Comprehensive Physiology Development of the Pituitary Gland
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Shh/Gli Signaling in Anterior Pituitary
SHH/GLI SIGNALING IN ANTERIOR PITUITARY AND VENTRAL TELENCEPHALON DEVELOPMENT by YIWEI WANG Submitted in partial fulfillment of the requirements For the degree of Doctor of Philosophy Department of Genetics CASE WESTERN RESERVE UNIVERSITY January, 2011 CASE WESTERN RESERVE UNIVERSITY SCHOOL OF GRADUATE STUDIES We hereby approve the thesis/dissertation of _____________________________________________________ candidate for the ______________________degree *. (signed)_______________________________________________ (chair of the committee) ________________________________________________ ________________________________________________ ________________________________________________ ________________________________________________ ________________________________________________ (date) _______________________ *We also certify that written approval has been obtained for any proprietary material contained therein. TABLE OF CONTENTS Table of Contents ••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••• i List of Figures ••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••• v List of Abbreviations •••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••• vii Acknowledgements •••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••• ix Abstract ••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••• x Chapter 1 Background and Significance ••••••••••••••••••••••••••••••••••••••••••••••••• 1 1.1 Introduction to the pituitary gland -

SUPPLEMENTARY MATERIAL Bone Morphogenetic Protein 4 Promotes
www.intjdevbiol.com doi: 10.1387/ijdb.160040mk SUPPLEMENTARY MATERIAL corresponding to: Bone morphogenetic protein 4 promotes craniofacial neural crest induction from human pluripotent stem cells SUMIYO MIMURA, MIKA SUGA, KAORI OKADA, MASAKI KINEHARA, HIROKI NIKAWA and MIHO K. FURUE* *Address correspondence to: Miho Kusuda Furue. Laboratory of Stem Cell Cultures, National Institutes of Biomedical Innovation, Health and Nutrition, 7-6-8, Saito-Asagi, Ibaraki, Osaka 567-0085, Japan. Tel: 81-72-641-9819. Fax: 81-72-641-9812. E-mail: [email protected] Full text for this paper is available at: http://dx.doi.org/10.1387/ijdb.160040mk TABLE S1 PRIMER LIST FOR QRT-PCR Gene forward reverse AP2α AATTTCTCAACCGACAACATT ATCTGTTTTGTAGCCAGGAGC CDX2 CTGGAGCTGGAGAAGGAGTTTC ATTTTAACCTGCCTCTCAGAGAGC DLX1 AGTTTGCAGTTGCAGGCTTT CCCTGCTTCATCAGCTTCTT FOXD3 CAGCGGTTCGGCGGGAGG TGAGTGAGAGGTTGTGGCGGATG GAPDH CAAAGTTGTCATGGATGACC CCATGGAGAAGGCTGGGG MSX1 GGATCAGACTTCGGAGAGTGAACT GCCTTCCCTTTAACCCTCACA NANOG TGAACCTCAGCTACAAACAG TGGTGGTAGGAAGAGTAAAG OCT4 GACAGGGGGAGGGGAGGAGCTAGG CTTCCCTCCAACCAGTTGCCCCAAA PAX3 TTGCAATGGCCTCTCAC AGGGGAGAGCGCGTAATC PAX6 GTCCATCTTTGCTTGGGAAA TAGCCAGGTTGCGAAGAACT p75 TCATCCCTGTCTATTGCTCCA TGTTCTGCTTGCAGCTGTTC SOX9 AATGGAGCAGCGAAATCAAC CAGAGAGATTTAGCACACTGATC SOX10 GACCAGTACCCGCACCTG CGCTTGTCACTTTCGTTCAG Suppl. Fig. S1. Comparison of the gene expression profiles of the ES cells and the cells induced by NC and NC-B condition. Scatter plots compares the normalized expression of every gene on the array (refer to Table S3). The central line -

The Viral Oncoproteins Tax and HBZ Reprogram the Cellular Mrna Splicing Landscape
bioRxiv preprint doi: https://doi.org/10.1101/2021.01.18.427104; this version posted January 18, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. The viral oncoproteins Tax and HBZ reprogram the cellular mRNA splicing landscape Charlotte Vandermeulen1,2,3, Tina O’Grady3, Bartimee Galvan3, Majid Cherkaoui1, Alice Desbuleux1,2,4,5, Georges Coppin1,2,4,5, Julien Olivet1,2,4,5, Lamya Ben Ameur6, Keisuke Kataoka7, Seishi Ogawa7, Marc Thiry8, Franck Mortreux6, Michael A. Calderwood2,4,5, David E. Hill2,4,5, Johan Van Weyenbergh9, Benoit Charloteaux2,4,5,10, Marc Vidal2,4*, Franck Dequiedt3*, and Jean-Claude Twizere1,2,11* 1Laboratory of Viral Interactomes, GIGA Institute, University of Liege, Liege, Belgium.2Center for Cancer Systems Biology (CCSB), Dana-Farber Cancer Institute, Boston, MA, USA.3Laboratory of Gene Expression and Cancer, GIGA Institute, University of Liege, Liege, Belgium.4Department of Genetics, Blavatnik Institute, Harvard Medical School, Boston, MA, USA. 5Department of Cancer Biology, Dana-Farber Cancer Institute, Boston, MA, USA.6Laboratory of Biology and Modeling of the Cell, CNRS UMR 5239, INSERM U1210, University of Lyon, Lyon, France.7Department of Pathology and Tumor Biology, Kyoto University, Japan.8Unit of Cell and Tissue Biology, GIGA Institute, University of Liege, Liege, Belgium.9Laboratory of Clinical and Epidemiological Virology, Rega Institute for Medical Research, Department of Microbiology, Immunology and Transplantation, Catholic University of Leuven, Leuven, Belgium.10Department of Human Genetics, CHU of Liege, University of Liege, Liege, Belgium.11Lead Contact. *Correspondence: [email protected]; [email protected]; [email protected] bioRxiv preprint doi: https://doi.org/10.1101/2021.01.18.427104; this version posted January 18, 2021. -
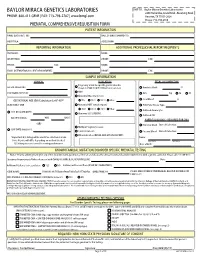
Prenatal Testing Requisition Form
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 PRENATAL COMPREHENSIVE REQUISITION FORM PATIENT INFORMATION NAME (LAST,FIRST, MI): DATE OF BIRTH (MM/DD/YY): HOSPITAL#: ACCESSION#: REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: SAMPLE INFORMATION CLINICAL INDICATION FETAL SPECIMEN TYPE Pregnancy at risk for specific genetic disorder DATE OF COLLECTION: (Complete FAMILIAL MUTATION information below) Amniotic Fluid: cc AMA PERFORMING PHYSICIAN: CVS: mg TA TC Abnormal Maternal Screen: Fetal Blood: cc GESTATIONAL AGE (GA) Calculation for AF-AFP* NTD TRI 21 TRI 18 Other: SELECT ONLY ONE: Abnormal NIPT (attach report): POC/Fetal Tissue, Type: TRI 21 TRI 13 TRI 18 Other: Cultured Amniocytes U/S DATE (MM/DD/YY): Abnormal U/S (SPECIFY): Cultured CVS GA ON U/S DATE: WKS DAYS PARENTAL BLOODS - REQUIRED FOR CMA -OR- Maternal Blood Date of Collection: Multiple Pregnancy Losses LMP DATE (MM/DD/YY): Parental Concern Paternal Blood Date of Collection: Other Indication (DETAIL AND ATTACH REPORT): *Important: U/S dating will be used if no selection is made. Name: Note: Results will differ depending on method checked. Last Name First Name U/S dating increases overall screening performance. Date of Birth: KNOWN FAMILIAL MUTATION/DISORDER SPECIFIC PRENATAL TESTING Notice: Prior to ordering testing for any of the disorders listed, you must call the lab and discuss the clinical history and sample requirements with a genetic counselor. -

PDF Download
Review Xatzipsalti Maria et al. Congenital Hypopituitarism: Various Genes, … Horm Metab Res 2018; 00: 00–00 Congenital Hypopituitarism: Various Genes, Various Phenotypes Authors Maria Xatzipsalti1, 2, Antonis Voutetakis1, Lela Stamoyannou2, George P. Chrousos1, Christina Kanaka-Gantenbein1 Affiliations ABSTRacT 1 Division of Endocrinology, Diabetes and Metabolism, The ontogenesis and development of the pituitary gland is a First Department of Pediatrics, Medical School, National highly complex process that depends on a cascade of transcrip- and Kapodistrian University of Athens, “Aghia Sofia” tion factors and signaling molecules. Spontaneous mutations Children's Hospital, Athens, Greece and transgenic murine models have demonstrated a role for 2 First Department of Pediatrics, “Aglaia Kyriakou” many of these factors, including HESX1, PROP1, PIT1, LHX3, Children's Hospital, Athens, Greece LHX4, SOX2, SOX3, OTX2, PAX6, FGFR1, SHH, GLI2, and FGF8 in the etiology of congenital hypopituitarism. Genetic muta- Key words tions in any of these factors can lead to congenital hypopitui- pituitary, combined pituitary hormone deficiency, congenital tarism, which is characterized by the deficiency in one or more hypopituitarism, transcription factors, syndromic hypopitui- pituitary hormones. The phenotype can be highly variable, tarism, non-syndromic hypopituitarism consisting of isolated hypopituitarism or more complex disor- ders. The same phenotype can be attributed to different gene received 27.03.2018 mutations; while a given gene mutation can -

Rapid Evolution of Mammalian X-Linked Testis-Expressed Homeobox Genes
Copyright 2004 by the Genetics Society of America DOI: 10.1534/genetics.103.025072 Rapid Evolution of Mammalian X-Linked Testis-Expressed Homeobox Genes Xiaoxia Wang and Jianzhi Zhang1 Department of Ecology and Evolutionary Biology, University of Michigan, Ann Arbor, Michigan 48109 Manuscript received November 26, 2003 Accepted for publication February 11, 2004 ABSTRACT Homeobox genes encode transcription factors that function in various developmental processes and are usually evolutionarily conserved in their sequences. However, two X-chromosome-linked testis-expressed homeobox genes, one from rodents and the other from fruit flies, are known to evolve rapidly under positive Darwinian selection. Here we report yet another case, from primates. TGIFLX is an X-linked homeobox gene that originated by retroposition of the autosomal gene TGIF2, most likely in a common ancestor of rodents and primates. While TGIF2 is ubiquitously expressed, TGIFLX is exclusively expressed in adult testis. A comparison of the TGIFLX sequences among 16 anthropoid primates revealed a signifi- cantly higher rate of nonsynonymous nucleotide substitution (dN) than synonymous substitution (dS), strongly suggesting the action of positive selection. Although the high dN/dS ratio is most evident outside ف the homeobox, the homeobox has a dN/dS of 0.89 and includes two codons that are likely under selection. Furthermore, the rate of radical amino acid substitutions that alter amino acid charge is significantly greater than that of conservative substitutions, suggesting that the selection promotes diversity of the protein charge profile. More interestingly, an analysis of 64 orthologous homeobox genes from humans and mice shows substantially higher rates of amino acid substitution in X-linked testis-expressed genes than in other genes. -

Comparative Genomics Reveals Functional Transcriptional Control Sequences in the Prop1 Gene
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by UNL | Libraries University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln U.S. Department of Agriculture: Agricultural Publications from USDA-ARS / UNL Faculty Research Service, Lincoln, Nebraska August 2007 Comparative genomics reveals functional transcriptional control sequences in the Prop1 gene Robert D. Ward University of Michigan MinChul Cho University of Michigan S. A. Camper University of Michigan Shannon W. Davis University of Michigan Lori T. Raetzman University of Michigan See next page for additional authors Follow this and additional works at: https://digitalcommons.unl.edu/usdaarsfacpub Part of the Agricultural Science Commons Ward, Robert D.; Cho, MinChul; Camper, S. A.; Davis, Shannon W.; Raetzman, Lori T.; Smith, Timothy P.L.; Esposito, Constance; Lyons, Robert H.; Cheng, Jan-Fang; Rubin, Edward M.; and Rhodes, Simon J., "Comparative genomics reveals functional transcriptional control sequences in the Prop1 gene" (2007). Publications from USDA-ARS / UNL Faculty. 222. https://digitalcommons.unl.edu/usdaarsfacpub/222 This Article is brought to you for free and open access by the U.S. Department of Agriculture: Agricultural Research Service, Lincoln, Nebraska at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Publications from USDA-ARS / UNL Faculty by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Authors Robert D. Ward, MinChul Cho, S. A. Camper, Shannon W. Davis, Lori T. Raetzman, Timothy P.L. Smith, Constance Esposito, Robert H. Lyons, Jan-Fang Cheng, Edward M. Rubin, and Simon J. Rhodes This article is available at DigitalCommons@University of Nebraska - Lincoln: https://digitalcommons.unl.edu/ usdaarsfacpub/222 Mamm Genome (2007) 18:521–537 DOI 10.1007/s00335-007-9008-6 Comparative genomics reveals functional transcriptional control sequences in the Prop1 gene Robert D. -

Genomics 93 (2009) 449–460
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Genomics 93 (2009) 449–460 Contents lists available at ScienceDirect Genomics journal homepage: www.elsevier.com/locate/ygeno Discovery of transcriptional regulators and signaling pathways in the developing pituitary gland by bioinformatic and genomic approaches Michelle L. Brinkmeier a, Shannon W. Davis a, Piero Carninci b, James W. MacDonald c, Jun Kawai b, Debashis Ghosh e,1, Yoshihide Hayashizaki b, Robert H. Lyons d, Sally A. Camper a,⁎ a Department of Human Genetics, University of Michigan Medical School, Ann Arbor, MI, 48109-5618, USA b Omics Science Center, RIKEN Yokohama Institute, Suehiro-cho, Tsurumi-ku, Yokohama, Kanagawa 230-0045, Japan c Affymetrix and cDNA Microarray Core Facility, University of Michigan Cancer Center, Ann Arbor, MI 48109-0946, USA d Department of Biological Chemistry, University of Michigan Medical School, Ann Arbor, MI, 48109-5638, USA e Department of Biostatistics, School of Public Health, University of Michigan, 48109-2029, USA article info abstract Article history: We report a catalog of the mouse embryonic pituitary gland transcriptome consisting of five cDNA libraries Received 13 December 2007 including wild type tissue from E12.5 and E14.5, Prop1df/df mutant at E14.5, and two cDNA subtractions: E14.5 Accepted 24 November 2008 WT–E14.5 Prop1df/df and E14.5 WT–E12.5 WT. DNA sequence information is assembled into a searchable Available online 11 February 2009 database with gene ontology terms representing 12,009 expressed genes. We validated coverage of the libraries by detecting most known homeobox gene transcription factor cDNAs. -

Lamprecht Et Al, Supplementary Data 1 Suppl. Figure S1. Specificity
Lamprecht et al, Supplementary Data Suppl. Figure S1. Specificity of PBX3 protein detection. (A) Representative immunohistochemistry of PBX3 in normal colonic mucosa. Scale bar, 100 µm. (B) Immunoblotting for indicated proteins in lysates of normal colonic mucosa and colon cancer tissue, derived from the same patient. (C) Immunoblotting for indicated proteins on whole cell lysates of SW480 and LoVo colon cancer cells after PBX3 or control (siCtrl) knockdown by siRNA for 72 h. (D) Amino acid sequences of PBX3 isoforms obtained from UniProt (www.uniprot.org) and immunogen sequence (epitope) for PBX3 monoclonal antibody (M01), clone 1A9 (Abnova). UniProt identifiers are P40426-1 (PBX3A), P40426-2 (PBX3B), P40426-3 (PBX3C), P40426-4 (PBX3D) and P40426-5 (PBX3-5). 1 Lamprecht et al, Supplementary Data Suppl. Figure S2. Effects of WNT repression on PBX3 in colon cancer cells. Immunoblotting for indicated proteins on whole cell lysates of indicated cell lines 72 h after transfection with two different siRNAs targeting β-catenin or with control siRNA (siCtrl). Numbers below immunoblots indicate normalized fold change by densitometry. n ≥ 3. 2 Lamprecht et al, Supplementary Data Suppl. Figure S3. Lack of transcriptional regulation of PBX3 expression by WNT. (A) Illustration of putative TCF/LEF binding elements (TBEs) within 2.5 kb of the PBX3 transcriptional start site (upper panel), and sequences of wild-type (WT) and mutated (MUT) TBEs used for luciferase assays (lower panel). (B) Dual luciferase assays with empty pBV-Luc vector or vector containing 2.5 kb of the PBX3 promoter region with wild-type (WT) or mutated (MUT) TBEs 24 h after stimulation of HEK293T cells with WNT3a or without stimulation (Ctrl). -

Congenital Hypopituitarism: How to Select the Patients for Genetic
Crisafulli et al. Italian Journal of Pediatrics (2018) 44:47 https://doi.org/10.1186/s13052-018-0484-y COMMENTARY Open Access Congenital hypopituitarism: how to select the patients for genetic analyses Giuseppe Crisafulli, Tommaso Aversa, Giuseppina Zirilli, Filippo De Luca*, Romina Gallizzi and Malgorzata Wasniewska Abstract Aim of this commentary is to analyze the relationships between genotypic bases and phenotypic expression of congenital “multiple pituitary hormone deficiency” (MPHD) syndrome and to indicate some reliable criteria for selecting the patients who should undergo genetic analyses in order to clarify the etiology of their disorder. On the basis of the most recent reports on this topic, it is possible to infer that: 1) in only few patients with congenital MPHD it is possible to detect a causative gene mutation; 2) therefore, it is fundamental to define some criteria for selecting the patients who should undergo genetic analyses; 3) such inclusion criteria should be based on the overall evaluation of hormonal clinical and neuroradiological phenotype; 4) it is crucial to consider whether the cases are sporadic or familial, since the probability of finding a causative gene mutation is distinctly higher in familial cases; 5) for PROP1 gene it is also important to consider the geographical origin of the patients, because this mutation is much more frequent in some ethnic groups. Keywords: Causative gene mutations, Combined pituitary hormone deficiency, HESX1 gene, LHX3 and LHX4 genes, Multiple pituitary hormone deficiency, POU1F1 gene, PROP1 gene Background familial or sporadic hypopituitarism and those with iso- GH deficiency (GHD) is a relatively uncommon patho- lated GHD or multiple pituitary hormone deficiency logical condition, which should always be considered in (MPHD) [2]. -

Pituitary Stem Cell Regulation: Who Is Pulling the Strings?
234 3 B COX, H ROOSE and others Pathways regulating pituitary 234:3 R135–R158 Review stem cells Pituitary stem cell regulation: who is pulling the strings? Correspondence Benoit Cox*, Heleen Roose*, Annelies Vennekens and Hugo Vankelecom should be addressed Department of Development and Regeneration, Cluster of Stem Cell and Developmental Biology, to H Vankelecom Unit of Stem Cell Research, University of Leuven (KU Leuven), Leuven, Belgium Email *(B Cox and H Roose contributed equally to this work) Hugo.Vankelecom@ kuleuven.be Abstract The pituitary gland plays a pivotal role in the endocrine system, steering fundamental Key Words processes of growth, metabolism, reproduction and coping with stress. The adult f pituitary pituitary contains resident stem cells, which are highly quiescent in homeostatic f stem cells conditions. However, the cells show marked signs of activation during processes f regulation of increased cell remodeling in the gland, including maturation at neonatal age, f homeostasis adaptation to physiological demands, regeneration upon injury and growth of local f regeneration tumors. Although functions of pituitary stem cells are slowly but gradually uncovered, f tumor their regulation largely remains virgin territory. Since postnatal stem cells in general f NOTCH reiterate embryonic developmental pathways, attention is first being given to f WNT Endocrinology of regulatory networks involved in pituitary embryogenesis. Here, we give an overview of f Hedgehog the current knowledge on the NOTCH, WNT, epithelial–mesenchymal transition, SHH f epithelial–mesenchymal and Hippo pathways in the pituitary stem/progenitor cell compartment during various transition Journal (activation) conditions from embryonic over neonatal to adult age. Most information f Hippo comes from expression analyses of molecular components belonging to these networks, f SOX2 whereas functional extrapolation is still very limited. -

PROP1-Related Combined Pituitary Hormone Deficiency
Title: PROP1-Related Combined Pituitary Hormone Deficiency GeneReview – LHX4 Variants Author: de Graaff L Date: August 2014 Note: The following information is provided by the authors listed above and has not been reviewed by GeneReviews staff. Specific variants in LHX4 • In a French family with CPHD, pituitary and cerebellar defects, and abnormalities of the sella turcica, Machinis et al [2001] identified a G-to-C transversion (IVS4, G-C, -1) in four affected members. • Pfaeffle et al [2008] identified three heterozygous missense LHX4 variants (p.Arg84Cys, p.Ala210Pro, and p.Leu190Arg) in five persons out of 253 individuals from 245 families with CPHD. In structural models and functional studies the p.Ala210Pro and p.Leu190Arg mutant proteins showed impaired DNA binding and impaired gene activation, causing the protein to be inactive. The p.Arg84Cys mutant protein showed only reduced activity. • Castinetti et al [2008] found a new variant in the protein sequence of LHX4 (Thr99fs) in one of 136 individuals with CPHD and malformations of the brain, pituitary stalk, or posterior pituitary gland [Castinetti et al 2008]. • Tajima et al [2007] found a de novo heterozygous Pro366-to-Thr (p.Pro366Thr) substitution in a conserved residue in the C terminus in a 16-month-old Japanese girl with severe CPHD, pituitary defects, small sella turcica, and Chiari malformation. The variant was not found in 80 Japanese controls [Tajima et al 2007]. • In 2010, Dateki et al identified a de novo heterozygous 522,009-bp deletion involving LHX4 in a patient with CPHD (GH, TSH, PRL, LH, and FSH deficiencies), anterior pituitary hypoplasia, ectopic posterior pituitary, and underdeveloped sella turcica.