Original Article
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Confocal Microscopy in Cornea Guttata and Fuchs' Endothelial Dystrophy
Br J Ophthalmol 1999;83:185–189 185 Confocal microscopy in cornea guttata and Fuchs’ Br J Ophthalmol: first published as 10.1136/bjo.83.2.185 on 1 February 1999. Downloaded from endothelial dystrophy Auguste G-Y Chiou, Stephen C Kaufman, Roger W Beuerman, Toshihiko Ohta, Hisham Soliman, Herbert E Kaufman Abstract conventional imaging methods.3–13 Because of Aims—To report the appearances of cor- its ability to focus the light source and the nea guttata and Fuchs’ endothelial dystro- image on the same focal plane, it allows real phy from white light confocal microscopy. time in vivo assessment of the diVerent layers Methods—Seven eyes of four consecutive of the cornea, including the endothelial layer. patients with cornea guttata were pro- Therefore, it may be an alternative method in spectively examined. Of the seven eyes, evaluating cornea guttata or Fuchs’ endothelial three also had corneal oedema (Fuchs’ dystrophy. dystrophy). In vivo white light tandem In the current study, we analysed the scanning confocal microscopy was per- appearances of cornea guttata and Fuchs’ dys- formed in all eyes. Results were compared trophy from confocal microscopy and compare with non-contact specular microscopy. the technique with non-contact specular mi- Results—Specular microscopy was pre- croscopy. cluded by corneal oedema in one eye. In the remaining six eyes, it demonstrated typical changes including pleomorphism, polymegathism, and the presence of gut- tae appearing as dark bodies, some with a central bright reflex. In all seven eyes, confocal microscopy revealed the pres- ence of round hyporeflective images with an occasional central highlight at the level of the endothelium. -

Curvularia Keratitis*
09 Wilhelmus Final 11/9/01 11:17 AM Page 111 CURVULARIA KERATITIS* BY Kirk R. Wilhelmus, MD, MPH, AND Dan B. Jones, MD ABSTRACT Purpose: To determine the risk factors and clinical signs of Curvularia keratitis and to evaluate the management and out- come of this corneal phæohyphomycosis. Methods: We reviewed clinical and laboratory records from 1970 to 1999 to identify patients treated at our institution for culture-proven Curvularia keratitis. Descriptive statistics and regression models were used to identify variables associ- ated with the length of antifungal therapy and with visual outcome. In vitro susceptibilities were compared to the clini- cal results obtained with topical natamycin. Results: During the 30-year period, our laboratory isolated and identified Curvularia from 43 patients with keratitis, of whom 32 individuals were treated and followed up at our institute and whose data were analyzed. Trauma, usually with plants or dirt, was the risk factor in one half; and 69% occurred during the hot, humid summer months along the US Gulf Coast. Presenting signs varied from superficial, feathery infiltrates of the central cornea to suppurative ulceration of the peripheral cornea. A hypopyon was unusual, occurring in only 4 (12%) of the eyes but indicated a significantly (P = .01) increased risk of subsequent complications. The sensitivity of stained smears of corneal scrapings was 78%. Curvularia could be detected by a panfungal polymerase chain reaction. Fungi were detected on blood or chocolate agar at or before the time that growth occurred on Sabouraud agar or in brain-heart infusion in 83% of cases, although colonies appeared only on the fungal media from the remaining 4 sets of specimens. -

Review the Global Incidence and Diagnosis of Fungal Keratitis
Review The global incidence and diagnosis of fungal keratitis Lottie Brown, Astrid K Leck, Michael Gichangi, Matthew J Burton, David W Denning Fungal keratitis is a severe corneal infection that often results in blindness and eye loss. The disease is most prevalent Lancet Infect Dis 2020 in tropical and subtropical climates, and infected individuals are frequently young agricultural workers of low Published Online socioeconomic status. Early diagnosis and treatment can preserve vision. Here, we discuss the fungal keratitis October 22, 2020 diagnostic literature and estimate the global burden through a complete systematic literature review from January, 1946 https://doi.org/10.1016/ S1473-3099(20)30448-5 to July, 2019. An adapted GRADE score was used to evaluate incidence papers—116 studies provided the incidence of University of Manchester, fungal keratitis as a proportion of microbial keratitis and 18 provided the incidence in a defined population. We Manchester, UK (L Brown MSc, calculated a minimum annual incidence estimate of 1 051 787 cases (736 251–1 367 323), with the highest rates in Asia Prof D W Denning FRCP); and Africa. If all culture-negative cases are assumed to be fungal, the annual incidence would be 1 480 916 cases International Centre for Eye (1 036 641–1 925 191). In three case series, 8–11% of patients had to have the eye removed, which represents an annual Health, London School of Hygiene & Tropical Medicine, loss of 84 143–115 697 eyes. As fungal keratitis probably affects over a million people annually, an inexpensive, simple London, UK (A K Leck PhD, diagnostic method and affordable treatment are needed in every country. -

Topical Corticosteroids and Fungal Keratitis: a Review of the Literature and Case Series
Journal of Clinical Medicine Review Topical Corticosteroids and Fungal Keratitis: A Review of the Literature and Case Series Karl Anders Knutsson 1,*, Alfonso Iovieno 2,3, Stanislav Matuska 1, Luigi Fontana 2 and Paolo Rama 1 1 Cornea and Ocular Surface Unit, San Raffaele Scientific Institute, 20132 Milan, Italy; [email protected] (S.M.); [email protected] (P.R.) 2 Arcispedale Santa Maria Nuova—IRCCS, 42123 Reggio Emilia, Italy; [email protected] (A.I.); [email protected] (L.F.) 3 Department of Ophthalmology, University of British Columbia, Vancouver, BC V6T 1Z, Canada * Correspondence: [email protected] or [email protected]; Tel./Fax: +39-022-6432-648 Abstract: The management of fungal keratitis is complex since signs and symptoms are subtle and ocular inflammation is minimal in the preliminary stages of infection. Initial misdiagnosis of the condition and consequent management of inflammation with corticosteroids is a frequent occurrence. Topical steroid use is considered to be a principal factor for development of fungal keratitis. In this review, we assess the studies that have reported outcomes of fungal keratitis in patients receiving steroids prior to diagnosis. We also assess the possible rebound effect present when steroids are abruptly discontinued and the clinical characteristics of three patients in this particular clinical scenario. Previous reports and the three clinical descriptions presented suggest that in fungal keratitis, discontinuing topical steroids can induce worsening of clinical signs. In these cases, we recommend to slowly taper steroids and continue or commence appropriate antifungal therapy. Citation: Knutsson, K.A.; Iovieno, A.; Keywords: fungal keratitis; topical corticosteroids; topical steroids; rebound effect Matuska, S.; Fontana, L.; Rama, P. -

Fusarium Keratitis and Corneal Collagen Cross
FUSARIUM KERATITIS AND SURGERY REFRACTIVE CORNEAL COLLAGEN CROSS-LINKING BY MINAS CORONEO, AO, BSC(MED), MBBS, MSC SYD, MD, MS, UNSW, FRACS, FRANZCO; RAJESH FOGLA, DNB, FRCS(EDIN), MMED(OPHTH); WILLIAM B. TRATTLER, MD; ASHIYANA NARIANI, MD, MPH; COMPLEX CASE MANAGEMENT COMPLEX GARGI KHARE VORA, MD; AND ALAN N. CARLSON, MD CASE PRESENTATION A 42-year-old white man is referred to the Duke University Eye Center Cornea Service for a central corneal ulcer with a hypopyon in his right eye. The patient sustained the ocular injury while mowing the lawn, with debris getting into the eye while he was wearing contact lenses. He was diagnosed with culture-positive Fusarium species by the referring ophthalmologist and was treat- ed with oral voriconazole 200 mg twice daily and frequent topical natamycin 5% and voriconazole 10 mg/mL. The patient under- went epithelium-off corneal collagen cross-linking (CXL) approxi- Figure 1. Initial evaluation of the eye with a Fusarium corneal mately 4 weeks after diagnosis of the ulcer and was treated with infiltrate and hypopyon. a loteprednol steroid taper after the procedure. His condition subsequently progressed, with increasing eye pain, a nonhealing epithelial defect, and a worsening corneal infiltrate. Upon evaluation, the patient has a large corneal infiltrate with necrotic stroma, which is approaching the limbus, and a hypopyon (Figure 1). His UCVA measures 20/70-1. B-scan ultrasound of the right eye shows no evidence of posterior segment involvement. Reculturing of the corneal infiltrate is negative for bacteria, fungus, and Acanthamoeba. Confocal microscopy reveals no evidence of hyphae or cysts. -

Herpetic Corneal Infections
FocalPoints Clinical Modules for Ophthalmologists VOLUME XXVI, NUMBER 8 SEPTEMBER 2008 (MODULE 2 OF 3) Herpetic Corneal Infections Sonal S. Tuli, MD Reviewers and Contributing Editors Consultants George A. Stern, MD, Editor for Cornea & External Disease James Chodosh, MD, MPH Kristin M. Hammersmith, MD, Basic and Clinical Science Course Faculty, Section 8 Kirk R. Wilhelmus, MD, PhD Christie Morse, MD, Practicing Ophthalmologists Advisory Committee for Education Focal Points Editorial Review Board George A. Stern, MD, Missoula, MT Claiming CME Credit Editor in Chief, Cornea & External Disease Thomas L. Beardsley, MD, Asheville, NC Academy members: To claim Focal Points CME cred- Cataract its, visit the Academy web site and access CME Central (http://www.aao.org/education/cme) to view and print William S. Clifford, MD, Garden City, KS Glaucoma Surgery; Liaison for Practicing Ophthalmologists Advisory your Academy transcript and report CME credit you Committee for Education have earned. You can claim up to two AMA PRA Cate- gory 1 Credits™ per module. This will give you a maxi- Bradley S. Foster, MD, Springfield, MA Retina & Vitreous mum of 24 credits for the 2008 subscription year. CME credit may be claimed for up to three (3) years from Anil D. Patel, MD, Oklahoma City, OK date of issue. Non-Academy members: For assistance Neuro-Ophthalmology please send an e-mail to [email protected] or a Eric P. Purdy, MD, Fort Wayne, IN fax to (415) 561-8575. Oculoplastic, Lacrimal, & Orbital Surgery Steven I. Rosenfeld, MD, FACS, Delray Beach, FL Refractive Surgery, Optics & Refraction C. Gail Summers, MD, Minneapolis, MN Focal Points (ISSN 0891-8260) is published quarterly by the American Academy of Ophthalmology at 655 Beach St., San Francisco, CA 94109-1336. -

Infectious Keratitis: Short Answers
Q Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? A Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas Infectious keratitis: Short answers Pseudomonas corneal ulcer associated with CL wear Q Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? A Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? CL wear Infectious keratitis: Short answers Acanthamoeba keratitis associated with CL wear Q Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? CL wear What are the three main culprits in fungal keratitis? What is the topical antifungal of choice for each? Fusarium:fungus 1 Topical…natamycin Aspergillisfungus 2 and Candida:fungus 3 A Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? CL wear What are the three main culprits in fungal keratitis? What is the topical antifungal of choice for each? Candida: Topical…natamycin Aspergillis and Fusarium: Q Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? CL wear What are the three main culprits in fungal keratitis? -

Acanthamoeba, Fungal, and Bacterial Keratitis: a Comparison of Risk Factors and Clinical Features
Acanthamoeba, Fungal, and Bacterial Keratitis: A Comparison of Risk Factors and Clinical Features JEENA MASCARENHAS, PRAJNA LALITHA, N. VENKATESH PRAJNA, MUTHIAH SRINIVASAN, MANORANJAN DAS, SEAN S. D’SILVA, CATHERINE E. OLDENBURG, DURGA S. BORKAR, ELIZABETH J. ESTERBERG, THOMAS M. LIETMAN, AND JEREMY D. KEENAN PURPOSE: To determine risk factors and clinical signs acanthamoeba keratitis research has been conducted in that may differentiate between bacterial, fungal, and industrialized countries, acanthamoeba keratitis also acanthamoeba keratitis among patients presenting with occurs in developing countries, often in non–contact presumed infectious keratitis. lens–wearing individuals.6,7 DESIGN: Hospital-based cross-sectional study. Acanthamoeba keratitis is frequently misdiagnosed as METHODS: We examined the medical records of 115 herpetic or fungal keratitis, and is subsequently treated incor- patients with laboratory-proven bacterial keratitis, 115 rectly, which can lead to poor outcomes.8 Case series of acan- patients with laboratory-proven fungal keratitis, and thamoeba keratitis have identified several important clinical 115 patients with laboratory-proven acanthamoeba kera- signs, such as pseudodendrites, perineural infiltrates, and ring titis seen at Aravind Eye Hospital, Madurai, India, from infiltrates.9,10 However, we are unaware of any studies that 2006-2011. Risk factors and clinical features of the 3 have compared the clinical findings of acanthamoeba organisms were compared using multinomial logistic keratitis with those of bacterial and fungal keratitis. regression. Clinical signs can be especially useful for differentiating the RESULTS: Of 95 patients with bacterial keratitis, 103 cause of infectious keratitis when microbiological testing is patients with fungal keratitis, and 93 patients with acan- not available—which is frequently the case in developing thamoeba keratitis who had medical records available for countries. -

Ophthalmic Drugs
A Supplement to 22nd EDITION Randall Thomas, OD, MPH Patrick Vollmer, OD The Clinical Guide to Dr. Melton Ophthalmic[ [ Dr. Thomas Drugs Dispense as writ ten — no substit utions. Refills: unlimit ed. May 15, 2018 Dr. Vollmer Peer-to-peer advice to help boost your prescribing prowess. Supported by an unrestricted grant from Bausch + Lomb 001_dg0518_fc.indd 3 5/11/18 10:52 AM FROM THE AUTHORS DEAR OPTOMETRIC COLLEAGUES: Supported by an Welcome to the 2018 edition of our annual Clinical Guide to Ophthalmic unrestricted grant from Drugs. Herein, we provide updates on our collective clinical experiences and Bausch + Lomb heavily season them with pertinent excerpts from the literature. This guide is intended to bring solid, scientifically accurate and clinically relevant information to our optometric colleagues. If you want to understand CONTENTS how the three of us treat, and what factors led us to develop these methods, you’ll find it explained here. The methods and opinions represented are our own. We recognize that other doctors may use alternative approaches. That First-year Impressions ...........3 is true in all of health care. But this three-doctor writing team has logged over 75 combined years of clinical optometry, and we bring that ‘real-world’ spirit to the discussions that follow. Know that, above all, we are doctors who are genuinely concerned for our patients’ well-being and who endeavor to Glaucoma Care .......................... 6 provide them the best of care, and we write from that perspective. The two topics of greatest interest and need for most eye physicians right now are glaucoma and dry eye disease. -

Treatment of Postkeratitis Fusarium Endophthalmitis with Amphotericin B Lipid Complex
Cornea 19(6): 853–856, 2000. © 2000 Lippincott Williams & Wilkins, Inc., Philadelphia Treatment of Postkeratitis Fusarium Endophthalmitis with Amphotericin B Lipid Complex David Goldblum, M.D., Beatrice E. Frueh, M.D., Stefan Zimmerli, M.D., and Matthias Bo¨hnke, M.D. Purpose. The authors report the first case of Fusarium solani tients treated with amphotericin B develop some degree of renal keratitis that progressed to fungal endophthalmitis and was suc- impairment. Patients who receive a cumulated dose of more than cessfully treated with amphotericin B lipid complex (ABLC). 4–5 g of the drug are particularly at risk.5 Method. The case of a 34-year-old immunocompetent woman Three new lipid formulations of amphotericin B with reduced who developed a contact lens-related F. solani keratitis requiring nephrotoxicity are now available for clinical use. Amphotericin B emergency penetrating keratoplasty (PKP) was analyzed. The im- lipid complex (ABLC) (Abelcet®; The Liposome Company, munocompetent patient developed fungal endophthalmitis (ante- rior chamber tap positive for F. solani three months after PKP) and Princeton, NJ, U.S.A.) is a concentration of ribbon-like structures was eventually treated with ABLC. Results. Systemic amphoteri- of a bilayered membrane formed by combining a 7:3 ratio of cin B (total, 0.42 g) and ketoconazole in addition to topical nata- dimyristoyl phosphatidylcholine and dimyristoyl phosphatidyl- mycin and amphotericin did not prove to be effective in eradicat- glycerol with amphotericin B. Amphotericin B colloidal dispersion ing the mycosis in the anterior chamber. Under ABLC treatment (Amphocil®; Sequus Pharmaceuticals, Menlo Park, CA, U.S.A.) (total, 8.79 g), the anterior chamber inflammation resolved com- is composed of disc-like structures of cholesteryl sulfate com- pletely. -
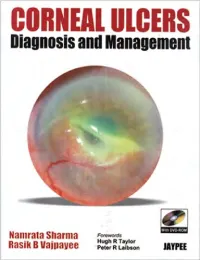
CORNEAL ULCERS Diagnosis and Management
CORNEAL ULCERS Diagnosis and Management System requirement: • Windows XP or above • Power DVD player (Software) • Windows Media Player 10.0 version or above • Quick time player version 6.5 or above Accompanying DVD ROM is playable only in Computer and not in DVD player. Kindly wait for few seconds for DVD to autorun. If it does not autorun then please do the following: • Click on my computer • Click the drive labelled JAYPEE and after opening the drive, kindly double click the file Jaypee CORNEAL ULCERS Diagnosis and Management Namrata Sharma MD DNB MNAMS Associate Professor of Ophthalmology Cornea, Cataract and Refractive Surgery Services Dr. Rajendra Prasad Centre for Ophthalmic Sciences All India Institute of Medical Sciences, New Delhi India Rasik B Vajpayee MS FRCSEd FRANZCO Head, Corneal and Cataract Surgery Centre for Eye Research Australia Royal Victorian Eye and Ear Hospital University of Melbourne Australia Forewords Hugh R Taylor Peter R Laibson ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD New Delhi • Ahmedabad • Bengaluru • Chennai • Hyderabad • Kochi • Kolkata • Lucknow • Mumbai • Nagpur Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd B-3 EMCA House, 23/23B Ansari Road, Daryaganj New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672 Rel: +91-11-32558559, Fax: +91-11-23276490, +91-11-23245683 e-mail: [email protected] Visit our website: www.jaypeebrothers.com Branches • 2/B, Akruti Society, Jodhpur Gam Road Satellite Ahmedabad 380 015, Phones: +91-79-26926233, -

Corneal Fungal Infections in Your Horse by Tammy Miller Michau, Noelle Mcnabb, Michele Stengard Diplomates of the American College of Veterinary Ophthalmologists
Corneal Fungal Infections in Your Horse by Tammy Miller Michau, Noelle McNabb, Michele Stengard Diplomates of the American College of Veterinary Ophthalmologists Fungal infection of the cornea in horses is an unfortunately common occurrence. It typically occurs following corneal trauma, for which horses are predisposed to due to the large size of their eyes, their environments and behavior. The trauma causes a break in the outer layer of the cornea (i.e. epithelium), which allows the normal ocular microflora, including fungal organisms, to invade the underlying corneal stroma and become pathogenic. Loss of the corneal epithelium is termed ulceration. Fungal organisms initially colonize the area of exposed stroma and incite secondary inflammation inside the eye (i.e. uveitis). Subsequently, the organisms can burrow into the deep corneal stroma, resulting in a stromal abscess or loss of stroma with risk of corneal rupture. Clinical findings Horses with fungal keratitis are often painful. They will squint, blink, and tear excessively. Eyelid swelling can also occur. Fungal keratitis should always be suspected in any ulcer that does not heal within 2-3 days. The appearance of fungal ulcers ranges widely from small superficial ulcers, to punctate lesions, to deep abscessation. Fungal keratitis in horses also commonly appears as a white or yellow plaque on the cornea. A furrow that develops around the plaque is associated with a poorer prognosis. Diagnosis Cytology, obtained by scraping the area of ulceration, is the quickest way to diagnose the disease but does not always confirm the presence of the organisms. Culture can also be performed but usually takes 2 weeks to get the results.