New Medicines for Type 2 Diabetes 4
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Think Medicines!
Think Issue 13 August 2016 MHRA Drug Safety SGLT2 inhibitors: updated advice on the risk of diabetic Medicines!Updates can be found ketoacidosis (DKA) at the following link. The MHRA are advising health care professionals to test for raised ketones in patients with ketoacidosis symptoms, who are taking SGLT2 inhibitors even if New higher strength Humalog® plasma glucose levels are near-normal. SGLT2 inhibitors include: Canagliflozin, 200 units/ml KwikPen™ Dapagliflozin and Empagliflozin. Serious, life-threatening, and fatal cases of In order to minimize medication DKA have been reported in patients taking an SGLT2 inhibitor. In several cases, errors. blood glucose levels were only moderately elevated (e.g. <14mmol/L) Insulin lispro 200 units/ml representing an atypical presentation for DKA, which could delay diagnosis and solution for injection should treatment. ONLY be administered using the Advice for health Care Professionals: Humalog 200 units/ml pre-filled Inform patients of the signs of diabetic ketoacidosis (DKA) and advise them to pen (KwikPen). seek immediate medical advice if they develop any of these symptoms (e.g. When switching from one rapid weight loss, feeling sick or being sick, stomach pain, fast and deep Humalog strength to another, breathing, sleepiness, a sweet smell to the breath, a sweet or metallic taste in the dose does not need to be the mouth, or a different odour to urine or sweat). converted. Unnecessary dose Discuss the risk factors of DKA with patients. conversion may lead to under/ Discontinue treatment with the SGLT2 inhibitor immediately if DKA is over dosing and resultant hyper/ suspected or diagnosed. -

IHS PROVIDER September 2017
September 2017 Volume 42 Number 9 Indian Health Service National Pharmacy and Therapeutics Committee SGLT-2 inhibitors (Update) NPTC Formulary Brief August Meeting 2017 Background: The FDA has currently approved three SGLT-2 inhibitors, two of which have completed FDA-mandated cardiovascular outcomes trials. Last year, in the Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients (EMPA-REG), empagliflozin not only reduced cardiovascular events, but also mortality.1 This year, the Canagliflozin Cardiovascular Assessment Study (CANVAS) demonstrated equivocal cardiovascular benefits, no mortality benefit, and significant harms in those receiving canagliflozin.2 The DECLARE-TIMI 58 cardiovascular study of dapagliflozin will be completed in April 2019 (ClinicalTrials.gov Identifier: NCT01730534). Uncertainty remains regarding the current data, long- term benefits and harms, and differentiation among SGLT-2 inhibitors. Following a review of SGLT2 inhibitors at the August 2017 NPTC meeting on their cardiovascular outcomes, net benefit and place in therapy, no modifications were made to the National Core Formulary (NCF). Discussion: EMPA-REG enrolled 7,020 patients with Type 2 diabetes mellitus (T2DM) and HgbA1c values between 7.0-10.0%. All patients had established cardiovascular disease (CVD) and were observed for a median duration of 3.1 years. Empagliflozin reduced the primary outcome of cardiovascular (CV) death, nonfatal myocardial infarction (MI), or nonfatal cardiovascular accident (CVA) by 6.5 events per 1000 patient-years (pt-yrs). Mortality decreased by 9.2 events per 1000 pt-yrs, primarily driven by a reduction in CV mortality of 7.8 events per 1000 pt-yrs. Heart failure hospitalization decreased by 5.1 events per 1000 pt-yrs. -

Step Therapy
UnitedHealthcare Pharmacy Clinical Pharmacy Programs Program Number 2020 P 3086-9 Program Step Therapy – Diabetes Medications - SGLT2 Inhibitors Medication Farxiga (dapagliflozin)*, Glyxambi (empagliflozin/linagliptan), Invokana (canagliflozin)*, Invokamet (canagliflozin/metformin)*, Invokamet XR (canaglifloxin/metformin extended-release)*, Jardiance (empagliflozin), Qtern (dapagliflozin/saxagliptin)*, Segluromet (ertugliflozin/metformin)*, Steglatro (ertugliflozin)*, Steglujan (ertugliflozin/sitagliptin)*, Xigduo XR (dapagliflozin/metformin extended-release)* P&T Approval Date 10/2016, 10/2017, 4/2018, 8/2018, 12/2018, 2/2019, 2/2020, 5/2020; 7/2020 Effective Date 10/1/2020; Oxford only: 10/1/2020 1. Background: Farxiga (dapagliflozin)*, Invokana (canagliflozin)*, Jardiance (empagliflozin) and Steglatro (ertugliflozin)* are sodium-glucose co-transporter 2 (SGLT2) inhibitors indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Farxiga*, Invokana* and Jardiance have additional indications. Farxiga* is indicated to reduce the risk of cardiovascular death and hospitalization for heart failure in adults with heart failure (NYHA class II-IV) with reduced ejection fraction. Invokana* is indicated to reduce the risk of major adverse cardiovascular events (cardiovascular death, nonfatal myocardial infarction and nonfatal stroke) in adults with type 2 diabetes mellitus and established cardiovascular disease (CVD), and to reduce the risk of end-stage kidney disease (ESKD), doubling of -

Ertugliflozin 5Mg, 15Mg Film-Coated Tablet (Steglatro®) Merck Sharp & Dohme
1 www.scottishmedicines.org.uk SMC2102 ertugliflozin 5mg, 15mg film-coated tablet (Steglatro®) Merck Sharp & Dohme 7 December 2018 The Scottish Medicines Consortium (SMC) has completed its assessment of the above product and advises NHS Boards and Area Drug and Therapeutic Committees (ADTCs) on its use in NHSScotland. The advice is summarised as follows: ADVICE: following a full submission ertugliflozin (Steglatro®) is accepted for restricted use within NHSScotland. Indication under review: in adults aged 18 years and older with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control: As monotherapy in patients for whom the use of metformin is considered inappropriate due to intolerance or contraindications. In addition to other medicinal products for the treatment of diabetes. SMC restriction: ertugliflozin is accepted for use as monotherapy and as add-on therapy. When used as monotherapy it is restricted to patients who would otherwise receive a dipeptidyl peptidase-4 inhibitor and in whom a sulphonylurea or pioglitazone is not appropriate. Ertugliflozin was superior to placebo in lowering HbA1c in adults with type 2 diabetes mellitus in phase III studies in monotherapy, dual therapy and triple therapy settings. Chairman Scottish Medicines Consortium Published 14 January 2019 1 Indication In adults aged 18 years and older with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control: As monotherapy in patients for whom the use of metformin is considered inappropriate due to intolerance or contraindications. In addition to other medicinal products for the treatment of diabetes.1 Dosing Information The recommended starting dose is 5mg orally once daily which can, if tolerated, be increased to 15mg once daily if additional glycaemic control is needed. -

SGLT2) Inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM
Sodium-glucose cotransporter-2 (SGLT2) inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM) There are currently four SGLT2 inhibitors (canagliflozin, dapagliflozin, empagliflozin and ertugliflozin) licensed in the UK for the management of adults with T2DM. No head to head trials between the SGLT2 inhibitors have been conducted. As at December 2019, clinical outcome data is available for three of the four SGLT2 inhibitors around their cardiovascular effects in people with T2DM. Ertugliflozin is still to report on this data. This document summarises the key prescribing considerations. NICE Technology Appraisal Recommendation NICE makes recommendations for when SGLT2 inhibitors can be considered in adults with T2DM; Hertfordshire Medicines Management Committee Recommendations are in line with NICE guidance: Monotherapy NICE TA 390: Canagliflozin, Dapagliflozin and Empagliflozin and NICE TA 572: Ertugliflozin as monotherapies for treating T2DM Monotherapy recommended as option in adults for whom metformin is contraindicated or not tolerated and when diet & exercise alone do not provide adequate glycaemic control, only if: •a DPP‑4 inhibitor would otherwise be prescribed and •a sulfonylurea or pioglitazone is not appropriate. Dual therapy NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin, TA 572: Ertugliflozin as combination therapies for treating T2DM In a dual therapy regimen in combination with metformin is recommended as an option, only if: •a sulfonylurea is contraindicated or not tolerated or •the person is at significant risk of hypoglycaemia or its consequences. In combination with insulin NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin in combination with insulin with or without other antidiabetic drugs is recommended as an option. -

SGLT2 Inhibitors in Combination Therapy: from Mechanisms To
Diabetes Care Volume 41, August 2018 1543 Michael¨ J.B. van Baar, SGLT2 Inhibitors in Combination Charlotte C. van Ruiten, Marcel H.A. Muskiet, Therapy: From Mechanisms to Liselotte van Bloemendaal, Richard G. IJzerman, and PERSPECTIVES IN CARE Clinical Considerations in Type 2 Daniel¨ H. van Raalte Diabetes Management Diabetes Care 2018;41:1543–1556 | https://doi.org/10.2337/dc18-0588 The progressive nature of type 2 diabetes (T2D) requires practitioners to periodically evaluate patients and intensify glucose-lowering treatment once glycemic targets are not attained. With guidelines moving away from a one-size-fits-all approach toward setting patient-centered goals and allowing flexibility in choosing a second-/ third-line drug from the growing number of U.S. Food and Drug Administration– approved glucose-lowering agents, keen personalized management in T2D has become a challenge for health care providers in daily practice. Among the newer generation of glucose-lowering drug classes, sodium–glucose cotransporter 2 inhibitors (SGLT2is), which enhance urinary glucose excretion to lower hyper- glycemia, have made an imposing entrance to the T2D treatment armamentarium. Given their unique insulin-independent mode of action and their favorable efficacy– to–adverse event profile and given their marked benefits on cardiovascular-renal outcome in moderate-to-high risk T2D patients, which led to updates of guidelines and product monographs, the role of this drug class in multidrug regimes is promising. However, despite many speculations based on pharmacokinetic and pharmacodynamic properties, physiological reasoning, and potential synergism, the effects of these agents in terms of glycemic and pleiotropic efficacy when combined with other glucose-lowering drug classes are largely understudied. -
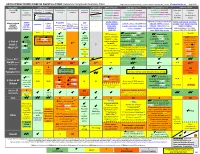
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Color Outcomes Comparison Summary Table
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Outcomes Comparison Summary Table L Regier BSP BA, M LeBras PharmD, T Trischuk PharmD, J Bareham BSP, L Lu BSP © www.RxFiles.ca Aug 2021 Drug Class Sulfonylureas TZDs Meglitinides DPP4 Inhibitors GLP1 Agonists *** SGLT2 Inhibitors *** Insulin in T2DM Generic Metformin Gliclazide Glyburide Pioglitazone Rosiglitazone Acarbose Repaglinide Saxagliptin ONGLYZA Liraglutide VICTOZA Empagliflozin JARDIANCE Intensity: Intensity: BRAND (MF) DIAMICRON DIABETA ACTOS, g AVANDIA GLUCOBAY GLUCONORM Sitagliptin JANUVIA Exenatide BYETTA, BYDUREON Canagliflozin INVOKANA Less More GLUCOPHAGE Dulaglutide TRULICITY Dapagliflozin FORXIGA, FARXIGA Alogliptin NESINA (e.g. NPH (Multiple daily GLUCOTROL D/C STEGLATRO Glipizide Nateglinide Semaglutide OZEMPIC, RYBELSUS (PO) Ertugliflozin Linagliptin TRAJENTA HS + MF) doses) STARLIX D/C SPREAD-DIMCAD] Lixisenatide ADLYXINE; ALBIGLUTIDE D/C SAVOR-TIMI 53, EMPA-REG, CANVAS, CREDENCE, T2DM: UKPDS-33,80; ADVANCE, Major trials to UKPDS- ProACTIVE ACE 33,34,80 UKPDS- Meta-analysis. TECOS, EXAMINE LEADER, EXSCEL, FREEDOM CVO, DECLARE, VERTIS-CV (2020), ACCORD, VADT, ORIGIN, DEVOTE support ADVANCE (Prevention (ADOPT; 33,80 Ferwana M. Meta- RECORD interim, PROLOGUE, REWIND, SUSTAIN-6, PIONEER-6, DAPA-HF, DAPA-CKD (2020), T1DM: DCCT/EDIC findings/ analysis 2013. trial: Stop- - some use in (ADOPT) ADOPT, DREAM CARMELINA, EMPEROR-Reduced & -Preserved (Also Boussageon et al. Meta- Outcomes* ADVANCE) SR-Liao 2017; IRIS NIDDM) ELIXA, HARMONY CAROLINA (2020), EMPA-Kidney (2022) analysis. -

Cost-Effectiveness of Empagliflozin Versus Canagliflozin, Dapagliflozin
Emerging technologies, pharmacology and therapeutics Open access Original research BMJ Open Diab Res Care: first published as 10.1136/bmjdrc-2020-001313 on 3 May 2021. Downloaded from Cost-effectivenessofempagliflozin versuscanagliflozin,dapagliflozin,or standardofcareinpatientswithtype2 diabetesandestablished cardiovasculardisease Odette S Reifsnider ,1 Anuraag R Kansal,1 Pranav K Gandhi,2 Lael Cragin,1 Sarah B Brand,1 Egon Pfarr,3 Kyle Fahrbach,4 Anastasia Ustyugova3 To cite: Reifsnider OS, ABSTRACT Kansal AR, Gandhi PK, Introduction Empagliflozin, a sodium- glucose co- Significance of this study et al. Cost- effectiveness transporter-2 (SGLT-2) inhibitor, is approved in the USA of empagliflozin versus to reduce risk of cardiovascular (CV) death in adults What is already known about this subject? canagliflozin, dapagliflozin, with type 2 diabetes mellitus (T2DM) and established CV ► The sodium glucose co- transporter-2 inhibitor (SGLT- or standard of care in 2) empagliflozin is Food and Drug Administration patients with type 2 disease, based on EMPA-REG OUTCOME (Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes (FDA) approved to reduce the risk of cardiovascular diabetes and established (CV) death in adults with type 2 diabetes mellitus cardiovascular disease. Mellitus Patients) trial results. Empagliflozin reduced major (T2DM) and established CV disease (CVD) based BMJ Open Diab Res Care adverse CV event (MACE) by 14%, CV death by 38%, and 2021;9:e001313. doi:10.1136/ hospitalization for heart failure (HHF) by 35% vs placebo, on the EMPA- REG OUTCOME trial, which showed a bmjdrc-2020-001313 each on top of standard of care (SoC). -

The Na+/Glucose Cotransporter Inhibitor Canagliflozin Activates
2784 Diabetes Volume 65, September 2016 Simon A. Hawley,1 Rebecca J. Ford,2 Brennan K. Smith,2 Graeme J. Gowans,1 Sarah J. Mancini,3 Ryan D. Pitt,2 Emily A. Day,2 Ian P. Salt,3 Gregory R. Steinberg,2 and D. Grahame Hardie1 The Na+/Glucose Cotransporter Inhibitor Canagliflozin Activates AMPK by Inhibiting Mitochondrial Function and Increasing Cellular AMP Levels Diabetes 2016;65:2784–2794 | DOI: 10.2337/db16-0058 Canagliflozin, dapagliflozin, and empagliflozin, all recently transporters that carry glucose across apical membranes approved for treatment of type 2 diabetes, were derived of polarized epithelial cells against concentration gradi- from the natural product phlorizin. They reduce hypergly- ents, driven by Na+ gradients. SGLT1 is expressed in the cemia by inhibiting glucose reuptake by sodium/glucose small intestine and responsible for most glucose uptake cotransporter (SGLT) 2 in the kidney, without affecting across the brush border membrane of enterocytes, whereas intestinal glucose uptake by SGLT1. We now report that SGLT2 is expressed in the kidney and responsible for most fl canagli ozin also activates AMPK, an effect also seen glucose readsorption in the convoluted proximal tubules. with phloretin (the aglycone breakdown product of The first identified SGLT inhibitor was a natural product, fi phlorizin), but not to any signi cant extent with dapagli- phlorizin, which is broken down in the small intestine to flozin, empagliflozin, or phlorizin. AMPK activation oc- phloretin, the aglycone form (Fig. 1). Although phlorizin curred at canagliflozin concentrations measured in had beneficial effects in hyperglycemic animals (2), it in- human plasma in clinical trials and was caused by hibits SGLT1 and SGLT2, causing adverse gastrointestinal inhibition of Complex I of the respiratory chain, leading effects (3). -

The Combination of Canagliflozin with a Half-Dose of Glimepiride
Harada et al. Int J Diabetes Clin Res 2016, 3:065 Volume 3 | Issue 3 International Journal of ISSN: 2377-3634 Diabetes and Clinical Research Original Article: Open Access The Combination of Canagliflozin with a Half-Dose of Glimepiride Improves Glycemic Control and Blood Glucose Perturbation without Increasing the Risk of Hypoglycemia and Ketosis Mayuko Harada, Yasuhisa Abe, Yuki Maeda, Michiko Kajikawa, and Mitsuru Hashiramoto* Division of Diabetes and Endocrinology, Yodogawa Christian Hospital, Japan *Corresponding author: Mitsuru Hashiramoto, MD, PhD, Division of Diabetes and Endocrinology, Yodogawa Christian Hospital, 1-7-50 Kuni-Jima, Higashi-Yodogawa-Ku, Osaka 533-0024, Japan, Tel: +81-6-6322-2259, Fax: +81-6-6-6320-6308, E-mail: [email protected] Abstract Introduction Aim: To evaluate the efficacy and safety of administering The application of sulfonylurea (SU) remains one of the most canagliflozin to Japanese type 2 diabetes mellitus (T2DM) patients popular approaches in pharmacological therapy for type 2 diabetes and reducing the dosage of their existing regimen of sulfonylurea mellitus (T2DM) patients because SU exerts potent stimulatory (SU) by half. effects on insulin secretion from pancreatic β cells and is relatively Methods: Seventeen Japanese T2DM patients on antidiabetes inexpensive and well tolerated. Hypoglycemia, however, is a major medication (SU) completed this 12-week prospective single-arm safety concern that is associated with the use of SUs, because it open-label study. First, the dose of SU was reduced by half and impairs a patient's quality of life and can become life threatening a concomitant administration of canagliflozin (100 mg/day) was initiated. -

Canagliflozin: a Novel Agent for the Treatment of Type 2 Diabetes Mellitus Correspondence Course Program Number: 0171-9999-13-072-H01-P 1
CE Canagliflozin: A Novel Agent for the Treatment of Type 2 Diabetes Mellitus By Marquita D. Bradshaw, Pharm.D., BCACP and Rikki L. Tonet, Pharm.D. Candidate 2014 Objectives INTRODUCTION • Describe the pathophysiological defects in Type 2 T2DM is one of the four clinical classes of diabetes Diabetes Mellitus (T2DM) incorporated in the omi- identified which results from a progressive insulin nous octet secretory defect on the background of insulin re- • Describe the mechanism of action of canagliflozin sistance.2 Signs and symptoms of T2DM include • Identify the potential place in therapy of cana- polyuria, polydipsia, and polyphagia which may not gliflozin be overt. Often patients with T2DM are not diag- • Summarize patient counseling points when dispens- nosed until complications appear; therefore resulting ing canagliflozin in subsequent reduction in quality of life if diabetes • Identify available strengths of canagliflozin (Phar- remains uncontrolled. macy technicians***) Approximately 25.8 million children and adults in Conflict of interest statement: There is no conflict the United States are living with diabetes, including 7 of interest involved in writing this article or in the million who are currently undiagnosed.3 This equates subject matter of this article. to 8.3% of the population in the United States. In 2010, South Carolina had the fifth highest prevalence Abstract: Several oral and injectable agents are of diabetes in the nation.4 The prevalence of diabetes available for the treatment of Type 2 Diabetes Melli- in South Carolina is presently 9.6% and has increased tus (T2DM). A recent consensus statement published more rapidly than the national rate.4 by the American Diabetes Association emphasizes a patient-centered approach.1 Canagliflozin belongs Previously it was thought that a triumvirate was to a novel therapeutic class. -

INVOKAMET (Canagliflozin and Metformin Hydrochloride)
HIGHLIGHTS OF PRESCRIBING INFORMATION ---------------------------WARNINGS AND PRECAUTIONS------------------- These highlights do not include all the information needed to use • Lactic acidosis: Warn against excessive alcohol use. INVOKAMET is not INVOKAMET® safely and effectively. See full prescribing information recommended in hepatic impairment or hypoxic states. Ensure normal renal for INVOKAMET. function before initiating and at least annually thereafter (5.1, 5.4, 5.7, 5.13, 5.14) INVOKAMET (canagliflozin and metformin hydrochloride) tablets, for • Hypotension: Before initiating INVOKAMET, assess volume status and oral use correct hypovolemia in patients with renal impairment, the elderly, in Initial U.S. Approval – 2014 patients with low systolic blood pressure, or on diuretics, ACEi, or ARB. Monitor for signs and symptoms during therapy (5.2) WARNING: LACTIC ACIDOSIS • Ketoacidosis: Assess patients who present with signs and symptoms of metabolic acidosis for ketoacidosis, regardless of blood glucose level. If See full prescribing information for complete boxed warning. suspected, discontinue INVOKAMET, evaluate and treat promptly. Before initiating INVOKAMET, consider risk factors for ketoacidosis. Patients on • Lactic acidosis can occur due to metformin accumulation. The risk INVOKAMET may require monitoring and temporary discontinuation of increases with conditions such as renal impairment, sepsis, therapy in clinical situations known to predispose to ketoacidosis (5.3) dehydration, excess alcohol intake, hepatic impairment,