Program, We Have Added a Few New Themes to the Program, Increasing the Number of These Concurrent Sessions to 12 in 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Treatment of ARDS*
Treatment of ARDS* Roy G. Brower, MD; Lorraine B. Ware, MD; Yves Berthiaume, MD; and Michael A. Matthay, MD, FCCP Improved understanding of the pathogenesis of acute lung injury (ALI)/ARDS has led to important advances in the treatment of ALI/ARDS, particularly in the area of ventilator- associated lung injury. Standard supportive care for ALI/ARDS should now include a protective ventilatory strategy with low tidal volume ventilation by the protocol developed by the National Institutes of Health ARDS Network. Further refinements of the protocol for mechanical ventilation will occur as current and future clinical trials are completed. In addition, novel modes of mechanical ventilation are being studied and may augment standard therapy in the future. Although results of anti-inflammatory strategies have been disappointing in clinical trials, further trials are underway to test the efficacy of late corticosteroids and other approaches to modulation of inflammation in ALI/ARDS. (CHEST 2001; 120:1347–1367) Key words: acute lung injury; mechanical ventilation; pulmonary edema; ventilator-associated lung injury Abbreviations: ALI ϭ acute lung injury; APRV ϭ airway pressure-release ventilation; ECco R ϭ extracorporeal ϭ ϭ 2 carbon dioxide removal; ECMO extracorporeal membrane oxygenation; Fio2 fraction of inspired oxygen; HFV ϭ high-frequency ventilation; I:E ϭ ratio of the duration of inspiration to the duration of expiration; IL ϭ interleukin; IMPRV ϭ intermittent mandatory pressure-release ventilation; IRV ϭ inverse-ratio ventilation; LFPPV ϭ low-frequency positive-pressure ventilation; NIH ϭ National Institutes of Health; NIPPV ϭ noninvasive positive-pressure ventilation; NO ϭ nitric oxide; PEEP ϭ positive end-expiratory pressure; PSB ϭ protected specimen brushing; TGI ϭ tracheal gas insufflation; TNF ϭ tumor necrosis factor he syndrome of acute respiratory distress in Standard Supportive Therapy T adults was first described in 1967.1 Until re- cently, most reported mortality rates exceeded 50%. -

RSC 2018 Seminar Bios
Royal Society of Canada Eastern Ontario Regional Seminar Saturday, April 14, 2018, Queen’s University Club, 168 Stuart St, Kingston, ON All Presentations are Free and Open to the Public 10:00 am: Peter Milliken: The Role of the Speaker of the House of Commons Peter Milliken was born in Kingston and after high school he attended Queen’s University beginning in 1964 studying Politics and Economics. He graduated in 1968 and went to Oxford University to study law where he earned a B.A. in 1970 then went to Dalhousie University to get an LL.B. in 1971. He practiced law in Kingston after his call to the Bar in 1973 until 1988 when he was elected M.P. for Kingston and the Islands. He served in the House of Commons until 2011 as M.P. and was Deputy Speaker from 1996 until 2000 and was elected Speaker in 2001 and reelected in 2004, 2006 and 2008 and served until his retirement in 2011. Milliken also has the unique distinction of being the first Speaker to preside over four Parliaments. His legacy includes his landmark rulings on Parliament’s right to information, which are key elements of parliamentary precedent both in Canada and throughout the Commonwealth. He currently resides in Kingston enjoying retirement. 11:00 am: Stéphanie Bélanger: War Trauma, Culture of War and Soldier Identity Dr. Bélanger is the Associate Scientific Director of the Canadian Institute for Military and Veteran Health Research, a unique consortium of 43 Canadian universities dedicated to researching the health needs of military personnel, Veterans and their families. -

BIOM 6070 – Pregnancy, Birth and Perinatal Adaptation Spring/Summer 2016 University of Guelph (Seminar Course Only)
Page 1 of 3 PREGNANCY: Graduate Course 2016 BMED 829 – Pregnancy, Queen’s University (Seminar and Laboratory Course) Meeting in Videoconference Room 155 at the School of Medicine (SoM) or as announced BIOM 6070 – Pregnancy, Birth and Perinatal Adaptation Spring/Summer 2016 University of Guelph (Seminar Course only). Meeting in videoconference room-location to be announced Course Coordinators Queen’s University: Dr. Anne Croy, DVM, PhD. ([email protected])-seminars B924 Dr. Chandra Tayade, DVM, PhD. ([email protected])-laboratory B860 University of Guelph: Dr. Jon LaMarre, DVM, PhD. ([email protected])-seminars OVC 3606 Dr. Rami Kridli, DVM, PhD. ([email protected]) OVC 2602 Clinical Participants: Dr. Graeme Smith, Department of Obstetrics and Gynecology, [email protected] Dr. Michael Flavin, Department of Pediatrics, [email protected] University of Guelph Scheduler: Ms. Kim Best, Secretary, Dept. Biomedical Sciences [email protected] Videoconference Support: Queens: [email protected] U. Guelph: Jim Hare [email protected] or [email protected] Part I of the Course: A Literature Review and Discussion Based Component Tuesday May 3 First Class Meeting – 9.30 – 10.30 – Videoconferene Room 155 SoM, Queen’s Guelph & Queen’s University linked with Ontario Veterinary College PATH4838 Reading List Topic #1 assigned. Discuss grant writing elective topic task, value of memberships in learned societies. Thursday, May 5 Queen’s Grand Rounds, Obstetrics and Gynecology with Reproduction Research Group. ONLY. Room to be announced. 7:30-8:30 AM. Guest Dr. Kelle Moley, James P. Crane Professor of Obstetrics and Gynecology; Director of the Division of Basic Science Research, Department of Obstetrics and Gynecology, Washington University, St. -

DBMS Graduate Program Proposal
NEW GRADUATE PROGRAM PROPOSAL Submission Form This template is to be used when seeking approval for new Graduate programs of study leading to a degree. New program submissions must receive the approval of the Graduate Studies Executive Council (GSEC) prior to being externally reviewed. The submission, external review, and the internal response to the review will, as a package, be submitted by GSEC to the Senate Office for referral to the Senate Committee on Academic Development (SCAD) which will then make their recommendations to Senate. Academic Units are strongly advised to contact the Director of the Office of the Vice-Provost and Dean SGS or the appropriate Associate Dean in the SGS with any questions that arise during this proposal development. Refer also to the QUQAP website at: http://www.queensu.ca/provost/responsibilities/qualityassurance.html. NOTE: the textboxes in this template will expand as needed. Part A – General Summary Name of Proposed Programs: Graduate Programs in Biomedical and Molecular Sciences [MSc (Anatomical Sciences), MSc and PhD] Unit(s): Department of Biomedical and Molecular Sciences (DBMS) Proposed Start Date: September 2014 Contact Information (1) Contact Information (2) Name: Louise Winn Name: Anne Tobin Title: Professor Title: DBMS Program Coordinator Associate Head DBMS, Post Graduate Education Unit: DBMS Unit: DBMS E-mail: [email protected] E-mail: [email protected] GRAD New DBMS Program Proposal 19Nov2012.doc Page 1 of 81 Executive Summary (1 page maximum suggested) Briefly summarize the rationale for introducing the new Programs and how they fit with the academic goals of the Faculty/School and University (i.e. -

Shaffer CV 010419.Pdf
CURRICULUM VITAE Name: Thomas H. Shaffer, MS.E., Ph.D. Office Address: Temple University School of Medicine Department of Physiology 3420 North Broad Street Philadelphia, PA 19140 Office Address: Nemours Research Lung Center Department of Biomedical Research Alfred I. duPont Hospital for Children 1600 Rockland Road, A/R 302 Wilmington, DE 19803 Present Academic and Hospital Appointments: 2004 – Present Director, Nemours Center for Pediatric Research Nemours Biomedical Research Alfred I duPont Hospital for Children 1600 Rockland Road Wilmington, DE 19803 2001 - Present Associate Director , Nemours Biomedical Research Nemours Children’s Clinic – Wilmington of The Nemours Foundation Alfred I. duPont Hospital for Children, Wilmington, DE 19803 Director, Nemours Pediatric Lung Center Nemours Children's Clinic - Wilmington of The Nemours Foundation Alfred I. duPont Hospital for Children, Wilmington, DE Director, Office of Technology Transfer Nemours Children's Clinic - Wilmington of The Nemours Foundation Alfred I. duPont Hospital for Children, Wilmington, DE Professor, Pediatrics, Department of Pediatrics Thomas Jefferson University, College of Medicine, Philadelphia, PA 2001-Present Professor Emeritus, Physiology and Pediatrics, Departments of Physiology and Pediatrics Temple University School of Medicine, Philadelphia, PA 1 Training, Awards, Societies, and Membership: Education: 1963-1968 B.S. Mechanical Engineering, Drexel University, Philadelphia, PA 1968 Mathematics, Pennsylvania State University, State College, PA 1969-1970 MSE. Applied -

Engraftment of Bone Marrow from Severe Combined Immunodeficient
Published January 19, 1998 Engraftment of Bone Marrow from Severe Combined Immunodeficient (SCID) Mice Reverses the Reproductive Deficits in Natural Killer Cell–deficient tge26 Mice By Marie-Josée Guimond,* Baoping Wang,‡ and B. Anne Croy* From the *Department of Biomedical Sciences, Ontario Veterinary College, University of Guelph, Guelph, Ontario, Canada N1G 2W1; and the ‡Division of Immunology, Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts 02215 Summary A large, transient population of natural killer (NK) cells appears in the murine uterine mesome- trial triangle during pregnancy. Depletion of uterine (u) NK cells, recently achieved using gene-ablated and transgenic mice, results in pathology. Pregnancies from matings of homozy- gous NK and T cell–deficient tge26 mice have ,1% of normal uNK cell frequency, no devel- opment of an implantation site–associated metrial gland, and an edematous decidua with vascu- lar pathology that includes abnormally high vessel walls/lumens ratios. Fetal loss of 64% occurs midgestation and placentae are small. None of these features are seen in pregnant T cell–defi- Downloaded from cient mice. To confirm the role of the NK cell deficiency in these reproductive deficits, trans- plantation of tge26 females was undertaken using bone marrow from B and T cell–deficient scid/scid donors. Engrafted pregnant females have restoration of the uNK cell population, in- duced metrial gland differentiation, reduced anomalies in the decidua and decidual blood ves- sels, increased placental sizes, and restoration of fetal viability at all gestational days studied (days 10, 12, and 14). Thus, uNK cells appear to have critical functions in pregnancy that promote decidual health, the appropriate vascularization of implantation sites, and placental size. -

Liquid Ventilation
Oman Medical Journal (2011) Vol. 26, No. 1: 4-9 DOI 10. 5001/omj.2011.02 Review Article Liquid Ventilation Qutaiba A. Tawfic, Rajini Kausalya Received: 14 Aug 2010 / Accepted: 23 Nov 2010 © OMSB, 2011 Abstract 1-3,5 Mammals have lungs to breathe air and they have no gills to normal, premature and with lung injury. breath liquids. When the surface tension at the air-liquid Two primary techniques for liquid-assisted ventilation have interface of the lung increases, as in acute lung injury, scientists emerged; total liquid ventilation and partial liquid ventilation.1 started to think about filling the lung with fluid instead of air While total liquid ventilation remains as an experimental to reduce the surface tension and facilitate ventilation. Liquid technique, partial liquid ventilation could be readily applied, but ventilation (LV) is a technique of mechanical ventilation in which its implementation in clinical practice awaits results from ongoing the lungs are insufflated with an oxygenated perfluorochemical and future clinical trials that may define its effectiveness.6 liquid rather than an oxygen-containing gas mixture. The use The PFC liquids used to support pulmonary gas exchange are of perfluorochemicals, rather than nitrogen, as the inert carrier a type of synthetic liquid fluorinated hydrocarbon (hydrocarbons of oxygen and carbon dioxide offers a number of theoretical with the hydrogen replaced by fluorine, and for perflubron where advantages for the treatment of acute lung injury. In addition, a bromine atom is added as well) with high solubility for oxygen there are non-respiratory applications with expanding potential and carbon dioxide.3 These are chemically and biologically inert, including pulmonary drug delivery and radiographic imaging. -

The Journal of Pulmonary Technique
7PMVNF/VNCFS"VHVTU4FQUFNCFS 5IF+PVSOBMPG1VMNPOBSZ5FDIOJRVF may mean the end of VENTILATOR-INDUCED LUNG INJURY. HAMILTON MEDICAL has started and continues to lead the quest for PATIENT SAFETY AND STAFF EFFECTIVENESS. Physicians, Respiratory Care Professionals and Nurses work hard every day to care for the patients that we all serve. Despite their best efforts, patients on ventilators are routinely harmed in the process. Ventilator-Induced Lung Injury is fact. Hamilton Medical wants to change that. We are leading the charge to create a standard of care where Intelligent Ventilation protects the patient from harm, reduces chances for errors and promotes better staff effectiveness. Dear Friends and Colleagues, Those of you who know me will understand the unconventional nature of my actions. Who gives some VP “suit” (a joke, since I rarely wear one) the idea that he should use valuable ad space as a bully pulpit? I do. I could not come up with a catchy, visually exciting marketing piece, so I decided to have a simple conversation with you. I consider the Hamilton Medical team on a quest to increase the safety of mechanical ventilation and increase the efficiency of the healthcare system. Hamilton Medical was the first company to offer closed-loop control mechanical ventilation and we still lead the market today. The last year has been a turning point for Intelligent Ventilation. Hamilton Medical has been working with key experts in the specialty of respiratory care to better understand the mechanisms to provide the SAFETY and EFFECTIVENESS of Intelligent Ventilation to as many leading edge clinicians and facilities as possible. -

A Novel Treatment Method for Bacterial Respiratory Infections
Antibacterial Perfluorocarbon Ventilation: A Novel Treatment Method for Bacterial Respiratory Infections by Ryan A. Orizondo A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Biomedical Engineering) in the University of Michigan 2015 Doctoral Committee: Professor Joseph L. Bull, Co-chair Associate Professor Keith E. Cook, Co-chair, Carnegie Mellon University Professor J. Brian Fowlkes Adjunct Professor John G. Younger © Ryan A. Orizondo 2015 ACKNOWLEDGEMENTS First and foremost, I would like to thank my research advisor, Keith Cook. He has served as an unparalleled mentor to me over the past eight years. He has inspired my career path and had a positive and lasting impact on my life. I would also like to thank my dissertation committee; this work could not have been completed without the valuable insight and guidance that they have contributed. Charlene Babcock and Mario Fabiilli have also contributed valuable work to this project as well as significantly aided in my growth as a researcher. Additionally, many members of my lab have played an important role in carrying out this work. In particular I would like to thank Erin Ebsch, Chi Chi Do-Nguyen, Marissa Morales, Diane Nelson, Josh Pohlmann, and Erin Rocci. Lastly, and perhaps most importantly, I would like to recognize those who have supported me in this endeavor outside of the laboratory. My parents have always provided me with loving support and countless opportunities, ultimately enabling me to pursue my passions. My sister, Carissa Orizondo, and girlfriend, Catalina Moreno, have been a never-ending source of support, counsel, and assurance during the entirety of this work. -

Guelph Conundrum
ISSN 0229-2378 gue p h UNIVERSITY NEWS BULLETIN Volume 29 Number 28 August 1, 1985 The limited awareness of Guelph programs The extends beyond the academic into extra-curricular actitivities as well. Well over 80 per cent of all survey respondents had never heard of such campus events as Guelph College Royal, March Counselling, Guelph Interaction or Summer Orientation. The study also examined the impact of the conundrum Heather Cooper poster and the image it portrays. Recognition of the poster was high among students Although everyone surveyed had heard of and teachers, with most reporting they had seen it in Guelph, knowledge of the programs it offers varied a high school classroom, hallway or guidance office. greatly. Teachers were more aware of the broad Only a few of the parents remembered having seen range of programs available than students and parents the poster before. Although some respondents who — a finding that is understandable, says Wardlaw, had seen it did not remember the sponsoring univer- because much of Guelph's liaison material is directed sity, most made the association. through teachers. Almost everyone agreed that the poster is beauti- Guelph was best known among respondents for ful and memorable. Many teachers said the print is se its agriculture and veterinary medicine programs, but popular, in fact, that it is frequently stolen by stu- there was also strong recognition of its biological dents off school hallway walls. sciences. When asked which of 14 Ontario univer- When asked whether they think Guelph should sities was academically superior in the biological continue to use the poster or find something new, sciences, the largest percentage of the respondents 72 per cent of the students favored continued use of (30 per cent) said Guelph. -
Schofield Memorial Lecture
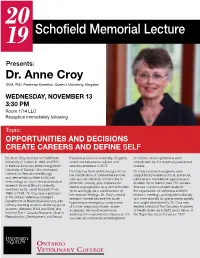
20 19 Schofield Memorial Lecture Presents: Dr. Anne Croy DVM, PhD. Professor Emeritus, Queen’s University, Kingston WEDNESDAY, NOVEMBER 13 3:30 PM Room 1714 LLC Reception immediately following Topic: OPPORTUNITIES AND DECISIONS CREATE CAREERS AND DEFINE SELF Dr. Anne Croy received her DVM from Function at Queen’s University, Kingston of children whose gestations were University of Guelph in 1969 and PhD where she became an adjunct and complicated by this maternally-presented in Medical Sciences (Immunology) from emeritus professor in 2017. disease. University of Toronto. She developed Dr. Croy has been widely recognized for Dr. Croy’s research programs were interests in Reproductive Biology her identification of uterine Natural Killer supported by numerous local, provincial, and uterine Natural Killer (uNK) cell cells and her definition of their roles in national and international agencies and immunology as a part-time postdoctoral promotion of early, post-implantation enabled her to mentor over 120 trainees. research fellow at Brock University, uterine angiogenesis using animal models She has chaired and participated in mentored by Dr. Janet Rossant. From (mice and pigs). As a consequence of the organization of numerous scientific 1985 to 2004, Dr. Croy was a professor her research findings, Dr. Croy’s central research meetings, participated nationally in the Ontario Veterinary College’s research interest became the acute, and internationally on grants review panels Department of Biomedical Sciences with hypertensive emergency complication and taught internationally. Dr. Croy was primary teaching duties in veterinary gross of human pregnancy known as pre- elected a fellow of the Canadian Academy anatomy. Between 2004 and 2016, she eclampsia. -
Robert Jan Houmes Jan Robert Pediatric Extracorporeal Membrane Oxygenation
Pediatric Extracorporeal Membrane Oxygenation, Pediatric Robert Jan Houmes Pediatric Why, When and How When Why, Extracorporeal Membrane Oxygenation, Why, Robert Jan Houmes Robert Jan When and How Pediatric Extracorporeal Membrane Oxygenation, Why, When and How Robert Jan Marcel Houmes ISBN/EAN: 978-90-825197-0-9 © R.J.M. Houmes, 2016 No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by means, electronically, mechanically, by photocopying, recording, or otherwise, without the prior written permission of the author. Layout and printing by: Optima Grafische Communicatie, Rotterdam, the Netherlands Pediatric Extracorporeal Membrane Oxygenation, Why, When and How Kunstlong behandeling bij kinderen, waarom, wanneer en hoe Proefschrift ter verkrijging van de graad van doctor aan de Erasmus Universiteit Rotterdam op gezag van de rector magnificus Prof.dr. H.A.P. Pols en volgens besluit van het College voor Promoties. De openbare verdediging zal plaatsvinden op woensdag 25 mei 2016 om 15.30 uur door Robert Jan Marcel Houmes geboren te Middelburg PromotiEcommissiE Promotor: Prof.dr. D. Tibboel Overige leden: Prof.dr. K. Allegaert Prof.dr. D.A.M.P.J. Gommers Prof.dr. I.K.M. Reiss copromotor: Dr. E.D. Wildschut ContEnts chapter 1 Introduction and outline of this thesis 7 chapter 2 Invasive ventilation modes in children: a systematic review 19 and meta-analysis chapter 3 How to achieve adherence to a ventilation algorithm for 37 critically ill children? chapter 4 Challenges in non-neonatal