Transient Compartment-Like Syndrome and Normokalaemic Periodic Paralysis Due to a Cav1.1 Mutation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Paramyotonia Congenita
Paramyotonia congenita Description Paramyotonia congenita is a disorder that affects muscles used for movement (skeletal muscles). Beginning in infancy or early childhood, people with this condition experience bouts of sustained muscle tensing (myotonia) that prevent muscles from relaxing normally. Myotonia causes muscle stiffness that typically appears after exercise and can be induced by muscle cooling. This stiffness chiefly affects muscles in the face, neck, arms, and hands, although it can also affect muscles used for breathing and muscles in the lower body. Unlike many other forms of myotonia, the muscle stiffness associated with paramyotonia congenita tends to worsen with repeated movements. Most people—even those without muscle disease—feel that their muscles do not work as well when they are cold. This effect is dramatic in people with paramyotonia congenita. Exposure to cold initially causes muscle stiffness in these individuals, and prolonged cold exposure leads to temporary episodes of mild to severe muscle weakness that may last for several hours at a time. Some older people with paramyotonia congenita develop permanent muscle weakness that can be disabling. Frequency Paramyotonia congenita is an uncommon disorder; it is estimated to affect fewer than 1 in 100,000 people. Causes Mutations in the SCN4A gene cause paramyotonia congenita. This gene provides instructions for making a protein that is critical for the normal function of skeletal muscle cells. For the body to move normally, skeletal muscles must tense (contract) and relax in a coordinated way. Muscle contractions are triggered by the flow of positively charged atoms (ions), including sodium, into skeletal muscle cells. The SCN4A protein forms channels that control the flow of sodium ions into these cells. -

Neuromuscular Disorders Neurology in Practice: Series Editors: Robert A
Neuromuscular Disorders neurology in practice: series editors: robert a. gross, department of neurology, university of rochester medical center, rochester, ny, usa jonathan w. mink, department of neurology, university of rochester medical center,rochester, ny, usa Neuromuscular Disorders edited by Rabi N. Tawil, MD Professor of Neurology University of Rochester Medical Center Rochester, NY, USA Shannon Venance, MD, PhD, FRCPCP Associate Professor of Neurology The University of Western Ontario London, Ontario, Canada A John Wiley & Sons, Ltd., Publication This edition fi rst published 2011, ® 2011 by Blackwell Publishing Ltd Blackwell Publishing was acquired by John Wiley & Sons in February 2007. Blackwell’s publishing program has been merged with Wiley’s global Scientifi c, Technical and Medical business to form Wiley-Blackwell. Registered offi ce: John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK Editorial offi ces: 9600 Garsington Road, Oxford, OX4 2DQ, UK The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK 111 River Street, Hoboken, NJ 07030-5774, USA For details of our global editorial offi ces, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell The right of the author to be identifi ed as the author of this work has been asserted in accordance with the UK Copyright, Designs and Patents Act 1988. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher. -
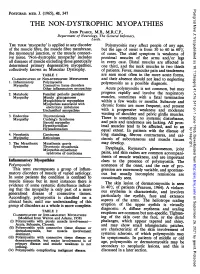
THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, the General Infirmary, Leeds
Postgrad Med J: first published as 10.1136/pgmj.41.476.347 on 1 June 1965. Downloaded from POSTGRAD. MED. J. (1965), 41, 347 THE NON-DYSTROPHIC MYOPATHIES JOHN PEARCE, M.B., M.R.C.P., Department of Neurology, The General Infirmary, Leeds. THE TERM 'myopathy' is applied to any disorder Polymyositis may affect people of any age, of the muscle fibre, the muscle fibre membrane, but the age of onset is from 30 to 60 in 60% the myoneural junction, or the muscle connect- of cases. The chief symptom is weakness of ive tissue. 'Non-dystrophic myopathy' includes proximal muscles of the arms and/or legs all diseases of muscle excluding those genetically in every case. Distal muscles are affected in determined primary degenerative myopathies, one third, and the neck muscles in two thirds collectively known as Muscular Dystrophy. of patients. Fever, muscular pain and tenderness TABLE 1 are seen most often in the more acute forms, CLASSIFICATION OF NON-DYSTROPHIC MYOPATHIES and their absence should not lead to neglecting 1. Inflammatory Polymyositis as a Myopathy Connective tissue disorders polymyositis possible diagnosis. Other inflammatory mvopathies Acute polymyositis is not common, but may 2. Metabolic Familial periodic paralysis progress rapidly and involve the respiratory Myopathy Muscle glycogenoses muscles, sometimes with a fatal termination Myoglobinuric myopathies within a few weeks or months. Myopathies associated with Subacute and electrolyte imbalance chronic forms are more frequent, and present Unclassified myopathies with a progressive weakness and moderate of shoulder 3. Endocrine Thyrotoxicosis wasting and pelvic girdle muscles. Myopathy Cushing's Syndrome There is sometimes no systemic disturbance, Steroid myopathy and pain and tenderness are lacking. -

Periodic Paralysis
Periodic Paralysis In Focus Dear Readers Fast Facts This “In Focus” report is the third in a series of MDA’s three-year commitment for all Hypokalemic periodic paralysis MDA comprehensive reports about the latest in periodic paralysis research as of March Hypokalemic PP can begin anywhere from neuromuscular disease research and manage- 2009 is $1,938,367. The Association’s early childhood to the 30s, with periodic ment. allocation for research on hyperkalemic attacks of severe weakness lasting hours This report focuses on the periodic and hypokalemic periodic paralysis to days. The frequency of attacks gener- paralyses, a group of disorders that result from research since 1950 is $8,125,341. ally lessens in the 40s or 50s. Permanent malfunctions in so-called ion channels, micro- MDA’s allocation for the recently weakness may persist between attacks, scopic tunnels that make possible high-speed identified Andersen-Tawil syndrome usually beginning in middle age and pro- movement of electrically charged particles is $515,430 since 2001. MDA is cur- gressing slowly over years. across barriers inside cells and between cells rently funding 11 grants in the periodic The most common underlying cause and their surroundings. paralyses. is any of several genetic mutations in When ion channels fail to open or close The periodic paralyses are gener- a gene on chromosome 1 that carries according to an exquisitely fine-tuned program, ally divided into hyperkalemic periodic instructions for a calcium channel protein episodes of paralysis of the skeletal muscles paralysis, hypokalemic periodic paralysis in skeletal muscle fibers. When this chan- and even temporary irregularities in the heart- and Andersen-Tawil syndrome. -

Neuromyotonia in Hereditary Motor Neuropathy J Neurol Neurosurg Psychiatry: First Published As 10.1136/Jnnp.54.3.230 on 1 March 1991
230 Journal ofNeurology, Neurosurgery, and Psychiatry 1991;54:230-235 Neuromyotonia in hereditary motor neuropathy J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.54.3.230 on 1 March 1991. Downloaded from A F Hahn, A W Parkes, C F Bolton, S A Stewart Abstract Case II2 Two siblings with a distal motor This 15 year old boy had always been clumsy. neuropathy experienced cramping and Since the age of 10, he had noticed generalised difficulty in relaxing their muscles after muscle stiffness which increased with physical voluntary contraction. Electromyogra- activity such as walking upstairs, running and phic recordings at rest revealed skating. For some time, he was aware of repetitive high voltage spontaneous elec- difficulty in releasing his grip and his fingers trical discharges that were accentuated tended to cramp on writing. He had noticed after voluntary contraction and during involuntary twitching of his fingers, forearm ischaemia. Regional neuromuscular muscles and thighs at rest and it was more blockage with curare indicated hyperex- pronounced after a forceful voluntary con- citability of peripheral nerve fibres and traction. Muscle cramping and spontaneous nerve block suggested that the ectopic muscle activity were particularly unpleasant activity originated in proximal segments when he re-entered the house in the winter, of the nerve. Symptoms were improved for example, after a game of hockey. Since the with diphenylhydantoin, carbamazepine age of twelve, he had noticed a tendency to and tocainide. trip. Subsequently he developed bilateral foot drop and weakness of his hands. He denied sensory symptoms and perspired only with The term "neuromyotonia" was coined by exertion. -

Facilitations and Hurdles of Genetic Testing in Neuromuscular Disorders
diagnostics Review Facilitations and Hurdles of Genetic Testing in Neuromuscular Disorders Andrea Barp 1,*, Lorena Mosca 2 and Valeria Ada Sansone 1 1 The NEMO Clinical Center in Milan, Neurorehabilitation Unit, University of Milan, Piazza Ospedale Maggiore 3, 20162 Milano, Italy; [email protected] 2 Medical Genetics Unit, ASST Grande Ospedale Metropolitano Niguarda, Piazza Ospedale Maggiore 3, 20162 Milano, Italy; [email protected] * Correspondence: [email protected] Abstract: Neuromuscular disorders (NMDs) comprise a heterogeneous group of disorders that affect about one in every thousand individuals worldwide. The vast majority of NMDs has a genetic cause, with about 600 genes already identified. Application of genetic testing in NMDs can be useful for several reasons: correct diagnostic definition of a proband, extensive familial counselling to identify subjects at risk, and prenatal diagnosis to prevent the recurrence of the disease; furthermore, identification of specific genetic mutations still remains mandatory in some cases for clinical trial enrollment where new gene therapies are now approaching. Even though genetic analysis is catching on in the neuromuscular field, pitfalls and hurdles still remain and they should be taken into account by clinicians, as for example the use of next generation sequencing (NGS) where many single nucleotide variants of “unknown significance” can emerge, complicating the correct interpretation of genotype-phenotype relationship. Finally, when all efforts in terms of molecular analysis have been carried on, a portion of patients affected by NMDs still remain “not genetically defined”. In the present review we analyze the evolution of genetic techniques, from Sanger sequencing to NGS, and we discuss “facilitations and hurdles” of genetic testing which must always be balanced by clinicians, Citation: Barp, A.; Mosca, L.; in order to ensure a correct diagnostic definition, but taking always into account the benefit that the Sansone, V.A. -

Identification of Gene Mutations in Patients with Primary Periodic
Luo et al. BMC Neurology (2019) 19:92 https://doi.org/10.1186/s12883-019-1322-6 RESEARCH ARTICLE Open Access Identification of gene mutations in patients with primary periodic paralysis using targeted next-generation sequencing Sushan Luo1†, Minjie Xu2†, Jian Sun1, Kai Qiao3, Jie Song1, Shuang Cai1, Wenhua Zhu1, Lei Zhou1, Jianying Xi1, Jiahong Lu1, Xiaohua Ni2, Tonghai Dou4 and Chongbo Zhao1,5* Abstract Background: Primary periodic paralysis is characterized by recurrent quadriplegia typically associated with abnormal serum potassium levels. The molecular diagnosis of primary PP previously based on Sanger sequencing of hot spots or exon-by-exon screening of the reported genes. Methods: We developed a gene panel that includes 10 ion channel-related genes and 245 muscular dystrophy- and myopathy-related genes and used this panel to diagnose 60 patients with primary periodic paralysis and identify the disease-causing or risk-associated gene mutations. Results: Mutations of 5 genes were discovered in 39 patients (65.0%). SCN4A, KCNJ2 and CACNA1S variants accounted for 92.5% of the patients with a genetic diagnosis. Conclusions: Targeted next-generation sequencing offers a cost-effective approach to expand the genotypes of primary periodic paralysis. A clearer genetic profile enables the prevention of paralysis attacks, avoidance of triggers and the monitoring of complications. Keywords: Primary periodic paralysis, Targeted next-generation sequencing, Gene panel, Gene mutation distribution, Calcium homeostasis. Background (SCN4A) and potassium voltage-gated channel subfamily Periodic paralysis (PP) is characterized by episodes of J member 2 (KCNJ2), that encode voltage-gated chan- muscle weakness that occur at irregular intervals due to nels in muscle membranes that generate or sustain skeletal muscle ion channelopathies. -

What Is a Skeletal Muscle Channelopathy?
Muscle Channel Patient Day 2019 Dr Emma Matthews The Team • Professor Michael Hanna • Emma Matthews • Doreen Fialho - neurophysiology • Natalie James – clinical nurse specialist • Sarah Holmes - physiotherapy • Richa Sud - genetics • Roope Mannikko – electrophysiology • Iwona Skorupinska – research nurse • Louise Germain – research nurse • Kira Baden- service manager • Jackie Kasoze-Batende– NCG manager • Jean Elliott – NCG senior secretary • Karen Suetterlin, Vino Vivekanandam • – research fellows What is a skeletal muscle channelopathy? Muscle and nerves communicate by electrical signals Electrical signals are made by the movement of positively and negatively charged ions in and out of cells The ions can only move through dedicated ion channels If the channel doesn’t work properly, you have a “channelopathy” Ion channels CHLORIDE CHANNELS • Myotonia congenita – CLCN1 • Paramyotonia congenita – SCN4A MYOTONIA SODIUM CHANNELS • Hyperkalaemic periodic paralysis – SCN4A • Hypokalaemic periodic paralysis – 80% CACNA1S CALCIUM CHANNELS – 10% SCN4A PARALYSIS • Andersen-Tawil Syndrome – KCNJ2 POTASSIUM CHANNELS Myotonia and Paralysis • Two main symptoms • Paralysis = an inexcitable muscle – Muscles are very weak or paralysed • Myotonia = an overexcited muscle – Muscle keeps contracting and become “stuck” - Nerve action potential Cl_ - + - + + + Motor nerve K+ + Na+ Na+ Muscle membrane Ach Motor end plate T-tubule Nav1.4 Ach receptors Cav1.1 and RYR1 Muscle action potential Calcium MuscleRelaxed contraction muscle Myotonia Congenita • Myotonia -

Cerebral Hypotonia by Mihee Bay MD (Dr
Cerebral hypotonia By Mihee Bay MD (Dr. Bay of Kennedy Krieger Institute and Johns Hopkins School of Medicine has no relevant financial relationships to disclose.) Originally released July 12, 2006; last updated February 1, 2016; expires February 1, 2019 Introduction This article includes discussion of cerebral hypotonia, central hypotonia, essential hypotonia, benign congenital hypotonia, and floppy infant. The foregoing terms may include synonyms, similar disorders, variations in usage, and abbreviations. Overview Hypotonia is a clinical manifestation of numerous diseases affecting the central and/or peripheral motor nervous system. The key to accurate diagnosis involves integral steps of evaluation that include a detailed history, examination, and diagnostic tests. “Cerebral” (or central) hypotonia implies pathogenesis from abnormalities from the central nervous system, and related causal disorders include cerebral dysgenesis and genetic or metabolic disorders. Patients with central hypotonia generally have hypotonia without associated weakness, in contrast to the peripheral (lower motor neuron) causes, which typically produce both hypotonia and muscle weakness. Hypotonia is a clinical manifestation of over 500 genetic disorders; thus, a logical, stepwise approach to diagnosis is essential. With recent advances in the field of genetic testing, diagnostic yield will undoubtedly improve. There is no cure, but treatment includes supportive therapies, such as physical and occupational therapy, and diagnosis-specific management. Key points • Hypotonia is reduced tension or resistance of passive range of motion. • The first step in the evaluation of a child with hypotonia is localization to the central (“cerebral”) or peripheral nervous system, or both. • Central hypotonia is more likely to be noted axially with normal strength and hyperactive to normal deep tendon reflexes. -

Ion Channels: Structural Basis for Function and Disease
UC Irvine UC Irvine Previously Published Works Title Ion channels: structural basis for function and disease. Permalink https://escholarship.org/uc/item/39x307jx Journal Seminars in perinatology, 20(6) ISSN 0146-0005 Author Goldstein, SA Publication Date 1996-12-01 DOI 10.1016/s0146-0005(96)80066-8 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Ion Channels: Structural Basis for Function and Disease Steve A. N. Goldstein Ion channels are ubiquitous proteins that mediate nervous and muscular function, rapid transmem- brane signaling events, and ionic and fluid balance. The cloning of genes encoding ion channels has led to major strides in understanding the mechanistic basis for their function. These advances have shed light on the role of ion channels in normal physiology, clarified the molecular basis for an expanding number of diseases, and offered new direction to the development of rational therapeutic interventions. Copyright 1996 by W.B. Saunders Company on channels reside in the membranes of all by ion channels to be divided into two broad cells and control their electrical activity. 1 mechanistic groups: those resulting from loss of These proteins underlie subtle biological events channel function and those consequent to gain such as the response of a single rod cell to a of channel function. Three exemplary patho- beam of light, the activation of a T cell by its physiological correlates are examined, Long QT antigen, and the fast block to polyspermy of a syndrome, Liddle's syndrome and pseudohypo- fertilized ovum. -

Gain-Of-Function Mutation in Nav 1.7 in Familial Erythromelalgia Induces Bursting of Sensory Neurons
Gain-of-function mutation in Nav 1.7 in familial erythromelalgia induces bursting of sensory neurons S. D. Dib-Hajj,1,2,3 A. M. Rush,1,2,3 T. R. Cummins,4 F. M. Hisama,1 S. Novella,1 L. Tyrrell,1,2,3, L. Marshall1 and S. G. Waxman1,2,3 1Department of Neurology and 2Center for Neuroscience and Regeneration Research, Yale University School of Medicine, New Haven, 3Rehabilitation Research Center, VA Connecticut Healthcare System, West Haven, CT and 4Department of Pharmacology and Toxicology, Stark Neurosciences Institute, Indiana University School of Medicine, Indianapolis, IN, USA Correspondence to: Stephen G. Waxman, MD, PhD, Department of Neurology, LCI 707, Yale School of Medicine, 333 Cedar Street, New Haven, CT 06510, USA E-mail: [email protected] Erythromelalgia is an autosomal dominant disorder characterized by burning pain in response to warm stimuli or moderate exercise. We describe a novel mutation in a family with erythromelalgia in SCN9A, the gene that encodes the Nav1.7 sodium channel. Nav1.7 produces threshold currents and is selectively expressed within sensory neurons including nociceptors. We demonstrate that this mutation, which produces a hyperpolarizing shift in activation and a depolarizing shift in steady-state inactivation, lowers thresholds for single action potentials and high frequency firing in dorsal root ganglion neurons. Erythromelalgia is the first inherited pain disorder in which it is possible to link a mutation with an abnormality in ion channel function and with altered firing of pain signalling neurons. Keywords: channel; channelopathy; erythromelalgia; mutation; pain; sodium Abbreviations: DRG = dorsal root ganglion Received January 25, 2005. -

Severe Infantile Hyperkalaemic Periodic Paralysis And
1339 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.74.9.1339 on 21 August 2003. Downloaded from SHORT REPORT Severe infantile hyperkalaemic periodic paralysis and paramyotonia congenita: broadening the clinical spectrum associated with the T704M mutation in SCN4A F Brancati, E M Valente, N P Davies, A Sarkozy, M G Sweeney, M LoMonaco, A Pizzuti, M G Hanna, B Dallapiccola ............................................................................................................................. J Neurol Neurosurg Psychiatry 2003;74:1339–1341 the face and hand muscles, and paradoxical myotonia. Onset The authors describe an Italian kindred with nine individu- of paramyotonia is usually at birth.2 als affected by hyperkalaemic periodic paralysis associ- HyperPP/PMC shows characteristics of both hyperPP and ated with paramyotonia congenita (hyperPP/PMC). PMC with varying degrees of overlap and has been reported in Periodic paralysis was particularly severe, with several association with eight mutations in SCN4A gene (I693T, episodes a day lasting for hours. The onset of episodes T704M, A1156T, T1313M, M1360V, M1370V, R1448C, was unusually early, beginning in the first year of life and M1592V).3–9 While T704M is an important cause of isolated persisting into adult life. The paralytic episodes were hyperPP, this mutation has been only recently described in a refractory to treatment. Patients described minimal single hyperPP/PMC family. As with other SCN4A mutations, paramyotonia, mainly of the eyelids and hands. All there can be marked intrafamilial and interfamilial variability affected family members carried the threonine to in paralytic attack frequency and severity in patients harbour- methionine substitution at codon 704 (T704M) in exon 13 ing T704M.10–12 We report an Italian kindred, in which all of the skeletal muscle voltage gated sodium channel gene patients presented with an unusually severe and homogene- (SCN4A).