Promising and Best Practices in Hiv/Aids Prevention and Care for West and Central Africa
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

KWAHU AFRAM PLAINS SOUTH DISTRICT SUB- PROGRAMME 1.3 Planning, Budgeting and Coordination
Table of Contents PART A: STRATEGIC OVERVIEW ........................................................................................................ 6 1. ESTABLISHMENT OF THE DISTRICT ......................................................................................... 6 POPULATION STRUCTURE ................................................................................................. 6 2. VISION ................................................................................................................................................. 7 4. GOALS ................................................................................................................................................ 7 REPUBLIC OF GHANA 5. CORE FUNCTIONS ........................................................................................................................... 7 6. DISTRICT ECONOMY ...................................................................................................................... 9 a. AGRICULTURE ................................................................................................................................. 9 b. MARKET CENTER .......................................................................................................................... 10 COMPOSITE BUDGET e. HEALTH ............................................................................................................................................ 13 5. KEY ACHIEVEMENTS IN 2019 ................................................................................................... -
![Addressing the Causes and Consequences of the Farmer-Herder Conflict in Ghana [ Margaret Adomako]](https://docslib.b-cdn.net/cover/5843/addressing-the-causes-and-consequences-of-the-farmer-herder-conflict-in-ghana-margaret-adomako-175843.webp)
Addressing the Causes and Consequences of the Farmer-Herder Conflict in Ghana [ Margaret Adomako]
KOFI ANNAN INTERNATIONAL PEACEKEEPING TRAINING CENTRE POLICY BRIEF 6 | September 2019 Addressing the Causes and Consequences of the Farmer-Herder Conflict in Ghana [ Margaret Adomako] SUMMARY For several years, tensions have existed between local farmers and Fulani herdsmen in Ghana. However, various factors have recently, contributed to the tensions taking on a violent nature and becoming one of Ghana’s foremost security threats. Based on an extensive fieldwork conducted in 2016/2017, this policy brief discusses the causes of the Farmer-herder conflict and its consequences on the security, social and economic structures of the country. It looks at the shortfalls of Operation Cowleg, the major intervention that has been implemented by the state and concludes with a few policy relevant recommendations which includes a nationwide registration of herdsmen to support the government in the implementation of an effective taxation system. INTRODUCTION night grazing. The Asante Akyem North district of Ghana has Beginning from the late 1990s, the farmer-herder conflict has recorded various cases of this nature as a result of its lush become a recurring annual challenge for the Government vegetation. The district has a wet semi-equatorial climate with of Ghana. This conflict usually occurs between local farmers annual total rainfall between 125cm and 175cm making it a and herdsmen, mostly of the Fulani origin, over grazing lands favorite spot for crop farming2 and animal grazing especially and water sources in certain parts of Ghana. The conflict has in the dry season.3 Usually, during the dry season, herders been prevalent in Agogo, in the Ashanti region, and Afram from towns such as Donkorkrom and Ekyiamanfrom pass Plains in the Eastern region, although there have also been through Agogo on their way to Kumawu and Nyantakurom in recorded incidences in some parts of the Northern and Brong search of pasture during the dry season. -
NW SW Presence Map Complete Copy
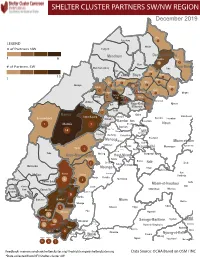
SHELTER CLUSTER PARTNERS SW/NWMap creation da tREGIONe: 06/12/2018 December 2019 Ako Furu-Awa 1 LEGEND Misaje # of Partners NW Fungom Menchum Donga-Mantung 1 6 Nkambe Nwa 3 1 Bum # of Partners SW Menchum-Valley Ndu Mayo-Banyo Wum Noni 1 Fundong Nkum 15 Boyo 1 1 Njinikom Kumbo Oku 1 Bafut 1 Belo Akwaya 1 3 1 Njikwa Bui Mbven 1 2 Mezam 2 Jakiri Mbengwi Babessi 1 Magba Bamenda Tubah 2 2 Bamenda Ndop Momo 6b 3 4 2 3 Bangourain Widikum Ngie Bamenda Bali 1 Ngo-Ketunjia Njimom Balikumbat Batibo Santa 2 Manyu Galim Upper Bayang Babadjou Malentouen Eyumodjock Wabane Koutaba Foumban Bambo7 tos Kouoptamo 1 Mamfe 7 Lebialem M ouda Noun Batcham Bafoussam Alou Fongo-Tongo 2e 14 Nkong-Ni BafouMssamif 1eir Fontem Dschang Penka-Michel Bamendjou Poumougne Foumbot MenouaFokoué Mbam-et-Kim Baham Djebem Santchou Bandja Batié Massangam Ngambé-Tikar Nguti Koung-Khi 1 Banka Bangou Kekem Toko Kupe-Manenguba Melong Haut-Nkam Bangangté Bafang Bana Bangem Banwa Bazou Baré-Bakem Ndé 1 Bakou Deuk Mundemba Nord-Makombé Moungo Tonga Makénéné Konye Nkongsamba 1er Kon Ndian Tombel Yambetta Manjo Nlonako Isangele 5 1 Nkondjock Dikome Balue Bafia Kumba Mbam-et-Inoubou Kombo Loum Kiiki Kombo Itindi Ekondo Titi Ndikiniméki Nitoukou Abedimo Meme Njombé-Penja 9 Mombo Idabato Bamusso Kumba 1 Nkam Bokito Kumba Mbanga 1 Yabassi Yingui Ndom Mbonge Muyuka Fiko Ngambé 6 Nyanon Lekié West-Coast Sanaga-Maritime Monatélé 5 Fako Dibombari Douala 55 Buea 5e Massock-Songloulou Evodoula Tiko Nguibassal Limbe1 Douala 4e Edéa 2e Okola Limbe 2 6 Douala Dibamba Limbe 3 Douala 6e Wou3rei Pouma Nyong-et-Kellé Douala 6e Dibang Limbe 1 Limbe 2 Limbe 3 Dizangué Ngwei Ngog-Mapubi Matomb Lobo 13 54 1 Feedback: [email protected]/ [email protected] Data Source: OCHA Based on OSM / INC *Data collected from NFI/Shelter cluster 4W. -

Forecasts and Dekadal Climate Alerts for the Period 1St to 10Th June 2021
REPUBLIQUE DU CAMEROUN REPUBLIC OF CAMEROON Paix-Travail-Patrie Peace-Work-Fatherland ----------- ----------- OBSERVATOIRE NATIONAL SUR NATIONAL OBSERVATORY LES CHANGEMENTS CLIMATIQUES ON CLIMATE CHANGE ----------------- ----------------- DIRECTION GENERALE DIRECTORATE GENERAL ----------------- ----------------- ONACC www.onacc.cm; [email protected]; Tel : (+237) 693 370 504 / 654 392 529 BULLETIN N° 82 Forecasts and Dekadal Climate Alerts for the Period 1st to 10th June 2021 st 1 June 2021 © NOCC June 2021, all rights reserved Supervision Prof. Dr. Eng. AMOUGOU Joseph Armathé, Director General, National Observatory on Climate Change (NOCC) and Lecturer in the Department of Geography at the University of Yaounde I, Cameroon. Eng. FORGHAB Patrick MBOMBA, Deputy Director General, National Observatory on Climate Change (NOCC). Production Team (NOCC) Prof. Dr. Eng. AMOUGOU Joseph Armathé, Director General, National Observatory on Climate Change (NOCC) and Lecturer in the Department of Geography at the University of Yaounde I, Cameroon. Eng. FORGHAB Patrick MBOMBA, Deputy Director General, National Observatory on Climate Change (NOCC). BATHA Romain Armand Soleil, PhD student and Technical staff, NOCC. ZOUH TEM Isabella, M.Sc. in GIS-Environment and Technical staff, NOCC. NDJELA MBEIH Gaston Evarice, M.Sc. in Economics and Environmental Management. MEYONG René Ramsès, M.Sc. in Physical Geography (Climatology/Biogeography). ANYE Victorine Ambo, Administrative staff, NOCC. ELONG Julien Aymar, M.Sc. in Business and Environmental law. I. Introduction -

Gastro-Intestinal Helminths of Goliath Frogs
Global Ecology and Conservation 4 (2015) 146–149 Contents lists available at ScienceDirect Global Ecology and Conservation journal homepage: www.elsevier.com/locate/gecco Original research article Gastro-intestinal helminths of goliath frogs (Conraua goliath) from the localities of Loum, Yabassi and Nkondjock in the Littoral Region of Cameroon Nguiffo Nguete Daniel, Wabo Pone Josue ∗, Mpoame Mbida Laboratory of Biology and Applied Ecology, Department of Animal Biology, Faculty of Science, University of Dschang, PO Box 067 Dschang, Cameroon article info a b s t r a c t Article history: The gastro-intestinal helminth parasites of goliath frog (Conraua goliath) from the Littoral Received 10 June 2015 Region of Cameroon in the Localities of Loum, Yabassi and Nkondjock were surveyed. Out Received in revised form 26 June 2015 of the 30 goliath frogs examined (13 males and 17 females) between April and May 2013, Accepted 30 June 2015 26 (85%) contained at least one helminth parasite and yielded a total of nine hundred and Available online 7 July 2015 seventy three (973) helminths comprising: Nematodes (90.5%), Trematodes (9.4%) and Pen- tastomids (0.1%). Nematodes included: Africana taylori (60%), Oswaldocruzia perreti (0.2%), Keywords: Aplectana sp. (21%), Gendria sp. (7.1%), Amphibiophilus sp. (0.2%), Strongyluris sp. (0.1%), Gastro-intestinal helminths Conraua goliath Physalopteroides sp. (1.6%), and Oxyuridae gen. sp. (0.3%). Trematodes comprised: Meso- Species richness coelium sp. (7.3%) and Diplodiscus subclavatus (2.1%). Pentastomids were represented by Diversity Sebekia sp. (0.1%). The mean species richness and diversity were 1:97±2:12 and 0:41±0:04 Cameroon respectively. -
Programmation De La Passation Et De L'exécution Des Marchés Publics
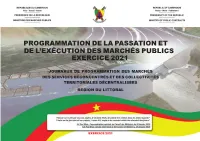
PROGRAMMATION DE LA PASSATION ET DE L’EXÉCUTION DES MARCHÉS PUBLICS EXERCICE 2021 JOURNAUX DE PROGRAMMATION DES MARCHÉS DES SERVICES DÉCONCENTRÉS ET DES COLLECTIVITÉS TERRITORIALES DÉCENTRALISÉES RÉGION DU LITTORAL EXERCICE 2021 SYNTHESE DES DONNEES SUR LA BASE DES INFORMATIONS RECUEILLIES Nbre de N° Désignation des MO/MOD Montant des Marchés N° page Marchés 1 Services déconcentrés Régionaux 11 476 050 000 3 2 Communauté Urbaine de Nkongsamba 143 49 894 418 496 4 3 Communauté Urbaine de Nkongsamba 1 125 000 000 16 Département du Moungo 4 Services déconcentrés départementaux 2 38 000 000 17 5 Commune de BARE BAKEM 9 312 790 000 17 6 Commune de BONALEA 24 412 000 000 17 7 Commune de DIBOMBARI 11 273 300 000 19 8 Commune de LOUM 8 186 600 000 20 9 Commune de MANJO 8 374 700 000 21 10 Commune de MBANGA 9 222 600 000 21 11 Commune de MELONG 13 293 140 184 22 12 Commune de NJOMBE PENJA 5 221 710 000 23 13 Commune d'EBONE 10 294 400 000 24 14 Commune de MOMBO 6 142 500 000 24 15 Commune de NKONGSAMBA I 11 245 833 000 25 16 Commune de NKONGSAMBA II 11 316 000 000 26 17 Commune de NKONGSAMBA III 6 278 550 000 27 TOTAL Département 133 3 612 123 184 Département du Nkam 18 Services déconcentrés départementaux 2 16 000 000 28 19 Commune de NDOBIAN 12 309 710 000 28 20 Commune de NKONDJOCK 8 377 000 000 29 21 Commune de YABASSI 21 510 500 000 29 22 Commune de YINGUI 11 241 000 000 31 TOTAL Département 54 1 454 210 000 Département de la Sanaga Maritime 23 Services déconcentrés départementaux 10 371 600 000 32 24 Commune de Dibamba 13 328 650 000 32 -

Research Into Small Scale Mining Formalization in Ghana
RESEARCH INTO SMALL S C A L E M I N I N G FORMALIZATION IN GHANA: CHANGING THE P A R A D I G M OF ILLEGAL GALAMSE DR. KINGSLEY ARKORFUL BAAH ACHEAMFOUR DINAH ARYEETEY SHEILA FREMPONG OSEI OWUSU Table of Contents Acknowledgment ........................................................................................................................................................... 2 Executive Summary ....................................................................................................................................................... 3 1. Introduction ............................................................................................................................................................ 6 1. Background of Research and Context ............................................................................................................. 6 2. Rationale for Mining Research .............................................................................................................................. 6 3. Objectives of the Research ..................................................................................................................................... 8 4. Methodology and Methods .................................................................................................................................... 9 1. Research Setting .............................................................................................................................................. 9 2. Research Methods and -

Drying Kinetics of Cassava Chips
Journal of Health, Medicine and Nursing www.iiste.org ISSN 2422-8419 An International Peer-reviewed Journal Vol.81, 2020 Factors Associated with Low Immunization Coverage in Children Under Five Years in Asuogyaman District in Eastern Region of Ghana Solomon Antwi Brefo1* Abdul Aziz Abdulai2 Cyril Azornu Kwami1 Jonathan Mawutor Gmanyami1 Emmanuel Senyo Kasu1,3 1.School of Public Health, University of Health and Allied Sciences, Ho, Volta Region, Ghana 2.District Health Directorate, Ghana Health Service, Asuogyaman District, Eastern Region 3.Public Health Department, Ho Teaching Hospital, Ho, Volta Region Abstract Expanded Programme on Immunization is one of the most successful and cost effective programmes adopted by World Health Organization and other partners to prevent vaccine preventable diseases which are the major cause of infant morbidity and mortality worldwide. Since 2012, Africa has demonstrated unprecedented commitments in the Global Vaccine Action Plan and this has resulted in the protection of millions of children. Despite this, some infants still remained unvaccinated and at risk of vaccine preventable diseases. Even though, Ghana was among countries which achieved 95% DPT3 coverage, this was not evenly distributed across all districts and Asuogyaman District was not an exception. The study assessed the factors associated with low immunization coverage among children under five years in Asuogyaman District. A descriptive cross-sectional study was conducted among mothers/caregivers in the Asuogyaman district. A total of 401 mothers/caregivers were enrolled into the study and structured questionnaire was used to collected data from mothers/caregivers on factors associated with low immunization coverage in children under 5 years. -

Open Whole.Kad.Final3re.Pdf
The Pennsylvania State University The Graduate School College of Earth and Mineral Sciences MANAGING WATER RESOURCES UNDER CLIMATE VARIABILITY AND CHANGE: PERSPECTIVES OF COMMUNITIES IN THE AFRAM PLAINS, GHANA A Thesis in Geography by Kathleen Ann Dietrich © 2008 Kathleen Ann Dietrich Submitted in Partial Fulfillment of the Requirements for the Degree of Master of Science August 2008 The thesis of Kathleen Ann Dietrich was reviewed and approved* by the following: Petra Tschakert Assistant Professor of Geography Alliance for Earth Sciences, Engineering, and Development in Africa Thesis Adviser C. Gregory Knight Professor of Geography Karl Zimmerer Professor of Geography Head of the Department of Geography *Signatures are on file in the Graduate School iii ABSTRACT Climate variability and change alter the amount and timing of water resources available for rural communities in the Afram Plains district, Ghana. Given the fact that the district has been experiencing a historical and multi-scalar economic and political neglect, its communities face a particular vulnerability for accessing current and future water resources. Therefore, these communities must adapt their water management strategies to both future climate change and the socio-economic context. Using participatory methods and interviews, I explore the success of past and present water management strategies by three communities in the Afram Plains in order to establish potentially effective responses to future climate change. Currently, few strategies are linked to climate variability and change; however, the methods and results assist in giving voice to the participant communities by recognizing, sharing, and validating their experiences of multiple climatic and non-climatic vulnerabilities and the past, current, and future strategies which may enhance their adaptive capacity. -

Proceedingsnord of the GENERAL CONFERENCE of LOCAL COUNCILS
REPUBLIC OF CAMEROON REPUBLIQUE DU CAMEROUN Peace - Work - Fatherland Paix - Travail - Patrie ------------------------- ------------------------- MINISTRY OF DECENTRALIZATION MINISTERE DE LA DECENTRALISATION AND LOCAL DEVELOPMENT ET DU DEVELOPPEMENT LOCAL Extrême PROCEEDINGSNord OF THE GENERAL CONFERENCE OF LOCAL COUNCILS Nord Theme: Deepening Decentralization: A New Face for Local Councils in Cameroon Adamaoua Nord-Ouest Yaounde Conference Centre, 6 and 7 February 2019 Sud- Ouest Ouest Centre Littoral Est Sud Published in July 2019 For any information on the General Conference on Local Councils - 2019 edition - or to obtain copies of this publication, please contact: Ministry of Decentralization and Local Development (MINDDEVEL) Website: www.minddevel.gov.cm Facebook: Ministère-de-la-Décentralisation-et-du-Développement-Local Twitter: @minddevelcamer.1 Reviewed by: MINDDEVEL/PRADEC-GIZ These proceedings have been published with the assistance of the German Federal Ministry for Economic Cooperation and Development (BMZ) through the Deutsche Gesellschaft für internationale Zusammenarbeit (GIZ) GmbH in the framework of the Support programme for municipal development (PROMUD). GIZ does not necessarily share the opinions expressed in this publication. The Ministry of Decentralisation and Local Development (MINDDEVEL) is fully responsible for this content. Contents Contents Foreword ..............................................................................................................................................................................5 -

Public Procurement Authority. Draft Entity Categorization List
PUBLIC PROCUREMENT AUTHORITY. DRAFT ENTITY CATEGORIZATION LIST A Special Constitutional Bodies Bank of Ghana Council of State Judicial Service Parliament B Independent Constitutional Bodies Commission on Human Rights and Administrative Justice Electoral Commission Ghana Audit Service Lands Commission Local Government Service Secretariat National Commission for Civic Education National Development Planning Commission National Media Commission Office of the Head of Civil Service Public Service Commission Veterans Association of Ghana Ministries Ministry for the Interior Ministry of Chieftaincy and Traditional Affairs Ministry of Communications Ministry of Defence Ministry of Education Ministry of Employment and Labour Relations Ministry of Environment, Science, Technology and Innovation Ministry of Finance Ministry Of Fisheries And Aquaculture Development Ministry of Food & Agriculture Ministry Of Foreign Affairs And Regional Integration Ministry of Gender, Children and Social protection Ministry of Health Ministry of Justice & Attorney General Ministry of Lands and Natural Resources Ministry of Local Government and Rural Development Ministry of Petroleum Ministry of Power PUBLIC PROCUREMENT AUTHORITY. DRAFT ENTITY CATEGORIZATION LIST Ministry of Roads and Highways Ministry of Tourism, Culture and Creative Arts Ministry of Trade and Industry Ministry of Transport Ministry of Water Resources, Works & Housing Ministry Of Youth And Sports Office of the President Office of President Regional Co-ordinating Council Ashanti - Regional Co-ordinating -

RC205.F76 Blthr C.L G365710
University of Ghana http://ugspace.ug.edu.gh RC205.F76 blthr C.l G365710 The Balme Llbran/ University of Ghana http://ugspace.ug.edu.gh UNIVERSITY OF GHANA SCHOOL OF PUBLIC HEALTH CONTROL OF YAWS IN THE ASUOGYAMAN DISTRICT. CAN COMMUNITY INVOLVEMENT MAKE THE DIFFERENCE? A DISSERTATION SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENT FOR THE AWARD OF MASTER OF PUBLIC HEALTH (MPH) DEGREE OF THE UNIVERSITY OF GHANA. BY DR. ABUDULAI ADAMS FORGOR ACADEMIC SUPERVISORS: PROF. F. K. WURAPA DR. J. GYAPONG FIELD SUPERVISOR: MRS GRACE NKRUMAH-MILLS AUGUST, 2001 University of Ghana http://ugspace.ug.edu.gh DECLARATION This dissertation is the result of independent investigation. Where my work is indebted to the work of others, I have made acknowledgement. I declare that, it has neither been accepted in substance for any other degree nor is it concurrently being submitted in candidature for any other degree. Dr. AbucMahMa^Forgor ACADEMIC SUPERVISORS: PROF. F.K. WURAPA DR. J. GYAPONG University of Ghana http://ugspace.ug.edu.gh DEDICATION This piece of work is dedicated to my only daughter Gifty Adjara Forgor who escaped death on 5th December 2000. University of Ghana http://ugspace.ug.edu.gh ACKNOWLEDGEMENT I wish to thank my academic supervisors Prof. F. K. Wurapa and Dr. Gyapong for all the support, advice and direction given me during this study. Without them this study not have been what it is. My sincere thanks go to Prof. F. Binka for his enormous technical and moral support given me during the course of this study. I wish to thank my field supervisor Mrs.