The Nondystrophic Myotonias
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Periodic Paralysis: a Case Report of Normokalemic Presentation in a Young Girl
Case Report ISSN: 2574 -1241 DOI: 10.26717/BJSTR.2021.35.005673 Periodic Paralysis: A Case Report of Normokalemic Presentation in a Young Girl Lucio Ceglie, Roberta Patacchiola, Daniela Iannucci, Miriana Guarino, Lorenzo Sansone, Maria Chiara Sgarrella, Francesco Chiarelli* and Annalisa Blasetti Department of Pediatrics, University of Chieti, Italy *Corresponding author: Francesco Chiarelli, Department of Pediatrics, University of Chieti, Italy ARTICLE INFO ABSTRACT Received: April 10, 2021 The skeletal muscle channelopathies represent a rare group of neuromuscular disorders which are caused by genetic mutations regarding voltage-gated ion Published: April 21, 2021 channels, which play an important role in muscle membrane depolarization. Muscle channelopathies are broadly divided into 2 main categories: nondystrophic myotonias (NDM) and periodic paralysis (PP). Periodic paralysis (PP) are rare autosomal dominant Citation: Lucio C, Roberta P, Daniela I, neuromuscular disorders, characterized clinically by periodic attacks of muscle weakness Miriana G, Francesco C, et al., Periodic in concomitance with serum potassium level alterations. It is possible to distinguish Paralysis: A Case Report of Normokalemic normokalemic, hyperkalemic and hypokalemic paralysis. PP is caused by genetic Presentation in a Young Girl. Biomed mutations in voltage-gate ion channels like sodium, potassium, and calcium channels, J Sci & Tech Res 35(2)-2021. BJSTR. which are determinant for muscle membrane depolarization. The most common genes MS.ID.005672. involved in pathogenesis are CACN1S, SCN4A and KCNJ2, encoding calcium, sodium, and potassium channels (Table 1). Moreover, paralysis related to serum potassium values Keywords: Hypokalemia; Periodic Paral- may also occur in thyreotoxicosis [1], Liddle syndrome, Gitelman syndrome, primary ysis; Transient Paralysis; Muscular Weak- hyperaldosteronism, and acid-base balance disorders. -

The Role of Z-Disc Proteins in Myopathy and Cardiomyopathy
International Journal of Molecular Sciences Review The Role of Z-disc Proteins in Myopathy and Cardiomyopathy Kirsty Wadmore 1,†, Amar J. Azad 1,† and Katja Gehmlich 1,2,* 1 Institute of Cardiovascular Sciences, College of Medical and Dental Sciences, University of Birmingham, Birmingham B15 2TT, UK; [email protected] (K.W.); [email protected] (A.J.A.) 2 Division of Cardiovascular Medicine, Radcliffe Department of Medicine and British Heart Foundation Centre of Research Excellence Oxford, University of Oxford, Oxford OX3 9DU, UK * Correspondence: [email protected]; Tel.: +44-121-414-8259 † These authors contributed equally. Abstract: The Z-disc acts as a protein-rich structure to tether thin filament in the contractile units, the sarcomeres, of striated muscle cells. Proteins found in the Z-disc are integral for maintaining the architecture of the sarcomere. They also enable it to function as a (bio-mechanical) signalling hub. Numerous proteins interact in the Z-disc to facilitate force transduction and intracellular signalling in both cardiac and skeletal muscle. This review will focus on six key Z-disc proteins: α-actinin 2, filamin C, myopalladin, myotilin, telethonin and Z-disc alternatively spliced PDZ-motif (ZASP), which have all been linked to myopathies and cardiomyopathies. We will summarise pathogenic variants identified in the six genes coding for these proteins and look at their involvement in myopathy and cardiomyopathy. Listing the Minor Allele Frequency (MAF) of these variants in the Genome Aggregation Database (GnomAD) version 3.1 will help to critically re-evaluate pathogenicity based on variant frequency in normal population cohorts. -

Neuromuscular Disorders Neurology in Practice: Series Editors: Robert A
Neuromuscular Disorders neurology in practice: series editors: robert a. gross, department of neurology, university of rochester medical center, rochester, ny, usa jonathan w. mink, department of neurology, university of rochester medical center,rochester, ny, usa Neuromuscular Disorders edited by Rabi N. Tawil, MD Professor of Neurology University of Rochester Medical Center Rochester, NY, USA Shannon Venance, MD, PhD, FRCPCP Associate Professor of Neurology The University of Western Ontario London, Ontario, Canada A John Wiley & Sons, Ltd., Publication This edition fi rst published 2011, ® 2011 by Blackwell Publishing Ltd Blackwell Publishing was acquired by John Wiley & Sons in February 2007. Blackwell’s publishing program has been merged with Wiley’s global Scientifi c, Technical and Medical business to form Wiley-Blackwell. Registered offi ce: John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK Editorial offi ces: 9600 Garsington Road, Oxford, OX4 2DQ, UK The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK 111 River Street, Hoboken, NJ 07030-5774, USA For details of our global editorial offi ces, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell The right of the author to be identifi ed as the author of this work has been asserted in accordance with the UK Copyright, Designs and Patents Act 1988. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher. -
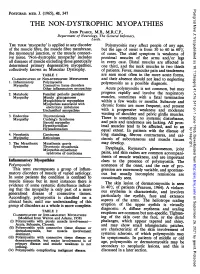
THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, the General Infirmary, Leeds
Postgrad Med J: first published as 10.1136/pgmj.41.476.347 on 1 June 1965. Downloaded from POSTGRAD. MED. J. (1965), 41, 347 THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, The General Infirmary, Leeds. THE TERM 'myopathy' is applied to any disorder Polymyositis may affect people of any age, of the muscle fibre, the muscle fibre membrane, but the age of onset is from 30 to 60 in 60% the myoneural junction, or the muscle connect- of cases. The chief symptom is weakness of ive tissue. 'Non-dystrophic myopathy' includes proximal muscles of the arms and/or legs all diseases of muscle excluding those genetically in every case. Distal muscles are affected in determined primary degenerative myopathies, one third, and the neck muscles in two thirds collectively known as Muscular Dystrophy. of patients. Fever, muscular pain and tenderness TABLE 1 are seen most often in the more acute forms, CLASSIFICATION OF NON-DYSTROPHIC MYOPATHIES and their absence should not lead to neglecting 1. Inflammatory Polymyositis as a Myopathy Connective tissue disorders polymyositis possible diagnosis. Other inflammatory mvopathies Acute polymyositis is not common, but may 2. Metabolic Familial periodic paralysis progress rapidly and involve the respiratory Myopathy Muscle glycogenoses muscles, sometimes with a fatal termination Myoglobinuric myopathies within a few weeks or months. Myopathies associated with Subacute and electrolyte imbalance chronic forms are more frequent, and present Unclassified myopathies with a progressive weakness and moderate of shoulder 3. Endocrine Thyrotoxicosis wasting and pelvic girdle muscles. Myopathy Cushing's Syndrome There is sometimes no systemic disturbance, Steroid myopathy and pain and tenderness are lacking. -

Periodic Paralysis
Periodic Paralysis In Focus Dear Readers Fast Facts This “In Focus” report is the third in a series of MDA’s three-year commitment for all Hypokalemic periodic paralysis MDA comprehensive reports about the latest in periodic paralysis research as of March Hypokalemic PP can begin anywhere from neuromuscular disease research and manage- 2009 is $1,938,367. The Association’s early childhood to the 30s, with periodic ment. allocation for research on hyperkalemic attacks of severe weakness lasting hours This report focuses on the periodic and hypokalemic periodic paralysis to days. The frequency of attacks gener- paralyses, a group of disorders that result from research since 1950 is $8,125,341. ally lessens in the 40s or 50s. Permanent malfunctions in so-called ion channels, micro- MDA’s allocation for the recently weakness may persist between attacks, scopic tunnels that make possible high-speed identified Andersen-Tawil syndrome usually beginning in middle age and pro- movement of electrically charged particles is $515,430 since 2001. MDA is cur- gressing slowly over years. across barriers inside cells and between cells rently funding 11 grants in the periodic The most common underlying cause and their surroundings. paralyses. is any of several genetic mutations in When ion channels fail to open or close The periodic paralyses are gener- a gene on chromosome 1 that carries according to an exquisitely fine-tuned program, ally divided into hyperkalemic periodic instructions for a calcium channel protein episodes of paralysis of the skeletal muscles paralysis, hypokalemic periodic paralysis in skeletal muscle fibers. When this chan- and even temporary irregularities in the heart- and Andersen-Tawil syndrome. -

Facilitations and Hurdles of Genetic Testing in Neuromuscular Disorders
diagnostics Review Facilitations and Hurdles of Genetic Testing in Neuromuscular Disorders Andrea Barp 1,*, Lorena Mosca 2 and Valeria Ada Sansone 1 1 The NEMO Clinical Center in Milan, Neurorehabilitation Unit, University of Milan, Piazza Ospedale Maggiore 3, 20162 Milano, Italy; [email protected] 2 Medical Genetics Unit, ASST Grande Ospedale Metropolitano Niguarda, Piazza Ospedale Maggiore 3, 20162 Milano, Italy; [email protected] * Correspondence: [email protected] Abstract: Neuromuscular disorders (NMDs) comprise a heterogeneous group of disorders that affect about one in every thousand individuals worldwide. The vast majority of NMDs has a genetic cause, with about 600 genes already identified. Application of genetic testing in NMDs can be useful for several reasons: correct diagnostic definition of a proband, extensive familial counselling to identify subjects at risk, and prenatal diagnosis to prevent the recurrence of the disease; furthermore, identification of specific genetic mutations still remains mandatory in some cases for clinical trial enrollment where new gene therapies are now approaching. Even though genetic analysis is catching on in the neuromuscular field, pitfalls and hurdles still remain and they should be taken into account by clinicians, as for example the use of next generation sequencing (NGS) where many single nucleotide variants of “unknown significance” can emerge, complicating the correct interpretation of genotype-phenotype relationship. Finally, when all efforts in terms of molecular analysis have been carried on, a portion of patients affected by NMDs still remain “not genetically defined”. In the present review we analyze the evolution of genetic techniques, from Sanger sequencing to NGS, and we discuss “facilitations and hurdles” of genetic testing which must always be balanced by clinicians, Citation: Barp, A.; Mosca, L.; in order to ensure a correct diagnostic definition, but taking always into account the benefit that the Sansone, V.A. -

Identification of Gene Mutations in Patients with Primary Periodic
Luo et al. BMC Neurology (2019) 19:92 https://doi.org/10.1186/s12883-019-1322-6 RESEARCH ARTICLE Open Access Identification of gene mutations in patients with primary periodic paralysis using targeted next-generation sequencing Sushan Luo1†, Minjie Xu2†, Jian Sun1, Kai Qiao3, Jie Song1, Shuang Cai1, Wenhua Zhu1, Lei Zhou1, Jianying Xi1, Jiahong Lu1, Xiaohua Ni2, Tonghai Dou4 and Chongbo Zhao1,5* Abstract Background: Primary periodic paralysis is characterized by recurrent quadriplegia typically associated with abnormal serum potassium levels. The molecular diagnosis of primary PP previously based on Sanger sequencing of hot spots or exon-by-exon screening of the reported genes. Methods: We developed a gene panel that includes 10 ion channel-related genes and 245 muscular dystrophy- and myopathy-related genes and used this panel to diagnose 60 patients with primary periodic paralysis and identify the disease-causing or risk-associated gene mutations. Results: Mutations of 5 genes were discovered in 39 patients (65.0%). SCN4A, KCNJ2 and CACNA1S variants accounted for 92.5% of the patients with a genetic diagnosis. Conclusions: Targeted next-generation sequencing offers a cost-effective approach to expand the genotypes of primary periodic paralysis. A clearer genetic profile enables the prevention of paralysis attacks, avoidance of triggers and the monitoring of complications. Keywords: Primary periodic paralysis, Targeted next-generation sequencing, Gene panel, Gene mutation distribution, Calcium homeostasis. Background (SCN4A) and potassium voltage-gated channel subfamily Periodic paralysis (PP) is characterized by episodes of J member 2 (KCNJ2), that encode voltage-gated chan- muscle weakness that occur at irregular intervals due to nels in muscle membranes that generate or sustain skeletal muscle ion channelopathies. -

Distal Myopathies a Review: Highlights on Distal Myopathies with Rimmed Vacuoles
Review Article Distal myopathies a review: Highlights on distal myopathies with rimmed vacuoles May Christine V. Malicdan, Ikuya Nonaka Department of Neuromuscular Research, National Institutes of Neurosciences, National Center of Neurology and Psychiatry, Tokyo, Japan Distal myopathies are a group of heterogeneous disorders Since the discovery of the gene loci for a number classiÞ ed into one broad category due to the presentation of distal myopathies, several diseases previously of weakness involving the distal skeletal muscles. The categorized as different disorders have now proven to recent years have witnessed increasing efforts to identify be the same or allelic disorders (e.g. distal myopathy the causative genes for distal myopathies. The identiÞ cation with rimmed vacuoles and hereditary inclusion body of few causative genes made the broad classiÞ cation of myopathy, Miyoshi myopathy and limb-girdle muscular these diseases under “distal myopathies” disputable and dystrophy type 2B (LGMD 2B). added some enigma to why distal muscles are preferentially This review will focus on the most commonly affected. Nevertheless, with the clariÞ cation of the molecular known and distinct distal myopathies, using a simple basis of speciÞ c conditions, additional clues have been classification: distal myopathies with known molecular uncovered to understand the mechanism of each condition. defects [Table 1] and distal myopathies with unknown This review will give a synopsis of the common distal causative genes [Table 2]. The identification of the myopathies, presenting salient facts regarding the clinical, genes involved in distal myopathies has broadened pathological, and molecular aspects of each disease. Distal this classification into sub-categories as to the location myopathy with rimmed vacuoles, or Nonaka myopathy, will of encoded proteins: sarcomere (titin, myosin); plasma be discussed in more detail. -

Cerebral Hypotonia by Mihee Bay MD (Dr
Cerebral hypotonia By Mihee Bay MD (Dr. Bay of Kennedy Krieger Institute and Johns Hopkins School of Medicine has no relevant financial relationships to disclose.) Originally released July 12, 2006; last updated February 1, 2016; expires February 1, 2019 Introduction This article includes discussion of cerebral hypotonia, central hypotonia, essential hypotonia, benign congenital hypotonia, and floppy infant. The foregoing terms may include synonyms, similar disorders, variations in usage, and abbreviations. Overview Hypotonia is a clinical manifestation of numerous diseases affecting the central and/or peripheral motor nervous system. The key to accurate diagnosis involves integral steps of evaluation that include a detailed history, examination, and diagnostic tests. “Cerebral” (or central) hypotonia implies pathogenesis from abnormalities from the central nervous system, and related causal disorders include cerebral dysgenesis and genetic or metabolic disorders. Patients with central hypotonia generally have hypotonia without associated weakness, in contrast to the peripheral (lower motor neuron) causes, which typically produce both hypotonia and muscle weakness. Hypotonia is a clinical manifestation of over 500 genetic disorders; thus, a logical, stepwise approach to diagnosis is essential. With recent advances in the field of genetic testing, diagnostic yield will undoubtedly improve. There is no cure, but treatment includes supportive therapies, such as physical and occupational therapy, and diagnosis-specific management. Key points • Hypotonia is reduced tension or resistance of passive range of motion. • The first step in the evaluation of a child with hypotonia is localization to the central (“cerebral”) or peripheral nervous system, or both. • Central hypotonia is more likely to be noted axially with normal strength and hyperactive to normal deep tendon reflexes. -

Myopathies Infosheet
The University of Chicago Genetic Services Laboratories 5841 S. Maryland Ave., Rm. G701, MC 0077, Chicago, Illinois 60637 Toll Free: (888) UC GENES (888) 824 3637 Local: (773) 834 0555 FAX: (773) 702 9130 [email protected] dnatesting.uchicago.edu CLIA #: 14D0917593 CAP #: 18827-49 Gene tic Testing for Congenital Myopathies/Muscular Dystrophies Congenital Myopathies Congenital myopathies are typically characterized by the presence of specific structural and histochemical features on muscle biopsy and clinical presentation can include congenital hypotonia, muscle weakness, delayed motor milestones, feeding difficulties, and facial muscle involvement (1). Serum creatine kinase may be normal or elevated. Heterogeneity in presenting symptoms can occur even amongst affected members of the same family. Congenital myopathies can be divided into three main clinicopathological defined categories: nemaline myopathy, core myopathy and centronuclear myopathy (2). Nemaline Myopathy Nemaline Myopathy is characterized by weakness, hypotonia and depressed or absent deep tendon reflexes. Weakness is typically proximal, diffuse or selective, with or without facial weakness and the diagnostic hallmark is the presence of distinct rod-like inclusions in the sarcoplasm of skeletal muscle fibers (3). Core Myopathy Core Myopathy is characterized by areas lacking histochemical oxidative and glycolytic enzymatic activity on histopathological exam (2). Symptoms include proximal muscle weakness with onset either congenitally or in early childhood. Bulbar and facial weakness may also be present. Patients with core myopathy are typically subclassified as either having central core disease or multiminicore disease. Centronuclear Myopathy Centronuclear Myopathy (CNM) is a rare muscle disease associated with non-progressive or slowly progressive muscle weakness that can develop from infancy to adulthood (4, 5). -

Genetic Neuromuscular Disease *
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.73.suppl_2.ii12 on 1 December 2002. Downloaded from GENETIC NEUROMUSCULAR DISEASE Mary M Reilly, Michael G Hanna ii12* J Neurol Neurosurg Psychiatry 2002;73(Suppl II):ii12–ii21 he clinical practice of neuromuscular disease is currently undergoing enormous change as a direct result of the wealth of recent molecular genetic discoveries. Indeed, the majority of gene Tdiscoveries in the area of neurological disease relate to neuromuscular disorders. The immedi- ate impact of these discoveries is that a precise DNA based diagnosis is possible. This often gives patients accurate prognostic and genetic counselling information. It will also facilitate rational screening programmes for recognised complications such as cardiac or respiratory involvement. Unfortunately, at present many eligible patients do not benefit from or have access to such diagnostic precision, although this is changing. The discovery of new genes and proteins has opened up unexplored avenues of research into therapies for neuromuscular patients. While therapeutic trials in genetic neuromuscular diseases remain in their infancy, it seems clear that a precise DNA based diagnosis will be essential. Eligi- bility for such trials and indeed for future proven therapies will be contingent upon DNA based diagnosis. For example, it is no longer acceptable to make “limb-girdle muscular dystrophy” based on simple histochemistry, a final diagnosis. Detailed immunocytochemistry and protein chemistry in combination with DNA analysis offer the patient the best chance of a precise diagnosis from which accurate prognostication, screening, and genetic counselling will follow. In this review we describe some of the more common genetic nerve and muscle diseases encountered by adult neurologists. -

Muscle Channelopathies
Muscle Channelopathies Stanley Iyadurai, MSc PhD MD Assistant Professor of Neurology, Neuromuscular Specialist, OSU, Columbus, OH August 28, 2015 24 F 9 M 18 M 23 F 16 M 8/10 Occasional “Paralytic “Seizures at “Can’t Release Headaches Gait Problems Episodes” Night” Grip” Nausea Few Seconds Few Hours “Parasomnia” “Worse in Winter” Vomiting Debilitating Few Days Full Recovery Full Recovery Video EEG Exercise – Light- Worse Sound- 1-2x/month 1-2x/year Pelvic Red Lobster Thrusting 1-2x/day 3-4/year Dad? Dad? 1-2x/year Dad? Sister Normal Exam Normal Exam Normal Exam Normal Exam Hyporeflexia Normal Exam “Defined Muscles” Photophobia Hyper-reflexia Phonophobia Migraines Episodic Ataxia Hypo Per Paralysis ADNFLE PMC CHANNELOPATHIES DEFINITION Channelopathy: a disease caused by dysfunction of ion channels; either inherited (Mendelian) or acquired/complex (Non-Mendelian, e.g., autoimmune), presenting either in neurologic or non-neurologic fashion CHANNELOPATHY SPECTRUM CHARACTERISTICS Paroxysmal Episodic Intermittent/Fluctuating Bouts/Attacks Between Attacks Patients are Usually Completely Normal Triggers – Hunger, Fatigue, Emotions, Stress, Exercise, Diet, Temperature, or Hormones Muscle Myotonic Disorders Periodic Paralysis MUSCLE CHANNELOPATHIES Malignant Hyperthermia CNS Migraine Episodic Ataxia Generalized Epilepsy with Febrile Seizures Plus Hereditary & Peripheral nerve Acquired Erythromelalgia Congenital Insensitivity to Pain Neuromyotonia NMJ Congenital Myasthenic Syndromes Myasthenia Gravis Lambert-Eaton MS Cardiac Congenital