Research Compilation 2016 – 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

United States Arctic Weather Station Programme
JOINT ARCTIC WEATHER STATIONS FIVE YEAR REPORT 1946-1951 JOINT CANADIAN -UNITED STATES ARCTIC WEATHER STATION PROGRAMME A REVIEW OF THE ESTABLISHMENT AND OPERATION OF THE JOINT ARCTIC WEATHER STATIONS AT EUREKA, RESOLUTE, ISACHSEN, MOULD BAY, AND ALERT AND A SUMMARY OF THE SCIENTIFIC ACTIVITIES AT THESE STATIONS 1946-1951 Compiled by METEOROLOGICAL DIVISION - DEPARTMENT OF TRANSPORT - CANADA and U.S. WEATHER BUREAU - DEPARTMENT OF COMMERCE – UNITED STATES CONTENTS CHAPTER PAGE 1. Introduction 1 2. Establishment of Stations 8 Eureka 8 Resolute 10 Isachsen 12 Mould Bay 14 Alert 15 Reconnaissance of Bridport Inlet 16 3. Station Maintenance 20 4. Methods of Re-supply 27 Summer Sea Supply Mission 27 Problems of Ice Navigation 29 Airlift Operations 35 5. Personnel 37 6. Meteorological Programme 42 Surface Observations 42 Upper Air Observations 46 7. Special Scientific Projects by Weather Station Personnel 48 Low Level Air Temperature Measurements 48 Permafrost Drilling and Soil Temperature Measurements at Resolute 49 Tidal Observations 59 Ice Thickness Measurements 61 Sea Ice Reports 63 Ice and Sea Water Temperatures 75 Lake Water Temperatures at Resolute 76 Observations of Arctic Snow Characteristics 77 Snow Crystal Replicas 81 Arctic Test of U.S. Navy Model, TDM-l, Automatic Weather Station 82 Salinity of Sea Water 85 Atmospheric Refraction 86 Solar Radiation 87 8. Stations Established at Resolute in Addition to the Weather Station 89 --ii-- CHAPTER PAGE Resolute Magnetic Observatory 89 Resolute Seismograph Station 90 Resolute Ionospheric Station 91 9. Arctic Buildings 92 Foundations 92 Prefabricated Buildings 95 Experimental Hut at Alert, N.W.T. 99 10. Projects by Transient Scientific Personnel 100 Wildlife Survey of Slidre Fiord Area 101 National Museum of Canada Investigations 101 Geological Survey - Cornwallis Island 104 Northern Insect Survey Investigations 109 Northern Insect Survey at Resolute, N.W.T.-1949 110 Northern Insect Survey at Alert, N.W.T.-l95l 114 Geographical Investigations at Eureka, N.W.T. -

Carex Concinna
Draft Carex concinna Draft Conservation Assessment For Carex concinna R. Brown (low northern sedge or beauty sedge) USDA Forest Service, Eastern Region Hiawatha National Forest January 2004 Draft Carex concinna This Conservation Assessment was prepared to compile the published and unpublished information on Carex concinna R. Brown; This report provides information to serve as a Conservation Assessment for the Eastern Region of the Forest Service. It is an administrative study only and does not represent a management decision by the U.S. Forest Service. Although the best scientific information available was used and subject experts were consulted in preparation of this document and its review, it is expected that new information will arise. In the spirit of continuous learning and adaptive management, if the reader has any information that will assist in conserving this species, please contact the Eastern Region of the Forest Service – Threatened and Endangered Species Program at 310 Wisconsin Avenue, Suite 580 Milwaukee, Wisconsin 53203. ii Draft Carex concinna This document is undergoing peer review, comments welcome iii Draft Carex concinna Table of Contents Acknowledgements …………………………………. 1 Introduction/Objectives ……………..….…………… 2 Executive Summary …………………………………. 2 Nomenclature and Taxonomy ……………………….. 3 Species Description …………………………………. 3 Geographic Distribution ……………………………. 4 Habitat and Ecology ………………………………… 5 Rangewide Protection Status ………………………. 7 Life History …………………………………………. 9 Population Viability ……………………..…………. 10 Potential -

April 1, 1999 Nunavut Becomes a Separate Territory
April 1, 1999 Nunavut Becomes a Separate Territory Nunavut is one of the territories of the Dominion of Canada. It is located in the far north and is considered to be part of the Arctic region. It has long, cold winters and short, cool summers. Nunavut makes up about one-fifth of the land area of Canada and is an important source of natural resources including diamonds, copper, gold, silver, and uranium. It is made up of rocky, treeless areas, and a lot of the ground is permanently frozen. There are large areas of Nunavut that are protected areas, including five national parks that attract the more adventurous visitors. Others are attracted to the exploring, fishing, hunting, and other outdoor activities. Look at the map of Nunavut below. Label the capital of Nunavut. Locate the towns of Eureka, Alert, Resolute, Qikiqtarjuaq, Kimmirut, Cape Dorset, Arviat, Kuglugtuk, and Carmacks, and label them on the map. Now label the United States Range and Mount Barbeau. Also, locate the Back River, Thelon River, Contwoyto Lake, Garry Lake, Yathkyed Lake, Kasba Lake, and Neultin Lake, and label them. Now, label Foxe Channel, Foxe Basin, Queen Maud Gulf, Gulf of Boothia, Nansen Sound, Coronation Gulf, M’Clintock Channel, Jones Sound, Parry Channel, and Lancaster Sound. Lastly, label the provinces, territories, states, or major bodies of water that border Nunavut. When you have finished, move on to the timeline of Nunavut history on the next page and the research prompts that follow. ©2018 Bonnie Rose Hudson WriteBonnieRose.com Timeline of Nunavut History Answer Key c. 1000 1576 1670 1771 1847 1876 1880 1930 1950 1955 1979 1982 1988 1992 1993 1999 2001 2003 2014 2015 ©2018 Bonnie Rose Hudson WriteBonnieRose.com 1. -
POL Volume 2 Issue 16 Back Matter
THE POLAR RECORD INDEX NUMBERS 9—16 JANUARY 1935—JULY 1938 PRINTED IN GREAT BRITAIN FOR THE SCOTT POLAR RESEARCH INSTITUTE CAMBRIDGE: AT THE UNIVERSITY PRESS 1939 THE POLAR RECORD INDEX Nos. 9-16 JANUARY 1935—JULY 1938 The names of ships are in italics. Expedition titles are listed separately at Uie end Aagaard, Bjarne, II. 112 Alazei Mountains, 15. 5 Abruzzi, Duke of, 15. 2 Alazei Plateau, 12. 125 Adams, Cdr. .1. B., 9. 72 Alazei River, 14. 95, 15. 6 Adams, M. B., 16. 71 Albert I Peninsula, 13. 22 Adderley, J. A., 16. 97 Albert Harbour, 14. 136 Adelaer, Cape, 11. 32 Alberta, 9. 50 Adelaide Island, 11. 99, 12. 102, 103, 13. Aldan, 11. 7 84, 14. 147 Aldinger, Dr H., 12. 138 Adelaide Peninsula, 14. 139 Alert, 11. 3 Admiralty Inlet, 13. 49, 14. 134, 15. 38 Aleutian Islands, 9. 40-47, 11. 71, 12. Advent Bay, 10. 81, 82, 11. 18, 13. 21, 128, 13. 52, 53, 14. 173, 15. 49, 16. 15. 4, 16. 79, 81 118 Adytcha, River, 14. 109 Aleutian Mountains, 13. 53 Aegyr, 13. 30 Alexander, Cape, 11. GO, 15. 40 Aerial Surveys, see Flights Alexander I Land, 12. 103, KM, 13. 85, Aerodrome Bay, II. 59 80, 14. 147, 1-19-152 Aeroplanes, 9. 20-30, 04, (i5-(>8, 10. 102, Alcxamtrov, —, 13. 13 II. 60, 75, 79, 101, 12. 15«, 158, 13. Alexcyev, A. D., 9. 15, 14. 102, 15. Ki, 88, 14. 142, 158-103, 16. 92, 93, 94, 16. 92,93, see also unilcr Flights Alftiimyri, 15. -
Lynx Conservation Assessment and Strategy
Canada Lynx Conservation Assessment and Strategy 3rd Edition — August 2013 http://www.fs.fed.us/biology/resources/pubs/wildlife/index.html Acknowledgments We would like to thank the interagency Steering Committee, chaired first by Kathy McAllister and later by Jane Cottrell of the USDA Forest Service, Northern Region, for guidance and support. The Science Team published the foundational scientific assessment, “Ecology and Conservation of Lynx in the Unit- ed States” (Ruggiero et al. 2000a) and provided invaluable assistance and advice to the Lynx Biology Team. Even after the Science Team completed its assignment and was dissolved, several of its members continued to give gen- erously of their time and expertise. We are indebted to John Squires, Rocky Mountain Research Station, USDA Forest Service, for sharing information and insights from his research on lynx. John contributed directly to this revision of the LCAS by administering the contract to update the conservation assessment, providing review and comment on early drafts, and arranging and administering a formal peer review of this document. We would like to acknowledge the important contributions by Ben Maletzke and Jennifer Burghardt-Dowd. Under the contract administered by the Rocky Mountain Research Station, they compiled relevant new scientific literature produced from 2000 to 2010 and proposed new text that would incorporate the new information on the ecology of lynx and snowshoe hare into the lynx assessment. We would like to acknowledge Eric Odell of Colorado Parks and Wildlife for his participation and contributions throughout the revision of this document, particularly the update of information concerning the Southern Rocky Mountains Geographic Area. -
Canadian Cancer Statistics a 2018 Special Report on Cancer Incidence by Stage
Canadian Cancer Statistics A 2018 special report on cancer incidence by stage Produced by the Canadian Cancer Society, Statistics Canada, the Public Health Agency of Canada, in collaboration with the provincial and territorial cancer registries cancer.ca/statistics Citation Material appearing in this publication may be reproduced or copied without permission. The following citation is recommended: Canadian Cancer Statistics Advisory Committee. Canadian Cancer Statistics 2018. Toronto, ON: Canadian Cancer Society; 2018. Available at: cancer.ca/Canadian-Cancer-Statistics-2018-EN.pdf (accessed [date]). June 2018 ISSN 0835-2976 This publication is available in English and French on the Canadian Cancer Society’s website at cancer.ca/statistics. Visit the website for the most up-to-date version of this publication and additional resources, such as individual figures from the publication and an archive of previous editions. The development of this publication over the years has benefited considerably from the comments and suggestions of readers. The Advisory Committee appreciates and welcomes such comments. To offer ideas on how the publication can be improved or to be notified about next year’s publication, complete the evaluation form or email [email protected]. Canadian Cancer Society n Canadian Cancer Statistics: A 2018 special report 2 Members of the Canadian Cancer Statistics Advisory Committee Leah Smith, PhD (Chair) Donna Turner, PhD Canadian Cancer Society, Toronto, Ontario CancerCare Manitoba, Winnipeg, Manitoba Shirley Bryan, PhD Hannah -

Glaciers in the Arctic 79
GLACIERSIN THE ARCTIC’ Robert P. Sharp* LACIERS are an important element of the arctic and subarctic environment. They strongly influence meteorological and climatological conditions andGhave local economic significance. Glaciers are delicately responsive to subtle climatological changes, and their behaviour provides a useful means of recognizing the nature and scale of these changes depending upon the degree to which the influence of the various glaciometeorological elements is under- stood (Wallkn, 1948; Hubley, 1954; Orvig, 1954). Useful data on mean annual temperatures in remote regions can be obtained from measurement of thermal regimen in polar glaciers (Ahlmann, 1953, p. 3). Academically, study of arctic glaciers will be especially valuable if Ahlmann (1953, p. 5) is right in supposing that the great Pleistocene ice-sheets were essentially polar in behaviour and temperature regimen. Recent interest in the nature and origin of “ice islands” inthe Arctic pack(Fletcher, 1950; Koenig et ai, 1952; Crary, Cotell, and Sexton, 1952; Montgomery, 1952; Crary, 1954; Debenham, 1954) demonstrates the need for study of arctic glaciers for practical and strategic reasons. The size, nature, and distribution of arctic and subarctic glaciers are treated descriptively in this compilation, which is necessarily based largely on the writings and observations of others. Essentially nothing offered is new or original, and, in spite of references sprinkled liberally through the text, it is not possible to acknowledge every word or thought. Recent air photographs will certainly result in modifications of the material presented. This compilation was prepared in 1949 for the EncyclopediaArctica, a project of the Stefansson Library supported by the Office of Naval Research. -

The Establishment of Alert, N.W.T., Canada J
ARCTIC VOL. 43, NO. 1 (MARCH 1990) P. 21-34 The Establishment of Alert, N.W.T., Canada J. PETER JOHNSON, JR.' (Received 18 February 1982;accepted in revised form 23 June 1989) ABSTRACT. The Joint Arctic WeatherStations of Canada and the United States were built in the Queen ElizabethIslands of northern Canada. The Eureka and Resolute stations were established in 1947 and another two, Mould Bay and Isachsen, in1948. In the summer of 1948 the US. icebreakers Edisto and Eastwind reached DumbbellBay on the north coast of Ellesmere Island,where a cache wasdeposited for a fifth Canadian station, Alert. This station was established by air from Thule in April 1950. Unlike earlier satellite stations, the eight regular station personnel were supplemented by four extra men to aid in construction of the buildings and a gravel airstrip. During the spring a message leftat Cape Sheridan by Peary in1907 was found and evidence, including an unreported marker, of the 1875-76 British Admiralty Expedition was discovered. Equipment failuresand supply problems later on caused construction delays, whichwere relieved by air drops. One of these led tothe crash of an RCAF Lancaster and the death of all aboard. An RCAFCanso sent to investigate was damaged during anattempted takeoff but was repaired when theEastwind arrived with support and badly needed equipment. Completion of the station proceeded rapidly after this, and it becameoperational in September1950. As an important Cold War listening post on the northern rim of the continent, its population of specialists grew to more than 200. Key words: Alert, N.W.T., Joint Arctic Weather Stations, Ellesmere Island, Cold War RÉSUMÉ. -

School Supply Retailer Gives Purolator an A+ for Its Canadian Returns Solution
CASE STUDY School Supply Retailer Gives Purolator an A+ for Its Canadian Returns Solution It was hardly surprising when school districts across The one weak link in this well-executed supply chain, Canada jumped at the chance to purchase all of especially with regard to its Canadian operations, their supplies — everything from pencils and paper has been its inability to process returns. to desks, janitorial supplies, technology hardware, and playground equipment — at a reduced cost Like many retailers, this company tended to view from a single supplier. After all, two things all school returns as a necessary cost of doing business and districts seem to have in common are increasingly never gave much thought to an actual returns tight budgets and not enough hours in the day to strategy. Instead, customer credits would be issued, accomplish everything that needs to get done. or replacement items provided, while returns essentially accumulated in a warehouse. This Wisconsin-based retailer was seemingly ahead of its time when it first rolled out the concept of a But with product returns accounting for as much “one-stop” supply solution almost 60 years ago. as ten percent of revenue, it was clear that this At the time, the company relied on catalogs, word “out of sight, out of mind” strategy was not of mouth, and a hardworking sales force to build sustainable. Company managers had implemented relationships with schools, colleges and universities, a process for addressing returns within the United community centers, and other facilities. Customers States and now sought to develop a similar strategy would place orders for most everything they needed for their Canadian returns. -

Interannual Trends in the Radiation Climatology of the Canadian High Arctic
INTERANNUAL TRENDS IN THE RADIATION CLIMATOLOGY OF THE CANADIAN HIGH ARCTIC Scott Thomas Weston B.Sc., Simon Fraser University, 2004 THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE In the Department of Geography 0 Scott Weston 2006 SIMON FRASER UNIVERSITY Spring 2006 All rights reserved. This work may not be reproduced in whole or in part, by photocopy or other means, without permission of the author. APPROVAL Name: Scott Thomas Weston Degree: Master of Science Title of Thesis: INTERANNUAL TRENDS IN THE RADIATION CLIMATOLOGY OF THE CANADIAN HIGH ARCTIC Examining Committee: Chair: Dr. S. Dragicevic Assistant Professor Dr. 0. Hertman acting for the late Dr. W.G. Bailey Sessional Instructor Senior Supervisor Geography Dept., SFU Professor, Geography Dept. Dr. A.M. Sawchuk, University College Professor Kwantlen University College Dr. L.J.B. McArthur, Chief, Air Quality Research Branch, Experimental Studies Division, Meteorological Service of Canada, Environment Canada Dr. I.G. McKendry, Professor Department of Geography and Atmospheric Sciences, University of British Columbia External Examiner Date Approved: March 24, 2006 IEI SIMON FRASER 0@ UNlVERSlTYl ibrary DECLARATION OF PARTIAL COPYRIGHT LICENCE The author, whose copyright is declared on the title page of this work, has granted to Simon Fraser University the right to lend this thesis, project or extended essay to users of the Simon Fraser University Library, and to make partial or single copies only for such users or in response to a request from the library of any other university, or other educational institution, on its own behalf or for one of its users. -

The Polar Record 10
THE POLAU UECORD NUM BER 10 : J ULY 1985 PRINTED IN GREAT BR ITA IN FOR THE SCOTT POLAR RESEARCH INSTI TUTE CAMBRIDGE: AT THE UNI VERS ITY PR ESS 19 85 P riee Two Shillings CO NTE NTS Dr J .-B. CHARCOT FrontUpieu F OREWORD• page " A RCTIC REGIONS: S valbard, Franz J osef Land, and llussian Arctic Regions , Soviet Union E xpeditions, 1985 . 76 Geological Expediti on 10 the Chukchis Peninsular, 193-i-85 • 77 Soviet Union Expeditions, 1984 . 78 Soviet Union Research Stations . 78 Soviet Investigat ions in Anadyr and t he Chukchis Peninsule, 1931 -84: 80 Norwegian Spitsbcrgen Expeditions. 1935 80 Norwegian-Swed.ish Spitsbergcn Expedit ion, 1934 81 Oxford Uni versity Arctie Expedit ion, 1935-36 82 PoJish Expedit ion 10 Spitsbergen, 193-& 88 ARTICLE : Explorat ion of the Interior of North East Land. By K. S. Sandford . 84 Greenland and J an Mayen : The Seientific Results of the Germa n Greenland Expedit ion Alfred Wegener, 1929 and 1930-81 90 Dr Charcot's East Greenland Croise, 1935 91 Norwegian Expeditions ta Greenland, 1935 91 Danish Oceanographieal Work in t he Greenland Seas, 1935 . 91 Danish Archaeological R eseareh in Greenland, 1935 92 Brit ish Expedition to East Greenland, 1985-36 . 92 Professer Ste inbOck's Research in West Greenland, 1935 98 l talian )Iountaineering Expedition to Scoresby Sound, East Grœnland, ] 934 98 :!tleteor Expedition, 1934 95 Other Work in Greenland 95 l celand: Icelendic Expedition to Vat naj ôkull, 1935 91 Mr Tryggvi Magmisson's E xpedition to Langjôkull, 1985 97 Ot her Expedit ions in Iceland 98 (Continued lm page 3 ofwrapper) Pages Directo r Secretary-General __~-'- _ 2:l_:jjif':r >' / Assistant-8ecretary Technicai-Assistant -A--d~-X-~- Techn icaI-Assistant ~~~~_. -
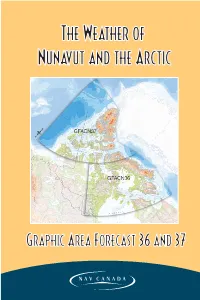
The Weather of Nunavut and the Arctic
NUNAVUT-E 11/12/05 10:34 PM Page 3 TheThe WeatWeathherer ofof NunavutNunavut andand thethe ArcticArctic GraphicGraphic AArearea FForecastorecast 3366 aandnd 3377 NUNAVUT-E 11/12/05 10:34 PM Page i TheThe WeatWeatherher ofof NunNunavavutut andand tthehe AArcticrctic GraphicGraphic AArearea FForecastorecast 3636 aandnd 3377 by Ed Hudson David Aihoshi Tim Gaines Gilles Simard John Mullock NUNAVUT-E 11/12/05 10:34 PM Page ii Copyright Copyright © 2001 NAV CANADA. All rights reserved. No part of this document may be reproduced in any form, including photocopying or transmission electronically to any computer, without prior written consent of NAV CANADA. The information contained in this document is confidential and proprietary to NAV CANADA and may not be used or disclosed except as expressly authorized in writing by NAV CANADA. Trademarks Product names mentioned in this document may be trademarks or registered trademarks of their respective companies and are hereby acknowledged. Relief Maps Copyright © 2000. Government of Canada with permission from Natural Resources Canada Design and illustration by Ideas in Motion Kelowna, British Columbia ph: (250) 717-5937 [email protected] NUNAVUT-E 11/12/05 10:34 PM Page iii LAKP-Nunavut and the Arctic iii Preface For NAV CANADA’s Flight Service Specialists (FSS), providing weather briefings to help pilots navigate through the day-to-day fluctuations in the weather is a critical role. While available weather products are becoming increasingly more sophisticated and at the same time more easily understood, an understanding of local and regional climatological patterns is essential to the effective performance of this role.