Cronicon OPEN ACCESS EC MICROBIOLOGY Research Article
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-
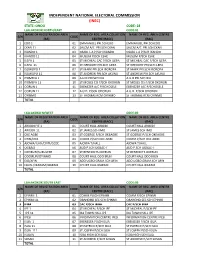
Ondo Code: 28 Lga:Akokok North/East Code:01 Name of Registration Area Name of Reg
INDEPENDENT NATIONAL ELECTORAL COMMISSION (INEC) STATE: ONDO CODE: 28 LGA:AKOKOK NORTH/EAST CODE:01 NAME OF REGISTRATION AREA NAME OF REG. AREA COLLATION NAME OF REG. AREA CENTRE S/N CODE (RA) CENTRE (RACC) (RAC) 1 EDO 1 01 EMMANUEL PRI.SCHEDO EMMANUEL PRI.SCHEDO 2 EKAN 11 02 SALEM A/C PRI.SCH EKAN SALEM A/C PRI.SCH EKAN 3 IKANDO 1 03 OSABL L.A P/SCH IKANDO OSABL L.A P/SCH IKANDO 4 IKANDO 11 04 MUSLIM P/SCH ESHE MUSLIM P/SCH ESHE 5 ILEPA 1 05 ST MICHEAL CAC P/SCH ILEPA ST MICHEAL CAC P/SCH ILEPA 6 ILEPA 11 06 ST GREGORY PRI.SCH ILEPA ST GREGORY PRI.SCH ILEPA 7 ISOWOPO 1 07 ST MARK PRI.SCH IBOROPA ST MARK PRI.SCH IBOROPA 8 ISOWOPO 11 08 ST ANDREW PRI.SCH AKUNU ST ANDREW PRI.SCH AKUNU 9 IYOMEFA 1 09 A.U.D PRI.SCH IKU A.U.D PRI.SCH IKU 10 IYOMEFA 11 10 ST MOSES CIS P/SCH OKORUN ST MOSES CIS P/SCH OKORUN 11 OORUN 1 11 EBENEZER A/C P/SCHOSELE EBENEZER A/C P/SCHOSELE 12 OORUN 11 12 A.U.D. P/SCH ODORUN A.U.D. P/SCH ODORUN 13 OYINMO 13 ST THOMAS RCM OYINMO ST THOMAS RCM OYINMO TOTAL LGA:AKOKO N/WEST CODE:02 NAME OF REGISTRATION AREA NAME OF REG. AREA COLLATION NAME OF REG. AREA CENTRE S/N CODE (RA) CENTRE (RACC) (RAC) 1 ARIGIDI IYE 1 01 COURT HALL ARIGIDI COURT HALL ARIGIDI 2 ARIGIDI 11 02 ST JAMES SCH IMO ST JAMES SCH IMO 3 OKE AGBE 03 ST GOERGE P/SCH OKEAGBE ST GOERGE P/SCH OKEAGBE 4 OYIN/OGE 04 COMM.P/SCH OKE AGBE COMM.P/SCH OKE AGBE 5 AJOWA/ILASI/ERITI/GEDE 05 AJOWA T/HALL AJOWA T/HALL 6 OGBAGI 06 AUD P.SCH OGBAC-I AUD P.SCH OGBAC-I 7 OKEIRUN/SURULERE 07 ST BENEDICTS OKERUN ST BENEDICTS OKERUN 8 ODOIRUN/OYINMO 08 COURT HALL ODO IRUN COURT HALL ODO IRUN 9 ESE/AFIN 09 ADO UGBO GRAM.SCH AFIN ADO UGBO GRAM.SCH AFIN 10 EBUSU/IKARAM/IBARAM 10 COURT HALL IKARAM COURT HALL IKARAM TOTAL LGA:AKOKOK SOUTH EAST CODE:03 NAME OF REGISTRATION AREA NAME OF REG. -

A Historical Survey of Socio-Political Administration in Akure Region up to the Contemporary Period
European Scientific Journal August edition vol. 8, No.18 ISSN: 1857 – 7881 (Print) e - ISSN 1857- 7431 A HISTORICAL SURVEY OF SOCIO-POLITICAL ADMINISTRATION IN AKURE REGION UP TO THE CONTEMPORARY PERIOD Afe, Adedayo Emmanuel, PhD Department of Historyand International Studies,AdekunleAjasin University,Akungba-Akoko, Ondo State, Nigeria Abstract Thepaper examines the political transformation of Akureregion from the earliest times to the present. The paper traces these stages of political development in order to demonstrate features associated with each stage. It argues further that pre-colonial Akure region, like other Yoruba regions, had a workable political system headed by a monarch. However, the Native Authority Ordinance of 1916, which brought about the establishment of the Native Courts and British judicial administration in the region led to the decline in the political power of the traditional institution.Even after independence, the traditional political institution has continually been subjugated. The work relies on both oral and written sources, which were critically examined. The paper, therefore,argues that even with its present political status in the contemporary Nigerian politics, the traditional political institution is still relevant to the development of thesociety. Keywords: Akure, Political, Social, Traditional and Authority Introduction The paper reviews the political administration ofAkure region from the earliest time to the present and examines the implication of the dynamics between the two periods may have for the future. Thus,assessment of the indigenous political administration, which was prevalent before the incursion of the colonial administration, the political administration during the colonial rule and the present political administration in the region are examined herein.However, Akure, in this context, comprises the present Akure North, Akure South, and Ifedore Local Government Areas of Ondo State, Nigeria. -

Nigeria's Constitution of 1999
PDF generated: 26 Aug 2021, 16:42 constituteproject.org Nigeria's Constitution of 1999 This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:42 Table of contents Preamble . 5 Chapter I: General Provisions . 5 Part I: Federal Republic of Nigeria . 5 Part II: Powers of the Federal Republic of Nigeria . 6 Chapter II: Fundamental Objectives and Directive Principles of State Policy . 13 Chapter III: Citizenship . 17 Chapter IV: Fundamental Rights . 20 Chapter V: The Legislature . 28 Part I: National Assembly . 28 A. Composition and Staff of National Assembly . 28 B. Procedure for Summoning and Dissolution of National Assembly . 29 C. Qualifications for Membership of National Assembly and Right of Attendance . 32 D. Elections to National Assembly . 35 E. Powers and Control over Public Funds . 36 Part II: House of Assembly of a State . 40 A. Composition and Staff of House of Assembly . 40 B. Procedure for Summoning and Dissolution of House of Assembly . 41 C. Qualification for Membership of House of Assembly and Right of Attendance . 43 D. Elections to a House of Assembly . 45 E. Powers and Control over Public Funds . 47 Chapter VI: The Executive . 50 Part I: Federal Executive . 50 A. The President of the Federation . 50 B. Establishment of Certain Federal Executive Bodies . 58 C. Public Revenue . 61 D. The Public Service of the Federation . 63 Part II: State Executive . 65 A. Governor of a State . 65 B. Establishment of Certain State Executive Bodies . -

Petroleum Extraction, Agriculture and Local Communities in the Niger Delta
Petroleum Extraction, Agriculture and Local Communities in the Niger Delta. A Case of Ilaje Community. Adedayo Ladelokun Howard University Chapter I: Introduction Petroleum resource exploration and extraction-- ● A crucial economic activity ● Petroleum resources contributed substantially to economic development ● Conversely, petroleum exploration and extraction often induce negative impacts on other economic activities such as agriculture. ● Threatens environmental Safety. ● Ilaje Community,Ondo State,Nigeria, was chosen as a case study. Introduction Cont. ● Location and member states of the Niger Delta. Located in Coastal Southern Region of Nigeria. Map of the Niger Delta region Niger Delta Image of the Niger Delta Source: Ken Saro-Wiwa 20 years on Niger Delta ... Cnn.com Map of Ondo State Showing the 18 Local Government Areas Ilaje Local Government Introduction Cont. ● Population --- Estimated at 46 Million(UNDP) ● Geographical Landmark --- ND Covers area over 70,000 Sq Kilometers (ie 27,000 Miles) ● Occupation --- Farming, Fishing, Canoe Making, Trading, Net Making, and Mat Making. ● Ilaje Community --- Occupies Atlantic Coastline of Ondo State,Nigeria. ● Ilaje Local Government (Polluted Area) was one of the 18 Local Governments in Ondo State, Nigeria. ● Five Local Governments were randomly selected to served as control. Scope of the study This research work will cover Ilaje Community in Ondo State. Ondo State is located in the petroleum producing area of the Niger Delta Ilaje community was mainly into agricultural production Chapter II: Literature Review ● Agriculture in Economic Development of Nigeria: ○ Machinery for life sustenance ○ Supportive role raw material provision for industrial development ○ Todaro MP (2000) viewed role of AG as passive and supportive ○ Precondition for eco developed ○ Rapid structural transformation of the AG sector Literature Review Continues Jhingan M.L (1985) opined that: (a) AG provides food surplus for the rapidly expanding population. -

Involvement of Rural Households in Oil Palm (Elaeis Guineensis) Fruits Postharvest Activities in Ondo State, Nigeria
Creative Commons User License: CC BY-NC-ND Journal of Agricultural Extension Abstracted by: EBSCOhost, Electronic Journals Service (EJS), Vol. 24 (1) January, 2020 Google Scholar, Journal Seek, Scientific Commons, ISSN(e): 24086851; ISSN(Print); 1119944X Food and Agricultural Organization (FAO), CABI and Scopus http://journal.aesonnigeria.org http://www.ajol.info/index.php/jae http://eoi.citefactor.org/10.11226/v23i4 Email: [email protected] Involvement of Rural Households in Oil Palm (Elaeis guineensis) Fruits Postharvest Activities in Ondo State, Nigeria https://dx.doi.org/10.4314/jae.v24i1.5 Alabi, Dorcas Lola Department of Agricultural Extension and Rural Development, Faculty of Agriculture, Obafemi Awolowo University, Ile-Ife. Nigeria. [email protected] +2348062915547 Famakinwa, Michael Department of Agricultural Extension and Rural Development, Faculty of Agriculture, Obafemi Awolowo University, Ile-Ife. Nigeria. [email protected] +2347039530266 Akinnawonu, Oluwakemi Esther Department of Agricultural Extension and Rural Development, Faculty of Agriculture, Obafemi Awolowo University, Ile-Ife. Nigeria. [email protected] +234816529546 Abstract The study assessed the involvement of rural households in oil palm fruits post- harvest activities (PHAs) in Ondo State, Nigeria. Specifically, examined their perception towards involvement in oil palm fruits PHAs; identified oil palm fruit PHAs respondents were involved in; determined their level of involvement in those activities and identified constraints associated with their involvement. A multi-stage sampling procedure was used to select 120 processors from selected 3 LGAs in Ondo State. Data were collected using structured interview schedule and summarized with percentages, means and standard deviations while correlation and chi-square analyses were used to draw inference on hypothesis. -

Gender Sensitivity to Public School Enrolment in Ondo State, Nigeria Using Systematic Sampling
DOI: http://dx.doi.org/10.4314/gjpas.v22i1.8 GLOBAL JOURNAL OF PURE AND APPLIED SCIENCES VOL. 22, 2016: 61-71 COPYRIGHT© BACHUDO SCIENCE CO. LTD PRINTED IN NIGERIA ISSN 1118-0579 61 www.globaljournalseries.com, Email: [email protected] GENDER SENSITIVITY TO PUBLIC SCHOOL ENROLMENT IN ONDO STATE, NIGERIA USING SYSTEMATIC SAMPLING ADEDAYO AMOS ADEWARA AND ADEBOLA ANTHONIA ADENIYI (Received 15 December 2015; Revision Accepted 3 March 2016) ABSTRACT This study employed the total number of public schools in Ondo, Nigeria which gives information on the name of the school, males and females in each school from JSS1 to SS3 in the eighteen local government areas. Systematic sampling was used to select forty eight schools from the two hundred and eighty eight public schools in the state during the 2012/2013 and 2013/2014 academic sections. Applying the instrument of Pearson product moment correlation coefficient, the study revealed that (i).females are more sensitive to public school enrolment during 2012/2013 and 2013/2014 academic sessions than their males counterparts, (ii).there is significant difference between the female enrolments during the two academic sessions, (iii).there is significant difference between the male enrolments during the two academic sessions and (iv). the trend of male female enrolments in the selected public schools shows improvement during 2013/2014 over that of 2012/2013 academic session. KEYWORD: Gender, Sensitivity, Systematic Sampling, School, Enrolment INTRODUCTION University of Technology, Akure, Adekunle Ajasin University, Akungba/Akoko, Ondo State polytechnic, The foundation of any state is in the number of Owo, Federal College of Agriculture, Akure and people who are literate in that particular state. -
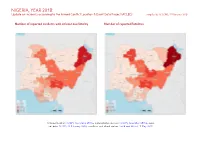
NIGERIA, YEAR 2018: Update on Incidents According to the Armed Conflict Location & Event Data Project (ACLED) Compiled by ACCORD, 25 February 2020
NIGERIA, YEAR 2018: Update on incidents according to the Armed Conflict Location & Event Data Project (ACLED) compiled by ACCORD, 25 February 2020 Number of reported incidents with at least one fatality Number of reported fatalities National borders: GADM, November 2015a; administrative divisions: GADM, November 2015b; incid- ent data: ACLED, 22 February 2020; coastlines and inland waters: Smith and Wessel, 1 May 2015 NIGERIA, YEAR 2018: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 25 FEBRUARY 2020 Contents Conflict incidents by category Number of Number of reported fatalities 1 Number of Number of Category incidents with at incidents fatalities Number of reported incidents with at least one fatality 1 least one fatality Violence against civilians 705 566 2853 Conflict incidents by category 2 Battles 474 373 2470 Development of conflict incidents from 2009 to 2018 2 Protests 427 3 3 Riots 213 61 154 Methodology 3 Strategic developments 117 3 4 Conflict incidents per province 4 Explosions / Remote 100 84 759 violence Localization of conflict incidents 4 Total 2036 1090 6243 Disclaimer 8 This table is based on data from ACLED (datasets used: ACLED, 22 February 2020). Development of conflict incidents from 2009 to 2018 This graph is based on data from ACLED (datasets used: ACLED, 22 February 2020). 2 NIGERIA, YEAR 2018: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 25 FEBRUARY 2020 Methodology on what level of detail is reported. Thus, towns may represent the wider region in which an incident occured, or the provincial capital may be used if only the province The data used in this report was collected by the Armed Conflict Location & Event is known. -

Ondo State Universal Basic Education Board, Oda Road, Akure Invitation for Pre-Qualification of Contractors and Tender for Year
Ondo State Universal Basic Education Board, Oda Road, Akure Invitation for Pre-qualification of Contractors and Tender for Year 2009-2010 (Merged) Education Trust Fund Projects The Ondo State Universal Basic Education Board hereby invites registered, experienced and reputable contractors to pre-qualify and tender for the under-listed jobs: Lot Job Description Construction of a prototype block of 3-Classroom with office and Store at Agboriki 1 Comprehensive JHS, Ikare-Akoko Construction of a prototype block of 3-Classroom with office and Store at Ajuta JHS, 2 Ogbagi-Akoko Construction of a prototype block of 3-Classroom with office and Store at Community 3 JHS, Ifira-Akoko Construction of a prototype block of 3-Classroom with office and Store at Community 4 JHS, Akungba-Akoko Construction of a prototype block of 3-Classroom with office and Store at St. Peter’s 5 C.A.C JHS, Ondo Construction of a prototype block of 3-Classroom with office and Store at Community 6 JHS, Apomu-Akure Construction of a prototype block of 3-Classroom with office and Store at Community 7 JHS, Ojuala in Ese-Odo Construction of a prototype block of 3-Classroom with office and Store at Methodist 8 JHS, Idanre Construction of a prototype block of 3-Classroom with office and Store at Ayo JGS, 9 Ipogun, Ifedore LGA Construction of a prototype block of 3-Classroom with office and Store at Ilejemeje 10 JGS, Mahintedo-Ilaje LGA Construction of a prototype block of 3-Classroom with office and Store at 11 Comprehensive JHS, Erusu-Akoko Construction of a prototype block of 3-Classroom with office and Store at L.A primary 12 school, Ifira-Akoko Construction of a prototype block of 3-Classroom with office and Store at Oke- 13 Oluwatedo CPS, Akure Construction of a prototype block of 3-Classroom with office and Store at Methodist 14 Primary School, Baleju Oke in Ese-Odo LGA Construction of a prototype block of 3-Classroom with office and Store at L.A 15 Primary School, Iju Akure North Construction of a prototype block of 3-Classroom with office and Store at St. -

The Case Study of Owo LGA, Ondo State, Nigeria
The International Journal Of Engineering And Science (IJES) ||Volume||2 ||Issue|| 9 ||Pages|| 19-31||2013|| ISSN(e): 2319 – 1813 ISSN(p): 2319 – 1805 Geo-Information for Urban Waste Disposal and Management: The Case Study of Owo LGA, Ondo State, Nigeria *1Dr. Michael Ajide Oyinloye and 2Modebola-Fadimine Funmilayo Tokunbo Department of Urban and Regional Planning, School of Environmental Technology, Federal University of Technology, Akure, Nigeria --------------------------------------------------------ABSTRACT-------------------------------------------------- Management of waste is a global environmental issue that requires special attention for the maintenance of quality environment. It has been observed that amount, size, nature and complexity of waste generated by man are profoundly influenced by the level of urbanization and intensity of socio-economical development in a given settlement. The problem associated with its management ranges from waste generation, collection, transportation, treatment and disposal. The study involves a kind of multi-criteria evaluation method by using geographical information technology as a practical instrument to determine the most suitable sites of landfill location in Owo Local Government Area of Ondo state. Landsat Enhanced Thematic Mapper plus (ETM+) 2002 and updated 2012 were used to map the most suitable site for waste disposal in Owo LGA. The result indicates that sites were found within the study area. The most suitable sites in the study area are located at 200metre buffer to surface water and 100metre to major and minor roads. The selected areas have 2500metres buffer zone distance from urban areas (built up areas). The study purposes acceptable landfill sites for solid waste disposal in the study area. The results achieved in this study will help policy and decision makers to take appropriate decision in considering sanitary landfill sites. -

A Focus on Federal University of Technology Akure, Nigeria
American Journal of Humanities and Social Sciences Vo1. 1, No. 3, 2013, 163-173 DOI: 10.11634/232907811301364 Monitoring Spatial Growth of Educational Institution using GIS: A Focus on Federal University of Technology Akure, Nigeria Micheal Ajide Oyinloye Department of Urban and Regional Planning, School of Environmental Technology, Federal University of Technology Akure, Nigeria Land use/ land cover changes is an important components in understanding the interaction of human activities with its environment, therefore it is necessary to analyze such change. The land use/landcover dynamics of Federal University of Technology Akure(FUTA) for a period of sixteen years was analyzed using Multi-temporal and Multi-source image of LandSat (TM) of 1986, LandSat (ETM+) of 2002and Quick bird satellite image of 2012. Maximum likelihood (MAL) supervised digital image classification method was employed using ILWIS 3.2 and Arcview 3.1 GIS software. Eight landcover/landuse classes were created: Built up area, Dense forest, Bareland, Exposed soil, Forest reserves, Gulley forest, Light forest and Rock-out crop. Change information was derived by comparing the classified maps. The results showed that the landcover in the study area has changed during the periods especially the built-up area has increased rapidly for the periods ( 1986- 2012).The results also show increase the bareland, exposed rock out crops while forest reserves, gulley forest and light forest decrease between the same periods. Based on exponential growth formulae, the future prediction of the landuse and landcover change and its subsequent development was modeled between 2012 and 2032.These results could help in providing information for decision and planning purpose and also provide management strategies initiatives that are crucial for such expansion in the study area. -

By Rural Women in Ondo State, Nigeria
British Journal of Education, Society & Behavioural Science 12(2): 1-9, 2016, Article no.BJESBS.18208 ISSN: 2278-0998 SCIENCEDOMAIN international www.sciencedomain.org Determinants of the Level of Utilization of Maternal Health Care Services ‘Abiye Programme’ by Rural Women in Ondo State, Nigeria O. O. Fasina 1, F. I. Wole-Alo 1* and F. L. Idowu 1 1Department of Agricultural Extension and Communication Technology, Federal University of Technology, Akure, Ondo State, Nigeria. Authors’ contributions This work was carried out in collaboration between all authors. Authors OOF and FIWA designed the study, wrote the protocol and supervised the work. Authors OOF and FLI carried out all laboratories work and performed the statistical analysis. Author OOF managed the analyses of the study. Author FLI wrote the first draft of the manuscript. Author FIWA managed the literature searches and edited the manuscript. All authors read and approved the final manuscript. Article Information DOI: 10.9734/BJESBS/2016/18208 Editor(s): (1) Manouchehr (Mitch) Mokhtari, School of Public Health, University of Maryland, College Park, USA. (2) Tyree Oredein, Health Education & Behavioral Sciences, University of Medicine and Dentistry of New Jersey, USA. (3) Madine VanderPlaat, Department of Sociology and Criminology, Saint Mary's University, Canada. (4) Chan Shen, Department of Biostatistics, University of Texas, USA. Reviewers: (1) Ryan michael f. Oducado, West Visayas State University, Philippines. (2) Anonymous, University of Malaya, Malaysia. (3) Anonymous, The American University in Cairo, Egypt. Complete Peer review History: http://sciencedomain.org/review-history/11604 Received 9th April 2015 Accepted 2nd September 2015 Original Research Article th Published 28 September 2015 ABSTRACT This study examined factors affecting the utilization of maternal health care services ‘Abiye programme’ by rural women of Ondo State, Nigeria. -

Ondo State Conflictbulletin: Nigeria
THE FUND FOR PEACE Nigeria Conflict Bulletin: Ondo State Patterns and Trends, January 2012 - J u n e 2 0 1 5 While violence in Ondo has historically Democratic Party (PDP). The next page shows the relative distribution of been relatively low, in the first half of 2015 gubernatorial elections are scheduled for incidents from one LGA to the next from reported fatalities increased significantly as 2016. January 2012 to June 2015. The trendline on compared to previous years. This was the next page shows the number of mainly in connection to a few incidents of This Conflict Bulletin provides a brief incidents and fatalities over time. The bar criminality (bank robberies in Owo and snapshot of the trends and patterns of chart shows the relative trend of incidents Akoko North West LGAs) and piracy (Ilaje conflict risk factors at the State and LGA of insecurity by LGA per capita. LGA) that killed dozens. Other issues, levels, drawing on the data available on the reported in Ondo included political tensions P4P Digital Platform for Multi-Stakeholder The summaries draw on data collected by and cult violence. Engagement (www.p4p-nigerdelta.org). It ACLED, FFP’s UNLocK, the Council on represents a compilation of the data from Foreign Relations’ NST, WANEP Nigeria, CSS/ After the 2012 gubernatorial election, in the sources listed below, not necessarily the ETH Zurich, NEEWS2015, and Nigeria Watch which Olusegun Mimiko of the Labour Party opinions of FFP or any other organization integrated on the P4P platform. They also (LP) was re-elected, the losing parties raised that collaborated on the production of this draw on data and information from concerns about alleged election bulletin.