Physiology and Pathophysiology of Oxygen Sensitivity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Oxygen Sensing by Ion Channels
Kidney International, Vol. 51 (1997), pp. 454—461 ION CHANNELS AND HEME PROTEINS AS OXYGEN SENSORS Oxygen sensing by ion channels JoSE LOPEZ-BARNEO, PATRICIA ORTEGA-SAENZ, ANTONIO MOLINA, ALFREDO FRANCO-OBREGON, JUAN UREA, and ANTONIO CASTELLANO Departamento de Fisiologla Médica y Biofisica, Universidad de Sevilla, Facultad de Medicina, Sevilla, Spain Oxygen is required for the survival of all higher life forms due 02-sensitive ion channels and chemotransduction in arterial to its role in mitochondrial respiration permitting ATP synthesis chemoreceptors by oxidative phosphorylation. Oxygen is also necessary for many The carotid bodies, located in the bifurcation of the carotid other cellular functions, including the synthesis of steroid hor-artery, are the main arterial oxygen chemoreceptors in mammals. mones or the generation of reactive oxygen species in the macro-The mechanisms underlying the basic transductional process have phage defense response. In mammals, 02 diffuses into the bloodremained obscure for decades, but most authors have traditionally in the lungs, is concentrated within the erythrocytes by its bindingascribed a central role to the glomus, or type I, cells, which are of to hemoglobin and is distributed throughout the body by theneuroectodermal origin. These cells contain numerous cytosolic circulatory system. Arterial and tissular 02 tension (P02) are keptgranules rich in dopamine and other neurotransmitters and within restricted limits by short- and long-term adaptative mech-peptides, establishing synapses with afferent sensory fibers of the anisms set in motion by changes in 07 availability due tosinus nerve. Hence, it was widely accepted that glomus cells act as environmental or physiological circumstances. An immediatethe primary 02 sensors releasing transmitters that stimulate the response to a hypoxic stress is the reflex increase in respiratoryafferent fibers of the sinus nerve in response to low P02 [1, 21. -

A Possible Role of the Glomus Cell in Controlling Vascular Tone of the Carotid Labyrinth of Xenopus Laevis
Tohoku J. exp. Med., 1987, 151, 395-408 A Possible Role of the Glomus Cell in Controlling Vascular Tone of the Carotid Labyrinth of Xenopus laevis TATSUMIKUSAKABE, * KAZUKOISHII and KOSEI ISHIIt Department of Physiology, Fukushima Medical College, Fukushima 960 KUSAKABE,T., ISHII,K. and Isxu, K. A Possible Role of the Glomus Cell in Controlling Vascular Tone of the Carotid Labyrinth of Xenopus laevis. Tohoku J. exp. Med., 1987, 151(4), 395-408 To clarify the physiological significance of the g-s connection (intimate apposition of the glomus cell to the smooth muscle) in the Xenopus carotid labyrinth, experiments were carried out morphologically and physiologically. Results obtained are as follows. 1. Efferent electrical stim- ulation of the glossopharyngeal nerve resulted in concentrating dense-cored vesicles on the peripheral region of the glomus cell, and a decrease of vesicles as a whole. 2. In the carotid labyrinth perfused artificially, outflow of the internal and the external carotid arteries decreased with administration of catecholamines (adrenaline, noradrenaline and dopamine). 3. Acetylcholine reduced only the internal outflow. This response was depressed by atropine, hexamethonium and phenotolamine, whereas accelerated by propranolol. 4. Sodium cyanide reduced the internal outflow without affecting the external outflow, and its effect is depressed by phentolamine. From these results, a possibility that the glomus cell participates in controlling the blood flow in the labyrinth through the intervention of the g-s connection was discussed. Xenopus laevis ; carotid labyrinth ; glomus cell ; catecholamine ; arterial chemoreceptor The carotid labyrinth of amphibia has a chemoreceptor function (Ishii et al. 1966) and contains glomus cells similar to those of many animal species in fine structure (Rogers 1963; Ishii and Oosaki 1969; Poullet-Krieger 1973). -

Oxygen Chemoreception by Carotid Body Cells in Culture (Glomus Cells/Dopamine/Hypoxia/Sensory Cells) MARK C
Proc. Nati. Acad. Sci. USA Vol. 82, pp. 1448-1450, March 1985 Cell Biology Oxygen chemoreception by carotid body cells in culture (glomus cells/dopamine/hypoxia/sensory cells) MARK C. FISHMAN*t#§¶, WILLIAM L. GREENEt§, AND DoRos PLATIKAt¶ *Howard Hughes Medical Institute, tThe Developmental Biology Laboratory (Medical Services), and *Neurology Services of the Massachusetts General Hospital, Boston, MA 02114; and Departments of §Medicine and ¶Neurology, Harvard Medical School, Boston, MA 02115 Communicated by Jerome Gross, October 29, 1984 ABSTRACT Chemoreceptors for oxygen reside within the enrichment procedure. Hypoxic conditions were identical carotid body, but it is not known which cells actually sense except that the Po2 was diminished to 36 mm Hg. Since there hypoxia and by what mechanisms they transduce this informa- are only a few thousand cells in the carotid body, each ex- tion into afferent signals in the carotid sinus nerve. We have periment necessitated the pooling of dissociated cells of 10- developed systems for the growth of glomus cells of the carotid 12 rats and subsequent distribution to two plates, one to be body in dissociated cell culture. Here we demonstrate that, as used for control and one for hypoxic conditions. Cells in in vivo, these cells contain the putative neurotransmitters do- both plates for each experiment were grown in culture for pamine, serotonin, and norepinephrine. Oxygen tension regu- the same period of time. Experiments were performed after lates the rate of dopamine secretion from the glomus cells. culturing of the cells for 5-7 days. Similar to chemically stimulated catecholamine secretion from Prior to testing the cells were washed twice in Hanks' bal- other adrenergic cells this hypoxia-stimulated release requires anced salt solution supplemented with 100 ,uM pargyline/5 extracellular calcium. -
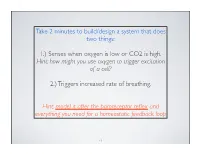
1.) Senses When Oxygen Is Low Or CO2 Is High. Hint: How Might You Use Oxygen to Trigger Excitation of a Cell?
Take 2 minutes to build/design a system that does two things: 1.) Senses when oxygen is low or CO2 is high. Hint: how might you use oxygen to trigger excitation of a cell? 2.) Triggers increased rate of breathing. Hint: model it after the baroreceptor reflex and everything you need for a homeostatic feedback loop 31 Step 1: we need a sensor. 32 Peripheral chemoreceptors monitor PO2, PCO2, pH Video from: http://bk.psu.edu/clt/bisc4/ipweb/systems/buildframes.html?respiratory/conresp/01 3 Glomus cells are peripheral chemoreceptors which sense O2, CO2, pH Blood vessel Low PO 2 Low P O 2 K+ channels close This system responds Cell when PaO2 gets very depolarizes Glomus cell in carotid low (~60 mmHg) body Ca2+ Relevant at high enters Voltage-gated Ca2+ altitudes or in chronic channel opens pulmonary disease Exocytosis of neurotransmitters Glomus cells also Receptor on sensory neuron respond to PaCO2 Action potential Increase in ventilation=faster Signal to medullary breathing=more O2 centers to increase 4 ventilation in, more CO2 out Central chemoreceptors in brain monitor PCO2 Video from: http://bk.psu.edu/clt/bisc4/ipweb/systems/buildframes.html?respiratory/conresp/015 Sidenote: wait wait wait wait......wait. CO2 is most important factor?? Remember changes in CO2 affect pH. Dangerous and deadly. Remember also that hemoglobin has oxygen reserves 6 Step 2: send signal to integrating center 7 Peripheral chemoreceptors monitor PO2, PCO2, pH Video from: http://bk.psu.edu/clt/bisc4/ipweb/systems/buildframes.html?respiratory/conresp/01 8 Step 3: have integrating center cause change in effectors 9 10 Figure 18.17 REVIEW: CHEMORECEPTOR RESPONSE Central Chemoreceptors Peripheral Chemoreceptors + Central chemoreceptors monitor CO2 in cerebrospinal fluid. -

Morphological and New Neurochemical Aspects of the Mammalian Carotid Body
Trakia Journal of Sciences, Vol. 17, Suppl. 2, pp 67-72, 2019 Copyright © 2019 Trakia University Available online at: http://www.uni-sz.bg ISSN 1313-3551 (online) doi:10.15547/tjs.2019.s.02.015 MORPHOLOGICAL AND NEW NEUROCHEMICAL ASPECTS OF THE MAMMALIAN CAROTID BODY N. Lazarov1,2,*, D. Atanasova2,3 1Department of Anatomy and Histology, Medical University of Sofia, Sofia, Bulgaria 2Institute of Neurobiology, Bulgarian Academy of Sciences, Sofia, Bulgaria 3Department of Anatomy, Faculty of Medicine, Trakia University, Stara Zagora, Bulgaria ABSTRACT The carotid body (CB) is a polymodal chemosensory organ that plays an essential role in initiating respiratory and cardiovascular adjustments to maintain blood gas homeostasis. It is strategically located at the carotid bifurcation. The CB works in concert with the apposing afferent nerve endings of the petrosal ganglion (PG) cells and together they form a functional unit, the CB chemosensory system. The organ consists of small clusters called glomeruli composed of two cell types, glomus and sustentacular cells, interspersed by blood vessels and nerve bundles, and separated by connective tissue. During chemotransduction glomus cells release a variety of neurotransmitters which activate chemoafferent nerve endings of PG neurons. Much of the available evidence suggests that the CB dysfunction and altered oxygen homeostasis are involved in the pathophysiology of several diseases including systemic hypertension. Our recent data show that in glomus cells of hypertensive animals the production of nitric oxide is impaired and components of the neurotrophin signaling system display enhanced expression. These results suggest that a heightened chemosensory discharge may contribute to sympathetic hyperactivity leading to hypertension. -

HIF-2A Is Essential for Carotid Body Development and Function
RESEARCH ARTICLE HIF-2a is essential for carotid body development and function David Macias1*, Andrew S Cowburn1,2, Hortensia Torres-Torrelo3, Patricia Ortega-Sa´ enz3, Jose´ Lo´ pez-Barneo3, Randall S Johnson1,4* 1Department of Physiology, Development and Neuroscience, University of Cambridge, Cambridge, United Kingdom; 2Department of Medicine, University of Cambridge, Cambridge, United Kingdom; 3Instituto de Biomedicina de Sevilla, Seville, Spain; 4Department of Cell and Molecular Biology, Karolinska Institute, Stockholm, Sweden Abstract Mammalian adaptation to oxygen flux occurs at many levels, from shifts in cellular metabolism to physiological adaptations facilitated by the sympathetic nervous system and carotid body (CB). Interactions between differing forms of adaptive response to hypoxia, including transcriptional responses orchestrated by the Hypoxia Inducible transcription Factors (HIFs), are complex and clearly synergistic. We show here that there is an absolute developmental requirement for HIF-2a, one of the HIF isoforms, for growth and survival of oxygen sensitive glomus cells of the carotid body. The loss of these cells renders mice incapable of ventilatory responses to hypoxia, and this has striking effects on processes as diverse as arterial pressure regulation, exercise performance, and glucose homeostasis. We show that the expansion of the glomus cells is correlated with mTORC1 activation, and is functionally inhibited by rapamycin treatment. These findings demonstrate the central role played by HIF-2a in carotid body development, growth and function. DOI: https://doi.org/10.7554/eLife.34681.001 *For correspondence: [email protected] (DM); Introduction [email protected] (RSJ) Detecting and responding to shifts in oxygen availability is essential for animal survival. Responding to changes in oxygenation occurs in cells, tissues, and at the level of the whole organism. -

Striking Parallels Between Carotid Body Glomus Cell and Adrenal Chroma N MARK Cell Development
Developmental Biology 444 (2018) S308–S324 Contents lists available at ScienceDirect Developmental Biology journal homepage: www.elsevier.com/locate/developmentalbiology ffi Striking parallels between carotid body glomus cell and adrenal chroma n MARK cell development Dorit Hockmana,b,c,1, Igor Adameykod,e, Marketa Kauckad, Perrine Barrauda, Tomoki Otania, Adam Hunta, Anna C. Hartwigf, Elisabeth Sockf, Dominic Waitheg, Marina C.M. Franckh,2, Patrik Ernforsh, Sean Ehingeri,3, Marthe J. Howardi, Naoko Brownj,Jeffrey Reesej, ⁎ Clare V.H. Bakera, a Department of Physiology, Development and Neuroscience, University of Cambridge, Anatomy Building, Downing Street, Cambridge CB2 3DY, United Kingdom b Weatherall Institute of Molecular Medicine, John Radcliffe Hospital, Headley Way, Oxford OX3 9DS, United Kingdom c Department of Molecular and Cell Biology, University of Cape Town, Cape Town, South Africa d Department of Physiology and Pharmacology, Karolinska Institute, S-171 77 Stockholm, Sweden e Center for Brain Research, Medical University Vienna, 1090 Vienna, Austria f Institut für Biochemie, Emil-Fischer-Zentrum, Friedrich-Alexander-Universität Erlangen-Nürnberg, Fahrstrasse 17, 91054 Erlangen, Germany g Wolfson Imaging Centre, Weatherall Institute of Molecular Medicine, John Radcliffe Hospital, Headley Way, Oxford OX3 9DS, United Kingdom h Unit of Molecular Neurobiology, Department of Medical Biochemistry and Biophysics, Karolinska Institute, S-171 77 Stockholm, Sweden i Department of Neurosciences and Program in Neurosciences and Neurodegenerative Diseases, University of Toledo Health Sciences Campus, Toledo, OH 43614, USA j Depts. of Pediatrics, Cell and Developmental Biology, Vanderbilt University Medical Center, 2215 B Garland Avenue, Nashville, TN 37232, USA ARTICLE INFO ABSTRACT Keywords: Carotid body glomus cells mediate essential reflex responses to arterial blood hypoxia. -
HIF-2Α Is Essential for Carotid Body Development and Function 3 4 5 6 David Macías1, Andrew S
bioRxiv preprint doi: https://doi.org/10.1101/250928; this version posted January 19, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 2 HIF-2α is essential for carotid body development and function 3 4 5 6 David Macías1, Andrew S. Cowburn1,2, Hortensia Torres-Torrelo3, Patricia 7 Ortega-Sáenz3, José López-Barneo3, and Randall S. Johnson1,4,5. 8 9 1Department of Physiology, Development and Neuroscience. 2Department of 10 Medicine, University of Cambridge, Cambridge, UK; 3Instituto de Biomedicina 11 de Sevilla (IBiS), Seville, Spain. 4Department of Cell and Molecular Biology, 12 Karolinska Institute, Stockholm, Sweden. 13 14 15 16 17 18 19 20 21 22 23 Keywords: hypoxia, carotid body, oxygen sensing, HIF-2α, HVR, physiological 24 responses 25 26 27 28 5For correspondence: Professor Randall S. Johnson, Department of 29 Physiology, Development and Neuroscience, University of Cambridge, 30 Downing Street, Cambridge. CB2 3EG. United Kingdom. E-mail: 31 [email protected] 32 33 1 bioRxiv preprint doi: https://doi.org/10.1101/250928; this version posted January 19, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 34 Summary 35 Mammalian adaptation to oxygen flux occurs at many levels, from shifts in 36 cellular metabolism to physiological adaptations facilitated by the sympathetic 37 nervous system and carotid body (CB). -

Adrenomedullin Expression and Function in the Rat Carotid Body
95 Adrenomedullin expression and function in the rat carotid body A Martínez, L Saldise1, M J Ramírez2, S Belzunegui1, E Zudaire, M R Luquin1 and F Cuttitta Cell and Cancer Biology Branch, National Cancer Institute, National Institutes of Health, Building 10, Room 13N262, Bethesda, Maryland 20892, USA 1Department of Experimental Neurology, University of Navarra, 31080 Pamplona, Spain 2Department of Pharmacology, University of Navarra, 31080 Pamplona, Spain (Requests for offprints should be addressed to A Martínez; Email: [email protected]) Abstract Adrenomedullin (AM) immunoreactivity has been found 60 nM AM/g body weight into the tail vein of the rats did in granules of the glomus (type I) cells of the carotid bodies not induce statistical differences in DA release from the in rats. The identity of these cells was ascertained by carotid bodies. Exposure of the oxygen-sensitive cell line colocalization of immunoreactivities for AM and tyrosine PC-12 to hypoxia elicited an increase in AM mRNA hydroxylase in their cytoplasm. Exposure of freshly iso- expression and peptide secretion into serum-free condi- lated carotid bodies to synthetic AM resulted in a tioned medium. Previous data have shown that elevation concentration- and time-dependent degranulation of of AM expression under hypoxia is mediated through glomus cells as measured by dopamine (DA) release. DA hypoxia-inducible factor-1, and that exposure of chroma- release reached a zenith 30 min after exposure to AM ffin cells to AM results in degranulation. All these data (94·2% over untreated controls). At this time-point, the suggest that AM is an important autocrine regulator of response to AM was similar to the one elicited by 5 min of carotid body function. -

H2S Mediates Carotid Body Response to Hypoxia but Not Anoxia T ⁎ Ying-Jie Peng , Vladislav V
Respiratory Physiology & Neurobiology 259 (2019) 75–85 Contents lists available at ScienceDirect Respiratory Physiology & Neurobiology journal homepage: www.elsevier.com/locate/resphysiol H2S mediates carotid body response to hypoxia but not anoxia T ⁎ Ying-Jie Peng , Vladislav V. Makarenko, Anna Gridina, Irina Chupikova, Xiuli Zhang, Ganesh K. Kumar, Aaron P. Fox, Nanduri R. Prabhakar Institute for Integrative Physiology and Center for Systems Biology of O2Sensing, University of Chicago, Chicago, IL, 60637, USA ARTICLE INFO ABSTRACT Keywords: The role of cystathionine-γ-lyase (CSE) derived H2S in the hypoxic and anoxic responses of the carotid body (CB) Cystathionine-γ-lyase were examined. Experiments were performed on Sprague-Dawley rats, wild type and CSE knockout mice on H S synthesis inhibitors 2 C57BL/6 J background. Hypoxia (pO2 = 37 ± 3 mmHg) increased the CB sensory nerve activity and elevated Hypoxic ventilatory response H2S levels in rats. In contrast, anoxia (pO2 = 5 ± 4 mmHg) produced only a modest CB sensory excitation with Carotid body chemo reflex no change in H2S levels. DL-propargylglycine (DL-PAG), a blocker of CSE, inhibited hypoxia but not anoxia- 2+ evoked CB sensory excitation and [Ca ]i elevation of glomus cells. The inhibitory effects of DL-PAG on hypoxia were seen: a) when it is dissolved in saline but not in dimethyl sulfoxide (DMSO), and b) in glomus cells cultured for18 h but not in cells either soon after isolation or after prolonged culturing (72 h) requiring 1–3 h of in- 2+ cubation. On the other hand, anoxia-induced [Ca ]i responses of glomus cell were blocked by high con- centration of DL-PAG (300μM) either alone or in combination with aminooxyacetic acid (AOAA; 300μM) with a 2+ decreased cell viability. -

Peripheral Arterial Chemoreceptors and the Evolution of the Carotid Body William K
Respiratory Physiology & Neurobiology 157 (2007) 4–11 Peripheral arterial chemoreceptors and the evolution of the carotid body William K. Milsom a,∗, Mark L. Burleson b a Department of Zoology, University of British Columbia, Vancouver, BC, Canada V6T 1Z4 b Department of Biological Sciences, University of North Texas, Denton, TX 76203-5220, United States Accepted 12 February 2007 Abstract There has been a reduction in the distribution of peripheral respiratory O2 chemoreceptors from multiple, dispersed sites in fish and amphibia to a single dominant receptor site in birds and mammals. In the process, the cells in the fish gill associated with O2 chemosensing (5-HT containing neuroepithelial cells often found in association with ACh/catecholamine (CA) containing cells) are replaced by the glomus cells of the mammalian carotid body (which contain multiple putative neurotransmitter substances, including 5-HT, CA and ACh, all within the same cells), although this difference may be more superficial than first appears. While still highly speculative, these trends would appear to be correlated with the transition from aquatic respiration and bimodal breathing, and from animals with intra-cardiac shunts (two situations where the ability to sense O2 at multiple sites would be an advantage), to strictly air breathing in animals with no intra-cardiac shunts. It is also tempting to speculate that while the basic O2-sensing mechanism is the same for all receptor cells, the receptor groups in fish have evolved in such a way to make the responses of some more sensitive to changes in O2 delivery than others. The net result is that those receptors associated with the first gill arch of fish (the third branchial arch) become the carotid body in higher vertebrates associated with the regulation of ventilation and ensuring oxygen supply to the gas exchange surface. -

Carbon Monoxide: a Role in Carotid Body Chemoreception (Heme Oxygenase 2/Zinc Protoporphyrin IX) NANDURI R
Proc. Natl. Acad. Sci. USA Vol. 92, pp. 1994-1997, March 1995 Neurobiology Carbon monoxide: A role in carotid body chemoreception (heme oxygenase 2/zinc protoporphyrin IX) NANDURI R. PRABHAKAR*, JAY L. DINERMANtt, FATON H. AGANI*, AND SOLOMON H. SNYDERt§v *Departments of Physiology and Biophysics, Case Western Reserve University, Cleveland, OH; and the Departments of tMedicine (Cardiology), iNeuroscience, §Pharmacology and Molecular Sciences and Psychiatry, Johns Hopkins University School of Medicine, Baltimore, MD 21205 Contributed by Solomon H. Snyder, November 28, 1994 ABSTRACT Carbon monoxide (CO), produced endog- mg/kg; i.p.), the trachea was intubated, and a femoral artery enously by heme oxygenase, has been implicated as a neuronal and vein were cannulated. The arterial catheter was used for messenger. Carotid bodies are sensory organs that regulate monitoring arterial blood pressure. Systemic administration of ventilation by responding to alterations of blood oxygen, CO2, fluids was accomplished through the venous catheter. To and pH. Changes in blood gases are sensed by glomus cells in expose the carotid bifurcation, the trachea and esophagus were the carotid body that synapse on afferent terminals of the ligated above the site of tracheal cannulation, sectioned, and carotid sinus nerve that projects to respiratory-related neu- retracted rostrally. The exposed tissues were covered with rons in the brainstem. Using immunocytochemistry, we dem- cotton gauze soaked in saline. Body temperature was main- onstrate that heme oxygenase 2 is localized to glomus cells in tained at 38 ± 1°C by a heating blanket governed by a rectal the cat and rat carotid bodies. Physiological studies show that thermistor probe.