Accepted Manuscript
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Realizing Constant Current and Constant Voltage Outputs and Input Zero Phase Angle of Wireless Power Transfer Systems with Minimum Component Counts
600 IEEE TRANSACTIONS ON INTELLIGENT TRANSPORTATION SYSTEMS, VOL. 22, NO. 1, JANUARY 2021 Realizing Constant Current and Constant Voltage Outputs and Input Zero Phase Angle of Wireless Power Transfer Systems With Minimum Component Counts Jianghua Lu , Student Member, IEEE, Guorong Zhu , Senior Member, IEEE,DeyanLin,Member, IEEE, Yiming Zhang , Member, IEEE, Haoran Wang , Member, IEEE, and Chunting Chris Mi , Fellow, IEEE Abstract— In both normal and fast wireless electric vehicle advantages of its high specific energy, energy density, and high charging systems, constant current/constant voltage (CC/CV) cycle lifetime. The wireless power transfer (WPT) technology charging profile, regardless of the variation of the battery [1], [2] using magnetic or electric field coupling, namely the state of charge, is one of the most essential characteristics to ensure the battery performance and reliability. The input zero inductive power transfer (IPT) or capacitive power transfer phase angle (ZPA) is able to minimize the system volt-ampere (CPT), provides a promising solution for both normal and fast rating, enhance the power transfer capability, and make it charging [3], [4] of EV Li-ion batteries. Over the full range easy to achieve soft-switching operation over the full range of of the Li-on battery charge, the battery pack equivalent load battery charging profile. Therefore, the load-independent CC and resistance, which defined as the ratio of the charging voltage CV output characteristics with ZPA conditions are necessary for wireless charging systems. However, the existing methods to the charging current, may be roughly from a few ohms to that can achieve these functions either add power switches or several hundred ohms [5]. -
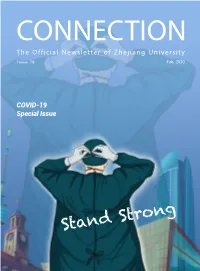
CONNECTION the Official Newsletter of Zhejiang University Issue 16 Feb.2020
CONNECTION The Official Newsletter of Zhejiang University Issue 16 Feb.2020 COVID-19 Special Issue Stand Strong Message from Editor-in-Chief CONNECTION Welcome to the special COVID-19 issue of Issue 16 CONNECTION, which highlights the efforts and contributions of ZJU community in face of the epidemic. As a group, they are heroes in harm's way, givers and doers who respond swiftly to the need of our city, our country and the world. When you read their stories, you'll recognize the strength and solidarity that define all ZJUers. ZJU community has demonstrated its courage and resilience in the battle against the novel coronavirus. At this time, let us all come together to protect ourselves and our loved ones, keep all those who are at the front lines in our prayers and pass on our gratitude to those who have joined and contributed to the fight against the virus. Together, we will weather this crisis. LI Min, Editor-in-Chief Director, Office of Global Engagement Editorial office : Global Communications Office of Global Engagement, Zhejiang University 866 Yuhangtang Road, Hangzhou, P.R. China 310058 Phone: +86 571 88981259 Fax: +86 571 87951315 Email: [email protected] Edited by : CHEN Weiying, AI Ni Designed by : HUANG Zhaoyi Material from Connection may be reproduced accompanied with appropriate acknowledgement. CONTENTS Faculty One of the heroes in harm’s way: LI Lanjuan 03 ZJU medics answered the call from Wuhan 04 Insights from ZJU experts 05 Alumni Fund for Prevention and Control of Viral Infectious Diseases set up 10 Alumni community mobilized in the battle against COVID-19 11 Education Classes start online during the epidemic 15 What ZJUers feel about online learning 15 Efforts to address concerns, avoid misinformation 17 International World standing with us 18 International students lending a hand against the epidemic 20 What our fans say 21 FacultyFaculty ZJU community has taken on the responsibility to join the concertedZJU community efforts has takenagainst on thethe responsibility spreadto join the of concerted the virus. -

Participants: (In Order of the Surname)
Participants 31 Participants: (in order of the surname) Yansong Bai yyyòòòttt: Jilin University, Changchun. E-mail: [email protected] Jianhai Bao ïïï°°°: Central South University, Changsha. E-mail: [email protected] Chuanzhong Chen •••DDD¨¨¨: Hainan Normal University, Haikou. E-mail: [email protected] Dayue Chen •••ŒŒŒ: Peking University, Beijing. E-mail: [email protected] Haotian Chen •••hhhUUU: Jilin University, Changchun. E-mail: [email protected] Longyu Chen •••999ˆˆˆ: Peking University, Beijing. E-mail: [email protected] Man Chen •••ùùù: Capital Normal University, Beijing. E-mail: [email protected] Mu-Fa Chen •••777{{{: Beijing Normal University, Beijing. E-mail: [email protected] Shukai Chen •••ÓÓÓppp: Beijing Normal University, Beijing. E-mail: [email protected] Xia Chen •••ggg: Jilin University, Changchun; University of Tennessee, USA. E-mail: [email protected] Xin Chen •••lll: Shanghai Jiao Tong University, Shanghai. E-mail: [email protected] Xue Chen •••ÆÆÆ: Capital Normal University, Beijing. E-mail: [email protected] Zengjing Chen •••OOO¹¹¹: Shandong University, Jinan. E-mail: [email protected] 32 Participants Huihui Cheng §§§¦¦¦¦¦¦: North China University of Water Resources and Electric Power, Zhengzhou E-mail: [email protected] Lan Cheng §§§===: Central South University, Changsha. E-mail: [email protected] Zhiwen Cheng §§§“““>>>: Beijing Normal University, Beijing. E-mail: [email protected] Michael Choi éééRRRZZZ: The Chinese University of Hong Kong, Shenzhen. E-mail: [email protected] Bowen Deng """ÆÆÆ©©©: Jilin University, Changchun. E-mail: [email protected] Changsong Deng """ttt: Wuhan University, Wuhan. E-mail: [email protected] Xue Ding ¶¶¶ÈÈÈ: Jilin University, Changchun. -

Wuhan University (China) Clinical Medicine MBBS Western Exceptional Class Program
Wuhan University (China) Clinical Medicine MBBS Western Exceptional Class Program A six-year innovative program specially tailored to students of western countries -An opportunity for high school juniors and seniors who are interested in entering the medical field from your respective school districts. Dear Colleague, It is well known that many American students hoping to enter medical school have their dreams shattered because of high tuition fees and/or low acceptance rates in our colleges of medicine. Fortunately, through a partnership we have with China’s Wuhan University, there is a remedy for these students. In this age of globalization, students can choose to go abroad to complete a degree program that is equivalent to what a U.S. medical school offers. The Wuhan University Medical School program has been offered for more than 10 years. After six years of study after high school, a student can be standing at the same line as a graduate from a U.S. medical school—at considerably less cost. The university is committed to providing international students with quality medical experiences that enable them to become competent physicians with solid medical knowledge while giving due consideration to the possible needs to practice medicine in their home countries or any other country, including China. The bachelor’s degree is approved by the ministry of education in China and is also approved by the World Health Organization. Graduates from the program can directly attend apply for a USMLE exam (U.S. Medical Licensing Examination) in the U.S. We wanted to share this information with you. -

Sichuan University(SCU) Is a National Key Comprehensive University, Incorporated
Sichuan University Sichuan University(SCU) is a national key comprehensive university, incorporated from three key universities, namely, the former Sichuan University, Chengdu University of Science and Technology (CUST) and West China University of Medical Science (WCUMS). Sichuan University offers courses in nine major fields of study including humanities, social sciences, natural sciences, engineering and technology, medical sciences,etc. Sichuan University 24,Southen Section1, 1st Ringroad, 610065, Sichuan,Chengdu, P.R. China Tel:+86-28-85402443 FAX:+86-28-85403260 E-mail:[email protected]. cn Contact Us Sitemap FAQ http://www.scu.org.cn/19.09.2003 01:34:23 Sichuan University SichuanUniversity 24,Southen Section1, 1st Ringroad, 610065, Sichuan,Chengdu, P.R. China Tel:+86-28-85402443 FAX:+86-28-85403260 E-mail:[email protected] E-mail:[email protected] http://www.scu.org.cn/CONT.htm19.09.2003 01:34:35 Sichuan University Home Genaral Information History of SCU About SCU A welcome from the President Eximious Schoolfellow Academics Degrees Admission Program Oversea Students Science Technology Medicine Research Literae Humaniores International Cooperation Library Resource Museum Hospital News&Events Map Campus Life Living Service Students' Assn. Foreign Experts Employment Overseas Schoolars http://www.scu.org.cn/sitemap.htm19.09.2003 01:34:52 Sichuan University General Information As one of the national key universities directly under the State Ministry of Education (MOE) as well as one of the State “211 Project” universities enjoying privileged construction in the Ninth Five-Year Plan period, the present Sichuan University (SCU) was first incorporated with Chengdu University of Science and Technology (CUST), another national key university under the MOE in1994, and West China General Information University of Medical Science (WCUMS), a key university directly subordinated to History of SCU the State Ministry of Health in 2000. -

Universities and the Chinese Defense Technology Workforce
December 2020 Universities and the Chinese Defense Technology Workforce CSET Issue Brief AUTHORS Ryan Fedasiuk Emily Weinstein Table of Contents Executive Summary ............................................................................................... 3 Introduction ............................................................................................................ 5 Methodology and Scope ..................................................................................... 6 Part I: China’s Defense Companies Recruit from Civilian Universities ............... 9 Part II: Some U.S. Tech Companies Indirectly Support China’s Defense Industry ................................................................................................................ 13 Conclusion .......................................................................................................... 17 Acknowledgments .............................................................................................. 18 Appendix I: Chinese Universities Included in This Report ............................... 19 Appendix II: Breakdown by Employer ............................................................. 20 Endnotes .............................................................................................................. 28 Center for Security and Emerging Technology | 2 Executive Summary Since the mid-2010s, U.S. lawmakers have voiced a broad range of concerns about academic collaboration with the People’s Republic of China (PRC), but the most prominent -

Curriculum Vitae
CURRICULUM VITAE Personal Information 请附上照片 Name Bang Shen Gender Male Position Title professor Working Department Huazhong Agricultural University Email [email protected] Address Wuhan, China Tel 027-87281810 Fax Research Interest Molecular mechanisms governing Toxoplasma parasitism and pathogenesis; carbon metabolism and its regulation;molecular mechanisms that control the transition of acute infection to chronic infection; design of live attenuated anti-toxoplasmic vaccines for animals. Education & Working Experience Academic career 2005 – 2010 Ph.D (Microbiology and Molecular Genetics) University of Kansas Medical Centre, USA 2001 – 2005 Bachelor of Science (Biology) Wuhan University, China Research experience 2014 – Huazhong Agricultural University, Wuhan, China 2010 – 2014 Postdoctoral fellow (Molecular Parasitology) Washington University in St Louis, MO, USA Publications Xia N, Ye S, Liang X, Chen P, Zhou Y, Fang R, Zhao J, Gupta N, Yang S, Yuan J, Shen B*. Pyruvate Homeostasis as a Determinant of Parasite Growth and Metabolic Plasticity in Toxoplasma gondii. MBio. 2019 Jun 11;10(3). pii: e00898-19. doi: 10.1128/mBio.00898-19. Pan M, Li M, Li L, Song Y, Hou L, Zhao J, Shen B* (2019). Identification of Novel Dense-Granule Proteins in Toxoplasma gondii by Two Proximity-Based Biotinylation Approaches. Journal of Proteome Research, 18: 319−330 Xia N, Yang J, Ye S, Zhang L, Zhou Y, Zhao J, David Sibley L, Shen B* (2018). Functional analysis of Toxoplasma lactate dehydrogenases suggests critical roles of lactate fermentation for parasite growth in vivo. Cellular Microbiology, 20(1) Xia N, Zhou T, Liang X, Ye S, Zhao P, Yang J, Zhou Y, Zhao J, Shen B* (2018). -

College Codes (Outside the United States)
COLLEGE CODES (OUTSIDE THE UNITED STATES) ACT CODE COLLEGE NAME COUNTRY 7143 ARGENTINA UNIV OF MANAGEMENT ARGENTINA 7139 NATIONAL UNIVERSITY OF ENTRE RIOS ARGENTINA 6694 NATIONAL UNIVERSITY OF TUCUMAN ARGENTINA 7205 TECHNICAL INST OF BUENOS AIRES ARGENTINA 6673 UNIVERSIDAD DE BELGRANO ARGENTINA 6000 BALLARAT COLLEGE OF ADVANCED EDUCATION AUSTRALIA 7271 BOND UNIVERSITY AUSTRALIA 7122 CENTRAL QUEENSLAND UNIVERSITY AUSTRALIA 7334 CHARLES STURT UNIVERSITY AUSTRALIA 6610 CURTIN UNIVERSITY EXCHANGE PROG AUSTRALIA 6600 CURTIN UNIVERSITY OF TECHNOLOGY AUSTRALIA 7038 DEAKIN UNIVERSITY AUSTRALIA 6863 EDITH COWAN UNIVERSITY AUSTRALIA 7090 GRIFFITH UNIVERSITY AUSTRALIA 6901 LA TROBE UNIVERSITY AUSTRALIA 6001 MACQUARIE UNIVERSITY AUSTRALIA 6497 MELBOURNE COLLEGE OF ADV EDUCATION AUSTRALIA 6832 MONASH UNIVERSITY AUSTRALIA 7281 PERTH INST OF BUSINESS & TECH AUSTRALIA 6002 QUEENSLAND INSTITUTE OF TECH AUSTRALIA 6341 ROYAL MELBOURNE INST TECH EXCHANGE PROG AUSTRALIA 6537 ROYAL MELBOURNE INSTITUTE OF TECHNOLOGY AUSTRALIA 6671 SWINBURNE INSTITUTE OF TECH AUSTRALIA 7296 THE UNIVERSITY OF MELBOURNE AUSTRALIA 7317 UNIV OF MELBOURNE EXCHANGE PROGRAM AUSTRALIA 7287 UNIV OF NEW SO WALES EXCHG PROG AUSTRALIA 6737 UNIV OF QUEENSLAND EXCHANGE PROGRAM AUSTRALIA 6756 UNIV OF SYDNEY EXCHANGE PROGRAM AUSTRALIA 7289 UNIV OF WESTERN AUSTRALIA EXCHG PRO AUSTRALIA 7332 UNIVERSITY OF ADELAIDE AUSTRALIA 7142 UNIVERSITY OF CANBERRA AUSTRALIA 7027 UNIVERSITY OF NEW SOUTH WALES AUSTRALIA 7276 UNIVERSITY OF NEWCASTLE AUSTRALIA 6331 UNIVERSITY OF QUEENSLAND AUSTRALIA 7265 UNIVERSITY -

更好luojia International Summer Program
Luojia International Summer Program Understanding China 汇报⼈:海湾同学社 Contact Us ISPT (International Summer Program Team) Study Abroad Section, Office of International Affairs 2020 June 28 - July 15 Wuhan University Email: [email protected] Phone: +86-27-68779092 Website: en.whu.edu.cn About Wuhan University The campus of Wuhan University is located in Wuhan, capital city of Hubei Province in the middle reaches of the Yangtze River. Flanked by East Lake and with a splendid integration of ever-green Luojia Hill and palatial architectural complex on its campus, Wuhan University is widely acclaimed as the most beautiful campus in China. CONTENTS The history of Wuhan University can be traced back to Ziqiang Institute, which was founded in 1893 by Zhang Zhidong, the then governor of Hubei and Hunan Provinces in the late Qing Dynasty. Through ages of About Wuhan University 03 development, Wuhan University has now grown into a top 10 comprehensive university in Mainland China. It offers a wide range of About 2020 Luojia International Summer Program 04 disciplines through six faculties, namely, humanities, sciences, social sciences, information science, engineering and medical science. Tutors 05 Burgeoning are the international exchanges and cooperation of Wuhan University in recent years. It has established cooperative relationships with Program Schedule & Assessment 12 more than 415 universities and research institutes in over 45 countries and regions. Now Wuhan University is endeavoring to shape itself into a world- Tuition & Fees 15 class comprehensive research university domestically and internationally. Eligibility & How to Apply 16 03 About 2020 Luojia International Tutors Summer Program BALZ, Timo Professor, State Key Laboratory of Information — Understanding China Engineering in Surveying, Mapping and Remote Sensing (LIESMARS), Wuhan University Luojia International Summer Program was initiated by Wuhan University in 2006. -

China Venture Fund
CHINA VENTURE FUND 2018-2019 China Venture Fund Scholars Name Proposal Title Partner Institution(s) Department College North China Plain and Texas High Plains: Collaboration between Geography & the Liberal Arts & Social 1 FeiFei Pan China Agricultural University UNT and China Agricultural Environment Sciences University Collaborative Research Activities Texas Center for Xinghai Conservatory 2 Kris Chesky with the Texas Center for Performing Arts Music Zhaoqing University Performing Arts Health Health Research, Education, and Peking University Recruiting Collaboration with Shanghai Jiao Tong University Biomedical 3 Donghui Zhu Engineering Biomedical Engineering Programs Northwest Institute for Nonferrous Engineering at Top Universities in China Metal Research Housing International Recognized Engineering 4 Cheng Yu Tsinghua University Engineering Researcher on Disaster Mitigation Technology Page 1 of 6 Last Updated: 01/07/2019 CHINA VENTURE FUND 2017-2018 China Venture Fund Scholars Name Proposal Title Partner Institution(s) Department College East China Normal University Enhancing Research & Shanghai University of Sport Kinesiology, Health 1 Tao Zhang Recruitment with Universities in Shanghai University Promotion, & Education China East China Jiaotong University Recreation Beijing Sport University Establishing Education & Engineering 2 Cheng Yu Beijing University of Technology Engineering Research Partnership with BJUT Technology Research and Education Collaboration with School of Computer Science & 3 Yan Huang Computer Science -

Information Sheet (2019-2020)
Information Sheet (2019-2020) University Information Name of Institution Wuhan University University Homepage http://en.whu.edu.cn Address No.299, Luojia Hill, Wuchang District, Wuhan, Hubei Province, China General Information Wuhan University (WHU) is a comprehensive and key national university directly under the administration of China’s Ministry of Education, and it’s one of the top ten universities in China. WHU covers a wide range of disciplines and is honored as the "Most Beautiful University in China". Since its establishment, Wuhan University has cultivated more than 300,000 professional talents in various occupations. Number of Students 54,084 Contact Information Central Office Wuhan University International Office E-mail Address [email protected] Mailing Address Address: 101 Office, School of International Education, Wuhan University, Wuhan, 430072, Hubei Province, China Contact person: Ms. Feng Wenzhu Tel: +86-27-68753912 Website for School of International Education http://admission.whu.edu.cn International Students Contacts Coordination and Partnership in general: Ms. Zhang Wenjia --- Inbound Students Tel: +86-27-68770701 Fax: +86-27-68779873 E-mail: [email protected] Student Application and Admission: Ms.Feng Wenzhu --- Admissions Office Tel: +86-27-68753912 Fax: +86-27-87863154 E-mail: [email protected] Student Services: Ms. LIU, Yebing --- Student Administration Office Tel: +86-27-68752590 Fax: +86-27-87863154 E-mail: [email protected] Course Selection and Transcript: Ms. WU, Yulan --- Teaching Affairs Office Tel: +86-27-68752041 E-mail: [email protected] International Students School of International Education Management Please note: There are two sections involved in dealing with exchange student affairs in WHU—the office of international affairs and the School of International Education (SIE). -

3. List of Participants
3. List of Participants Ziad Adwan, Department of Mathematics, University of Texas at Brownsville, 80 Fort Brown, Brownsville, TX 78520 , USA [email protected] Daniel Barlet, Institut Universitaire de France et Institut Elie Cartan UMR 7502, Nancy-Universit´e, CNRS, INRIA, BP 239 - F - 54506 Vandoeuvre- l´es-Nancy Cedex, France [email protected] Hongzhe Cao ( ¨ ´ ), Department of Mathematics, Nanchang University, Nanchang 330031, China [email protected] Tingbin Cao ( ¨ Ò £), Department of Mathematics, Nanchang University, Nanchang 330031, China [email protected] Der-Chen Chang, Department of Mathematics, Georgetown University, Wash- ington, DC 20057, USA [email protected] Hua Chen ( «·), School of Mathematics and Statistics, Wuhan University, Wuhan 430072, China [email protected] Lvping Chen ( « Ê), School of Mathematical Sciences, Xiamen Univer- sity, Xiamen 361005, China [email protected] Minru Chen ( « Ä ℄), Department of Mathematics, Henan University, Kaifeng 475004, China [email protected] ¸ Renyu Chen ( « ), Department of Mathematics, Tianjing University, Tianjing 300072, China [email protected] 26 Æ Wenyi Chen ( «Û ), School of Mathematics and Statistics, Wuhan Uni- versity, Wuhan 430072, China [email protected] £ Xueyong Chen ( « ), School of Mathematics and Statistics, Wuhan Uni- versity, Wuhan 430072, China Í Zeqian Chen ( « ), Wuhan Institute of Physics and Mathematics,Wuhan 430071, China [email protected] ° ¶ Zhihua Chen ( « ), Department of Mathematics, Tongji University, Shang- hai 200092, China [email protected]