le Programme pour l’environnement et le Développement Durable (PEDD) pour les dispositions prises pour faciliter cette mission et l’atteinte des résultats attendus. Nous remercions tout particulièrement le Bureau du PNUD-Guinée, le Directeur pays et le Directeur Adjoint pays, qui n’ont ménagé aucun effort pour donner des orientations claires à la mission. Aussi, que l’ensemble du personnel, trouve ici l’expression de nos meilleurs sentiments, pour la confiance portée en nous pour conduire l’évaluation terminale du projet, et plus particulièrement Mr. Mamadou Ciré Camara, Team Leader de l’Unité Environnement et Énergie et son équipe, notamment Mamadou kalidou Diallo, chargé du suivi à l’Unité Environnement et Énergie/PNUD, Mr Mamadou Diallo du Procurement -PNUD. -

Camtraco Management Services
CAMTRACO MANAGEMENT SERVICES CONFIDENTIAL This proposal is for the supply, transport by sea, installation and commissioning in Guinea of isolated photovoltaic solar systems for 50 villages. 1. Object The purpose of this project is to provide electricity in rural areas of Guinea. 50 villages were chosen in the first phase for the installation of solar systems with isolated storage capacity adapted to the needs of the connected devices. 2. Locations and insolation NUMBER OF IRRADIATION N° NATURAL REGIONS PREFECTURES VILLAGES VILAGES (kWh/m²/day) DOGMET – KANKAMA - 1 DABOLA 3 4,8 BISSIKIRIMA KINIERAN- SANGUIANA -SARAYA 2 KOUROUSSA 4 5,0 – CISSELA TOKOUNOU-BATENAFAYI- 3 KANKAN SANFINA -TOKOUNOU- 6 5,5 UPPER-GUINEA (24) BATENAFAYI -BALANDOU NORASSOBA-SIGUIRINI- NIANDANKORO – BAFINDA – 4 SIGUIRI DOKO- KOUREMALE – 8 5,5 FRENKAMAYA – KINGNEIBAKOURA – TIGUIBIRI 5 FARANAH TIRO- KOBIKORO- BANYA 3 5,0 1 DUBREKA KONFONYA 1 4,8 2 FRIA TORMELEN- BAGUINET 2 4,8 3 MARITIME GUINEA (11) BOFFA FONFO –KOLO 2 4,8 KOLIA – YONYA – SANGAREKO – 4 BOKE 6 4,8 TANENE – SINEYA -DARI DOUNET –OUREKABA- MARELA – 1 MID-GUINEA (5) MAMOU 5 4,8 TAMAGALE- SARAMOUSAYA 1 MACENTA SEREDOU 1 3,8 2 KISSIDOUGOU YENDE MILLIMOU 1 4,8 3 GUECKEDOU KAMALO – TEKOULO 2 3,8 FORESTED GUINEA (10) BOUNOUMA-KOROPARA- 4 N’ZEREKORE 5 3,8 YALENZOU-SAMOE- KOULE 5 LOLA BOSSOU 1 3,8 Insolation depends on location and meteorological conditions for each site. For power and energy consumption profile data calculated for each consumer of electricity equipment (loads), the insolation of the considered site determines the power of the photovoltaic field (W) and the storage capacity of batteries (Wh).