Dequalinium Chloride for the Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antiseptics and Disinfectants for the Treatment Of
Verstraelen et al. BMC Infectious Diseases 2012, 12:148 http://www.biomedcentral.com/1471-2334/12/148 RESEARCH ARTICLE Open Access Antiseptics and disinfectants for the treatment of bacterial vaginosis: A systematic review Hans Verstraelen1*, Rita Verhelst2, Kristien Roelens1 and Marleen Temmerman1,2 Abstract Background: The study objective was to assess the available data on efficacy and tolerability of antiseptics and disinfectants in treating bacterial vaginosis (BV). Methods: A systematic search was conducted by consulting PubMed (1966-2010), CINAHL (1982-2010), IPA (1970- 2010), and the Cochrane CENTRAL databases. Clinical trials were searched for by the generic names of all antiseptics and disinfectants listed in the Anatomical Therapeutic Chemical (ATC) Classification System under the code D08A. Clinical trials were considered eligible if the efficacy of antiseptics and disinfectants in the treatment of BV was assessed in comparison to placebo or standard antibiotic treatment with metronidazole or clindamycin and if diagnosis of BV relied on standard criteria such as Amsel’s and Nugent’s criteria. Results: A total of 262 articles were found, of which 15 reports on clinical trials were assessed. Of these, four randomised controlled trials (RCTs) were withheld from analysis. Reasons for exclusion were primarily the lack of standard criteria to diagnose BV or to assess cure, and control treatment not involving placebo or standard antibiotic treatment. Risk of bias for the included studies was assessed with the Cochrane Collaboration’s tool for assessing risk of bias. Three studies showed non-inferiority of chlorhexidine and polyhexamethylene biguanide compared to metronidazole or clindamycin. One RCT found that a single vaginal douche with hydrogen peroxide was slightly, though significantly less effective than a single oral dose of metronidazole. -

1 Brief Report: the Virucidal Efficacy of Oral Rinse Components Against SARS-Cov-2 in Vitro Evelina Statkute1†, Anzelika Rubin
bioRxiv preprint doi: https://doi.org/10.1101/2020.11.13.381079; this version posted November 13, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. Brief Report: The Virucidal Efficacy of Oral Rinse Components Against SARS-CoV-2 In Vitro Evelina Statkute1†, Anzelika Rubina1†, Valerie B O’Donnell1, David W. Thomas2† Richard J. Stanton1† 1Systems Immunity University Research Institute, Division of Infection & Immunity, School of Medicine, Heath Park, Cardiff, CF14 4XN 2Advanced Therapies Group, School of Dentistry, Cardiff University, Heath Park, Cardiff CF14 4XY, UK †These authors contributed equally * Correspondence: [email protected], [email protected] Running title: Virucidal Activity of Mouthwashes Keywords: SARS-CoV2, mouthwash, lipid, envelope Disclosure: Venture Life Group plc provided information on mouthwash formulations employed in the study, but had no role in funding, planning, execution, analysis or writing of this study. A separate study funded to Cardiff University by Venture Life Group is assessing in vivo efficacy of CPC in patients with COVID19. The investigators declare no direct conflicts exist. 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.11.13.381079; this version posted November 13, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. -

Tonsillopharyngitis - Acute (1 of 10)
Tonsillopharyngitis - Acute (1 of 10) 1 Patient presents w/ sore throat 2 EVALUATION Yes EXPERT Are there signs of REFERRAL complication? No 3 4 EVALUATION Is Group A Beta-hemolytic Yes DIAGNOSIS Streptococcus (GABHS) • Rapid antigen detection test infection suspected? (RADT) • roat culture No TREATMENT EVALUATION No A Supportive management Is GABHS confi rmed? B Pharmacological therapy (Non-GABHS) Yes 5 TREATMENT A EVALUATE RESPONSEMIMS Supportive management TO THERAPY C Pharmacological therapy • Antibiotics Poor/No Good D Surgery, if recurrent or complicated response response REASSESS PATIENT COMPLETE THERAPY & REVIEW THE DIAGNOSIS© Not all products are available or approved for above use in all countries. Specifi c prescribing information may be found in the latest MIMS. B269 © MIMS Pediatrics 2020 Tonsillopharyngitis - Acute (2 of 10) 1 ACUTE TONSILLOPHARYNGITIS • Infl ammation of the tonsils & pharynx • Etiologies include bacterial (group A β-hemolytic streptococcus, Haemophilus infl uenzae, Fusobacterium sp, etc) & viral (infl uenza, adenovirus, coronavirus, rhinovirus, etc) pathogens • Sore throat is the most common presenting symptom in older children TONSILLOPHARYNGITIS 2 EVALUATION FOR COMPLICATIONS • Patients w/ sore throat may have deep neck infections including epiglottitis, peritonsillar or retropharyngeal abscess • Examine for signs of upper airway obstruction Signs & Symptoms of Sore roat w/ Complications • Trismus • Inability to swallow liquids • Increased salivation or drooling • Peritonsillar edema • Deviation of uvula -

NINDS Custom Collection II
ACACETIN ACEBUTOLOL HYDROCHLORIDE ACECLIDINE HYDROCHLORIDE ACEMETACIN ACETAMINOPHEN ACETAMINOSALOL ACETANILIDE ACETARSOL ACETAZOLAMIDE ACETOHYDROXAMIC ACID ACETRIAZOIC ACID ACETYL TYROSINE ETHYL ESTER ACETYLCARNITINE ACETYLCHOLINE ACETYLCYSTEINE ACETYLGLUCOSAMINE ACETYLGLUTAMIC ACID ACETYL-L-LEUCINE ACETYLPHENYLALANINE ACETYLSEROTONIN ACETYLTRYPTOPHAN ACEXAMIC ACID ACIVICIN ACLACINOMYCIN A1 ACONITINE ACRIFLAVINIUM HYDROCHLORIDE ACRISORCIN ACTINONIN ACYCLOVIR ADENOSINE PHOSPHATE ADENOSINE ADRENALINE BITARTRATE AESCULIN AJMALINE AKLAVINE HYDROCHLORIDE ALANYL-dl-LEUCINE ALANYL-dl-PHENYLALANINE ALAPROCLATE ALBENDAZOLE ALBUTEROL ALEXIDINE HYDROCHLORIDE ALLANTOIN ALLOPURINOL ALMOTRIPTAN ALOIN ALPRENOLOL ALTRETAMINE ALVERINE CITRATE AMANTADINE HYDROCHLORIDE AMBROXOL HYDROCHLORIDE AMCINONIDE AMIKACIN SULFATE AMILORIDE HYDROCHLORIDE 3-AMINOBENZAMIDE gamma-AMINOBUTYRIC ACID AMINOCAPROIC ACID N- (2-AMINOETHYL)-4-CHLOROBENZAMIDE (RO-16-6491) AMINOGLUTETHIMIDE AMINOHIPPURIC ACID AMINOHYDROXYBUTYRIC ACID AMINOLEVULINIC ACID HYDROCHLORIDE AMINOPHENAZONE 3-AMINOPROPANESULPHONIC ACID AMINOPYRIDINE 9-AMINO-1,2,3,4-TETRAHYDROACRIDINE HYDROCHLORIDE AMINOTHIAZOLE AMIODARONE HYDROCHLORIDE AMIPRILOSE AMITRIPTYLINE HYDROCHLORIDE AMLODIPINE BESYLATE AMODIAQUINE DIHYDROCHLORIDE AMOXEPINE AMOXICILLIN AMPICILLIN SODIUM AMPROLIUM AMRINONE AMYGDALIN ANABASAMINE HYDROCHLORIDE ANABASINE HYDROCHLORIDE ANCITABINE HYDROCHLORIDE ANDROSTERONE SODIUM SULFATE ANIRACETAM ANISINDIONE ANISODAMINE ANISOMYCIN ANTAZOLINE PHOSPHATE ANTHRALIN ANTIMYCIN A (A1 shown) ANTIPYRINE APHYLLIC -

Inactivation of SARS-Cov-2 Through Treatment with the Mouth Rinsing Solutions Viruprox® and Bacterx® Pro
microorganisms Communication Inactivation of SARS-CoV-2 through Treatment with the Mouth Rinsing Solutions ViruProX® and BacterX® Pro Julia Koch-Heier 1,†, Helen Hoffmann 1,†, Michael Schindler 2 , Adrian Lussi 3,4 and Oliver Planz 1,* 1 Interfaculty Institute for Cell Biology, Department of Immunology, Eberhard Karls University of Tuebingen, 72076 Tuebingen, Germany; [email protected] (J.K.-H.); [email protected] (H.H.) 2 Institute for Medical Virology and Epidemiology of Viral Disease, Department of Molecular Virology, 72076 Tuebingen, Germany; [email protected] 3 Department of Operative Dentistry and Periodontology, University Medical Centre, 79106 Freiburg, Germany; [email protected] 4 School of Dental Medicine, University of Bern, 3010 Bern, Switzerland * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic effects daily dental work. Therefore, infection control measures are necessary to prevent infection of dental personnel during dental treatments. The use of a preprocedural mouth rinse with chlorhexidine (CHX), cetylpyridinium chloride (CPC), or hydrogen peroxide (H2O2) solution for 30–60 s may reduce the viral load and may protect the personnel in a dental practice. In the present study the ® virucidal effect of the mouth rinsing solutions ViruProX with 0.05% CPC and 1.5% H2O2 and Citation: Koch-Heier, J.; Hoffmann, BacterX® pro containing 0.1% CHX, 0.05% CPC, and 0.005% sodium fluoride (F-) was investigated H.; Schindler, M.; Lussi, A.; Planz, O. in vitro. The mouth rinsing solutions successfully inactivated infectious SARS-CoV-2 particles, the Inactivation of SARS-CoV-2 through causative agent of coronavirus disease 2019 (COVID-19), within 30 s. -

Chemical Modulators of Fibrinogen Production and Their Impact on Venous Thrombosis
Published online: 2020-12-10 Coagulation and Fibrinolysis 433 Chemical Modulators of Fibrinogen Production and Their Impact on Venous Thrombosis Rui Vilar1 Samuel W. Lukowski1,2 Marco Garieri1 Corinne Di Sanza1 Marguerite Neerman-Arbez1,3 Richard J. Fish1 1 Department of Genetic Medicine and Development, University of Address for correspondence Richard J. Fish, Department of Genetic Geneva Faculty of Medicine, Geneva, Switzerland Medicine and Development, Faculty of Medicine, University of 2 Institute for Molecular Bioscience, The University of Queensland, Geneva, 1, rue Michel-Servet, Geneva 1206, Switzerland Saint Lucia, Queensland, Australia (e-mail: [email protected]). 3 iGE3, Institute of Genetics and Genomics in Geneva, Geneva, Switzerland Thromb Haemost 2021;121:433–448. Abstract Thrombosis is a leading cause of morbidity and mortality. Fibrinogen, the soluble substrate for fibrin-based clotting, has a central role in haemostasis and thrombosis and its plasma concentration correlates with cardiovascular disease event risk and a prothrombotic state in experimental models. We aimed to identify chemical entities capable of changing fibrinogen production and test their impact on experimental thrombosis. A total of 1,280 bioactive compounds were screened for their ability to alter fibrinogen production by hepatocyte-derived cancer cells and a selected panel was tested in zebrafish larvae. Anthralin and all-trans retinoic acid (RA) were identified as fibrinogen-lowering and fibrinogen-increasing moieties, respectively. In zebrafish larvae, anthralin prolonged laser-induced venous occlusion times and reduced thrombocyte accumulation at injury sites. RA had opposite effects. Treatment with RA, a nuclear receptor ligand, increased fibrinogen mRNA levels. Using an antisense morpholino oligonucleotide to deplete zebra- fish fibrinogen, we correlated a shortening of laser-induced venous thrombosis times with RA treatment and fibrinogen protein levels. -

Pharmaceutical Appendix to the Tariff Schedule 2
Harmonized Tariff Schedule of the United States (2006) – Supplement 1 (Rev. 1) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2006) – Supplement 1 (Rev. 1) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABACAVIR 136470-78-5 ACEXAMIC ACID 57-08-9 ABAFUNGIN 129639-79-8 ACICLOVIR 59277-89-3 ABAMECTIN 65195-55-3 ACIFRAN 72420-38-3 ABANOQUIL 90402-40-7 ACIPIMOX 51037-30-0 ABARELIX 183552-38-7 ACITAZANOLAST 114607-46-4 ABCIXIMAB 143653-53-6 ACITEMATE 101197-99-3 ABECARNIL 111841-85-1 ACITRETIN 55079-83-9 ABIRATERONE 154229-19-3 ACIVICIN 42228-92-2 ABITESARTAN 137882-98-5 ACLANTATE 39633-62-0 ABLUKAST 96566-25-5 ACLARUBICIN 57576-44-0 ABUNIDAZOLE 91017-58-2 ACLATONIUM NAPADISILATE 55077-30-0 ACADESINE 2627-69-2 ACODAZOLE 79152-85-5 ACAMPROSATE 77337-76-9 ACONIAZIDE 13410-86-1 ACAPRAZINE 55485-20-6 ACOXATRINE 748-44-7 ACARBOSE 56180-94-0 ACREOZAST 123548-56-1 ACEBROCHOL 514-50-1 ACRIDOREX 47487-22-9 ACEBURIC -

Unduh File PDF
Majalah Farmasetika, 3 (5) 2018, 98-101 https://doi.org/10.24198/farmasetika.v3i5.21633 e-ISSN : 2686-2506 Perkembangan Obat Sariawan dan Terapi Alternatifnya Prilly Mutiara Sandy*, Fira Burhanisa Irawan Program Studi Sarjana Farmasi, Fakultas Farmasi, Universitas Padjadjaran, Sumedang 45363 email: [email protected] Abstrak : Sariawan merupakan penyakit mulut yang sudah tidak asing lagi. Berbagai kalangan mulai dari balita, remaja, orang tua, maupun lanjut usia tentu pernah mengalami penyakit tersebut. Efek dari sariawan itu sendiri ialah bisa menyebabkan para penderitanya tidak nafsu makan dan mulut terasa perih. Pengobatan yang dapat dilakukan adalah dengan mengonsumsi zat pemati rasa dan antiseptika.Pemakaiannya obat bisa dilakukan sebanyak 2-3 kali dalam sehari. Selain dengan zat pemati rasa, sariawan juga dapat diobati dengan antiseptika. Hasil terbaik dari penggunaan antiseptika terbukti oleh obat kumur provid-ion (Betadine) dan klorheksidin dalam bentuk tablet hisap srta larutan peroksida 3%. Selain itu juga bisa menggunakan obat kumur yang mengandung Chlorhexidine gluconate 2%, sodium hyaluronate, PVP , dan glycyrrhetinic. BPOM menganjurkan penggunaan obat-obat yang memiliki kandungan enzydamine HCL, providone iodine 1%, atau kombinasi dequalinium chloride dan vitamin C. Bagi yang ingin menyembuhkan sariawan dengan bahan-bahan alami, yaitu: tanaman gambir, daun sirih, air garam, dan cabai. Keyword : obat, sariawan, terapi alternative Outline • Pendahuluan • Terapi sariawan • Albothyl (policresulen) • Terapi alternatif • Kesimpulan Pendahuluan Sariawan atau aphtous stomatitis adalah luka yang terdapat di dalam mulut yang biasanya berbentuk oval atau bulat berwarna putih dan dapat menimbulkan rasa tidak sakit serta tidak nyaman. Sariawan disebabkan oleh beberapa hal, diantaranya ialah kurangnya vit C, vit B12 dan bisa juga karena adanya infeksi yang disebabkan oleh bakteri, virus, atau jamur. -
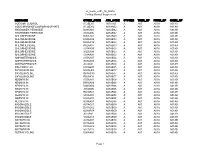
Vr Meds Ex01 3B 0825S Coding Manual Supplement Page 1
vr_meds_ex01_3b_0825s Coding Manual Supplement MEDNAME OTHER_CODE ATC_CODE SYSTEM THER_GP PHRM_GP CHEM_GP SODIUM FLUORIDE A12CD01 A01AA01 A A01 A01A A01AA SODIUM MONOFLUOROPHOSPHATE A12CD02 A01AA02 A A01 A01A A01AA HYDROGEN PEROXIDE D08AX01 A01AB02 A A01 A01A A01AB HYDROGEN PEROXIDE S02AA06 A01AB02 A A01 A01A A01AB CHLORHEXIDINE B05CA02 A01AB03 A A01 A01A A01AB CHLORHEXIDINE D08AC02 A01AB03 A A01 A01A A01AB CHLORHEXIDINE D09AA12 A01AB03 A A01 A01A A01AB CHLORHEXIDINE R02AA05 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S01AX09 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S02AA09 A01AB03 A A01 A01A A01AB CHLORHEXIDINE S03AA04 A01AB03 A A01 A01A A01AB AMPHOTERICIN B A07AA07 A01AB04 A A01 A01A A01AB AMPHOTERICIN B G01AA03 A01AB04 A A01 A01A A01AB AMPHOTERICIN B J02AA01 A01AB04 A A01 A01A A01AB POLYNOXYLIN D01AE05 A01AB05 A A01 A01A A01AB OXYQUINOLINE D08AH03 A01AB07 A A01 A01A A01AB OXYQUINOLINE G01AC30 A01AB07 A A01 A01A A01AB OXYQUINOLINE R02AA14 A01AB07 A A01 A01A A01AB NEOMYCIN A07AA01 A01AB08 A A01 A01A A01AB NEOMYCIN B05CA09 A01AB08 A A01 A01A A01AB NEOMYCIN D06AX04 A01AB08 A A01 A01A A01AB NEOMYCIN J01GB05 A01AB08 A A01 A01A A01AB NEOMYCIN R02AB01 A01AB08 A A01 A01A A01AB NEOMYCIN S01AA03 A01AB08 A A01 A01A A01AB NEOMYCIN S02AA07 A01AB08 A A01 A01A A01AB NEOMYCIN S03AA01 A01AB08 A A01 A01A A01AB MICONAZOLE A07AC01 A01AB09 A A01 A01A A01AB MICONAZOLE D01AC02 A01AB09 A A01 A01A A01AB MICONAZOLE G01AF04 A01AB09 A A01 A01A A01AB MICONAZOLE J02AB01 A01AB09 A A01 A01A A01AB MICONAZOLE S02AA13 A01AB09 A A01 A01A A01AB NATAMYCIN A07AA03 A01AB10 A A01 -

Efficacy of Commercial Mouth-Rinses on SARS-Cov-2 Viral Load in Saliva: Randomized Control Trial in Singapore
medRxiv preprint doi: https://doi.org/10.1101/2020.09.14.20186494; this version posted September 18, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Efficacy of commercial mouth-rinses on SARS-CoV-2 viral load in saliva: Randomized Control Trial in Singapore Chaminda J. Seneviratne1,2*+, Preethi Balan1,2+, Karrie Ko Kwan Ki3+, Nadeeka S Udawatte1, Deborah Lai3, Dorothy Ng Hui Lin4 , Indumathi Venkatachalam4, Jay Lim Kheng Sit5, Ling Moi Lin6, Lynette Oon3, Goh Bee Tin1,2, Jean Sim Xiang Ying4*+ 1Singapore Oral Microbiomics Initiative, National Dental Research Institute Singapore (NDRIS), National Dental Centre Singapore, 2Oral Health ACP, Duke NUS Medical School, Singapore; 3Department of Microbiology, 4Department of Infectious Diseases, 5Department of Urology, 6Department of Infection Prevention and Epidemiology, Singapore General Hospital, Singapore +Equal contribution *Corresponding authors Associate Prof. Chaminda Jaya Seneviratne, Lead Principal Investigator, Singapore Oral Microbiomics Initiative, National Dental Research Institute Singapore (NDRIS), National Dental Centre Singapore, SingHealth Oral Health ACP, Duke NUS Medical School, Singapore, [email protected] Dr. Jean Sim Xiang Ying, Consultant, Department of Infectious Diseases, Singapore General Hospital, SingHealth, Singapore [email protected] Keywords: COVID-19, SARS-CoV-2, mouth-rinses, saliva, clinical trial NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. 1 medRxiv preprint doi: https://doi.org/10.1101/2020.09.14.20186494; this version posted September 18, 2020. -

An Update on the Role of Atopobium Vaginae in Bacterial Vaginosis: What to Consider When Choosing a Treatment? a Mini Review
Archives of Gynecology and Obstetrics (2019) 300:1–6 https://doi.org/10.1007/s00404-019-05142-8 REVIEW An update on the role of Atopobium vaginae in bacterial vaginosis: what to consider when choosing a treatment? A mini review Werner Mendling1 · Ana Palmeira‑de‑Oliveira2,3 · Stephan Biber4 · Valdas Prasauskas4 Received: 23 January 2019 / Accepted: 26 March 2019 / Published online: 5 April 2019 © The Author(s) 2019 Abstract Introduction Bacterial vaginosis (BV) is the most common vaginal disorder in reproductive-age women. The condition is characterised by the replacement of a healthy, lactobacilli-dominated vaginal microbiota by anaerobic and facultative anaerobic bacteria. BV increases the risk of acquisition of STIs and is associated with pregnancy complications. Although the composition of the bacteria in BV varies between individuals, there are some species such as Gardnerella, Atopobium, Mycoplasma, Snethia, Megasphera, Dialister, etc., that are found most frequently. Material and Methods Literature research to the importance of Atopobium vaginae in BV and treatment options. Results Atopobium (A.) vaginae is an important component of the complex abnormal vaginal fora in BV; even though A. vaginae, like Gardnerella vaginalis, has also been detected in the normal fora, it is much more common in BV patients. A. vaginae has been shown to play an important role in the pathophysiology of BV and is thought to be at least a partial cause of the known negative sequelae. The presence of A. vaginae in the BV-associated bioflms and its resistance to some antimicrobial substances has been described - this seems to have a major impact on treatment outcome. -
Open Operatory Dental Setting Infection Control Practices and Risk Of
RAPID REVIEW 11/26/2020 Open operatory dental setting infection control practices and risk of transmission during aerosol-generating dental procedures Key Findings • Few pre-operative mouth rinses have in vivo data available on their virucidal effectiveness versus SARS-CoV-2; and hydrogen peroxide should no longer be recommended as a pre-operative mouth rinse due to lack of efficacy versus SARS-CoV-2. • No direct evidence has been published on the use of dental dams and various types of suction to prevent SARS-CoV-2 aerosol spread. Pathogen non-specific contamination studies indicate an important role for dental dams and suction in reducing aerosol spread during aerosol-generating dental procedures. • No direct evidence has been published on aerosol transmission of SARS-CoV-2 in open versus closed dental operatories. The limited evidence available indicates that spread can be diffuse affecting adjacent bays in an open operatory set-up. Spread may be impacted by factors such as air flow conditions and work practice controls, but this requires further investigation. Background and Scope The Provincial Infectious Diseases Advisory Committee – Infection Prevention and Control (PIDAC-IPC) has recommended that all aerosol-generating dental procedures (AGDPs) be performed in individual rooms due to risk of SARS-CoV-2 transmission from aerosolized saliva.1 Open dental operatories may encounter challenges or an inability to improve ventilation or construct enclosed operatories in accordance with this recommendation. Globally, many dental guidance documents exist and yet many do not cite evidence to support the guidance provided.2 This review aims to summarize available evidence for work practice controls to reduce infectious aerosol production during dental procedures with no restriction on type of dental procedure, but with specific reference to reduction of SARS-CoV-2 transmission risk.