Enhancement Strategies for Transdermal Drug Delivery Systems Current Trends and Applications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Long-Acting Cabotegravir: the Future of HIV Prep
Long-Acting Injectable Cabotegravir: the Future of HIV PrEP? Brian R. Wood, MD Associate Professor of Medicine University of Washington Mountain West AIDS Education & Training Center June 4, 2020 Disclosures No conflicts of interest or relationships to disclose. Will be discussing an investigational antiretroviral. Full HPTN 083 study results not yet available. Will be reviewing data from a preliminary DSMB analysis today. See press release and webinar: https://www.hptn.org/news-and-events/announcements/cab- la-proves-be-highly-effective-prevention-hiv-acquisition Outline • General notes about cabotegravir • News from the phase 3 PrEP trial (and why it’s a big deal) • Questions, concerns, and next steps for long-acting PrEP What is Cabotegravir? Cabotegravir (CAB) • Investigational integrase strand transfer inhibitor • Potential infrequent dosing and parenteral administration - Oral half-life: 40 hours - Parenteral nanosuspension (IM, SC) half-life: 21-50 days - Median time from discontinuation to undetectable plasma level (IM, SC): 43-66 weeks • Metabolized by UGT1A1 (main pathway) & UGT1A9 - Minimal CYP metabolism; likely few drug interactions • Relatively low barrier to resistance Aidsinfo.nih.gov/drugs Injectable Long-Acting Cabotegravir Image courtesy of Dr. Raphael Landovitz, UCLA What is the HPTN 083 Trial and What’s the Big News? HPTN 083 A Phase 2b/3 Double Blind Safety and Efficacy Study of Injectable Cabotegravir Compared to Daily Oral TDF/FTC, for Pre-Exposure Prophylaxis in HIV-Uninfected Cisgender Men and TranHPTNsgender Women wh o 083have Sex wi thSites Men – Phase 2b/3 Target enrollment: 4,500 HIV- uninfected cisgender men and transgender 45 Sites in 8 Countrieswomen who have sex with men and who are at risk of HIV acquisition Primary outcome: HIV Prevention effectiveness of cabotegravir compared to daily oral TDF/FTC United States India Vietnam Thailand Peru Brazil South Argentina Africa ClinicalTrials.gov Identifier: NCT02720094 Slide courtesy of Dr. -

LATTE Study Oral Cabotegravir + Rilpivirine Versus Efavirenz + 2 NRTI’S LATTE Study: Design
Oral Cabotegravir + Rilpivirine versus Efavirenz + 2 NRTI’s LATTE Study Oral Cabotegravir + Rilpivirine versus Efavirenz + 2 NRTI’s LATTE Study: Design Study Design: CAB 10 mg CAB 10 mg + 2 NRTI’s + RPV 25 mg • BacKground: Phase 2b, (n = 60) (n = 52) randoMized, partially blinded study done at Multiple centers CAB 30 mg CAB 30 mg in the U.S. and Canada + 2 NRTI’s + RPV 25 mg (n = 60) (n = 51) • Inclusion Criteria (n = 244) - Age ≥18 years - Antiretroviral-naïve CAB 60 mg CAB 60 mg - HIV RNA >1,000 copies/ML + 2 NRTI’s + RPV 25 mg - CD4 count >200 cells/MM3 (n = 61) (n = 53) - CrCl >50 ML/Min - No hepatitis B Efavirenz 600 mg Efavirenz 600 mg - No significant transaMinitis + 2 NRTI’s + 2 NRTI’s (n = 62) (n = 46) 24-week lead-in phase Source: Margolis DA, et al. Lancet Infect Dis. 2015;15:1145-55. Oral Cabotegravir + Rilpivirine versus Efavirenz + 2 NRTI’s LATTE Study: Results Cabotegravir + 2NRTIs Cabotegravir + Rilpivirine Efavirenz + 2NRTIs Induction* Maintenance* 100 80 86 82 76 74 71 60 63 40 HIV RNA <50 copies/mL (%) <50 copies/mL HIV RNA 20 156/181 46/62 149/181 44/62 137/181 39/62 0 Week 24 Week 48 Week 96 *Cabotegravir data is composite of all cabotegravir doses Source: Margolis DA, et al. Lancet Infect Dis. 2015;15:1145-55. Oral Cabotegravir + Rilpivirine versus Efavirenz + 2 NRTI’s LATTE Study: Results 100 Induction* Maintenance 80 60 Cabotegravir 10 mg + Rilpivirine 40 Cabotegravir 30 mg + Rilpivirine HIV RNA <40 copies/mL HIV RNA 20 Cabotegravir 60 mg + Rilpivirine Efavirenz 600 mg + 2NRTIs 0 0 12 24 36 48 60 72 84 96 Treatment Week *During induction phase cabotegravir administered with investigator chosen 2NRTIs Source: Margolis DA, et al. -

(KPIC) PPO and Out-Of- Area Indemnity (OOA) Drug Formulary with Specialty Drug Tier
Kaiser Permanente Insurance Company (KPIC) PPO and Out-of- Area Indemnity (OOA) Drug Formulary with Specialty Drug Tier This Drug Formulary was updated: September 1, 2021 NOTE: This drug formulary is updated often and is subject to change. Upon revision, all previous versions of the drug formulary are no longer in effect. This document contains information regarding the drugs that are covered when you participate in the California Nongrandfathered PPO and Out-of- Area Indemnity (OOA) Health Insurance Plans with specialty drug tier offered by Kaiser Permanente Insurance Company (KPIC) and fill your prescription at a MedImpact network pharmacy. Access to the most current version of the Formulary can be obtained by visiting kp.org/kpic-ca-rx-ppo-ngf. For help understanding your KPIC insurance plan benefits, including cost sharing for drugs under the prescription drug benefit and under the medical benefit, please call 1-800-788-0710 or 711 (TTY) Monday through Friday, 7a.m. to 7p.m. For help with this Formulary, including the processes for submitting an exception request and requesting prior authorization and step therapy exceptions, please call MedImpact 24 hours a day, 7 days a week, at 1-800-788-2949 or 711 (TTY). For cost sharing information for the outpatient prescription drug benefits in your specific plan, please visit: kp.org/kpic-ca-rx-ppo-ngf. For help in your preferred language, please see the Kaiser Permanente Insurance Company Notice of Language Assistance in this document. KPIC PPO NGF Table of Contents Informational Section................................................................................................................................2 -

Antivirals: HIV –Cabotegravir/Rilpivirine (Cabenuva) Medical Policy No
Antivirals: HIV –Cabotegravir/rilpivirine (Cabenuva) Medical policy no. 12.10.99.AB-1 Effective Date: June 1, 2021 Related medical policies: • 12.10.99 Antivirals- HIV Combinations • 12.10.99.AA Antivirals – HIV: emtricitabine-tenofovir (Descovy) Note: New-to-market drugs included in this class based on the Apple Health Preferred Drug List (AHPDL) are non-preferred and subject to this prior authorization (PA) criteria. Non-preferred agents in this class require an inadequate response or documented intolerance due to severe adverse reaction or contraindication to at least ONE preferred regimen. If a drug within this policy receives a new indication approved by the Food and Drug Administration (FDA), medical necessity for the new indication will be determined on a case-by-case basis following FDA labeling. To see the list of the current AHPDL, please visit: https://www.hca.wa.gov/assets/billers-and-providers/apple-health-preferred-drug-list.xlsx Before authorization of Cabenuva will be approved, documentation from TheraCom specialty pharmacy showing the patient has been established on Vocabria must be included. Documentation must include patient’s name, patient’s date of birth, NDC, quantity/days supply, and date patient received the medication. TheraCom Pharmacy contact information: TheraCom Mailing Address: TheraCom VIIV Specific Team numbers (Used to locate TheraCom in e-Prescribing systems) Phone: 1-844-276-6299 TheraCom Fax: 1-833-904-1881 345 International Blvd Ste 200 Brooks, KY 40109 Background: Human immunodeficiency virus (HIV) is a single-stranded RNA retrovirus that attacks the immune system, specifically CD4+ T-helper cells, causing a progressive decrease in CD4+ T cell count and increased susceptibility of a person to infections. -

Pdf/Dires/Hiv-Surveillance- 1: 185–95
Articles Emtricitabine and tenofovir alafenamide vs emtricitabine and tenofovir disoproxil fumarate for HIV pre-exposure prophylaxis (DISCOVER): primary results from a randomised, double-blind, multicentre, active-controlled, phase 3, non-inferiority trial Kenneth H Mayer, Jean-Michel Molina, Melanie A Thompson, Peter L Anderson, Karam C Mounzer, Joss J De Wet, Edwin DeJesus, Heiko Jessen, Robert M Grant, Peter J Ruane, Pamela Wong, Ramin Ebrahimi, Lijie Zhong, Anita Mathias, Christian Callebaut, Sean E Collins, Moupali Das, Scott McCallister, Diana M Brainard, Cynthia Brinson, Amanda Clarke, Pep Coll, Frank A Post, C Bradley Hare Summary Background Tenofovir alafenamide shows high antiviral efficacy and improved renal and bone safety compared with Lancet 2020; 396: 239–54 tenofovir disoproxil fumarate when used for HIV treatment. Here, we report primary results from a blinded phase 3 See Comment page 214 study evaluating the efficacy and safety of pre-exposure prophylaxis (PrEP) with emtricitabine and tenofovir The Fenway Institute, Fenway alafenamide versus emtricitabine and tenofovir disoproxil fumarate for HIV prevention. Health, Boston, MA, USA (Prof K H Mayer MD); Department of Medicine, Methods This study is an ongoing, randomised, double-blind, multicentre, active-controlled, phase 3, non- Harvard Medical School, inferiority trial done at 94 community, public health, and hospital-associated clinics located in regions of Europe Boston, MA, USA and North America, where there is a high incidence of HIV or prevalence of people living with HIV, or both. We (Prof K H Mayer); Infectious enrolled adult cisgender men who have sex with men and transgender women who have sex with men, both with Diseases Department, Hopitaux Saint-Louis a high risk of acquiring HIV on the basis of their self-reported sexual behaviour in the past 12 weeks or their Lariboisière, University of Paris recent history (within 24 weeks of enrolment) of bacterial sexually transmitted infections. -

Injectable Antiretroviral Drugs: Back to the Future
viruses Review Injectable Antiretroviral Drugs: Back to the Future Marco Berruti 1 , Niccolò Riccardi 2, Diana Canetti 3,4 , Sergio Lo Caputo 5 , Lucia Taramasso 6 and Antonio Di Biagio 1,6,* 1 Infectious Diseases Unit, Department of Health Sciences (DISSAL), University of Genoa, 16132 Genoa, Italy; [email protected] 2 Department of Infectious-Tropical Diseases and Microbiology, IRCCS Sacro Cuore Don Calabria Hospital, Negrar di Valpolicella, 37024 Verona, Italy; [email protected] 3 Clinic of Infectious Diseases, IRCCS San Raffaele Scientific Institute, 20097 Milan, Italy; [email protected] 4 School of Medicine, Vita-Salute San Raffaele University, 20097 Milan, Italy 5 Clinic of Infectious Diseases, Department of Clinical and Experimental Medicine, University of Foggia, 71122 Foggia, Italy; [email protected] 6 Infectious Diseases Unit, Department of Internal Medicine, Ospedale Policlinico San Martino IRCCS, 16132 Genoa, Italy; [email protected] * Correspondence: [email protected] Abstract: Current HIV treatment regimens provide sustained virologic suppression, at least partially restore the immune system and have limited side effects; however, they do not allow viral eradication and they are burdened by daily pill intake with a life-long commitment for the people living with HIV (PHIV). Injectable agents might represent a turning point in the care of PHIV, allowing less frequent administration of antiretroviral treatment (ART), more widespread use of pre-exposure prophylaxis (PrEP) and more stable drug levels in the blood, thus increasing the odds to get closer to end the HIV pandemic. The aim of this manuscript is to give a comprehensive review of injectable antiretrovirals that have been used in the past, which are available now, will be available in the future, and their role in the treatment of HIV infection Citation: Berruti, M.; Riccardi, N.; Canetti, D.; Lo Caputo, S.; Taramasso, Keywords: ART; injectable; HIV; antiretroviral; treatment; PrEP L.; Di Biagio, A. -
Guidelines for the Use of Antiretroviral Agents in Adults and Adolescent Living With
Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV Developed by the DHHS Panel on Antiretroviral Guidelines for Adults and Adolescents – A Working Group of the Office of AIDS Research Advisory Council (OARAC) How to Cite the Adult and Adolescent Guidelines: Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. Department of Health and Human Services. Available at https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/ AdultandAdolescentGL.pdf. Accessed [insert date] [insert page number, table number, etc. if applicable] It is emphasized that concepts relevant to HIV management evolve rapidly. The Panel has a mechanism to update recommendations on a regular basis, and the most recent information is available on the HIVinfo Web site (http://hivinfo.nih.gov). What’s New in the Guidelines? August 16, 2021 Hepatitis C Virus/HIV Coinfection • Table 18 of this section has been updated to include recommendations regarding concomitant use of fostemsavir or long acting cabotegravir plus rilpivirine with different hepatitis C treatment regimens. June 3, 2021 What to Start • Since the release of the last guidelines, updated data from the Botswana Tsepamo study have shown that the prevalence of neural tube defects (NTD) associated with dolutegravir (DTG) use during conception is much lower than previously reported. Based on these new data, the Panel now recommends that a DTG-based regimen can be prescribed for most people with HIV who are of childbearing potential. Before initiating a DTG-based regimen, clinicians should discuss the risks and benefits of using DTG with persons of childbearing potential, to allow them to make an informed decision. -

This Project Has Been Supported with Unrestriced Grants from Abbvie Gilead Sciences HEXAL Janssen-Cilag MSD Viiv Healthcare By
This project has been supported with unrestriced grants from AbbVie Gilead Sciences HEXAL Janssen-Cilag MSD ViiV Healthcare By Marcus Altfeld, Hamburg/Boston (USA) Achim Barmeyer, Dortmund Georg Behrens, Hannover Dirk Berzow, Hamburg Christoph Boesecke, Bonn Patrick Braun, Aachen Thomas Buhk, Hamburg Rob Camp, Barcelona (Spain/USA) Rika Draenert, Munich Christian Eggers, Linz (Austria) Stefan Esser, Essen Gerd Fätkenheuer, Cologne Gunar Günther, Windhoek (Namibia) Thomas Harrer, Erlangen Christian Herzmann, Borstel Christian Hoffmann, Hamburg Heinz-August Horst, Kiel Martin Hower, Dortmund Christoph Lange, Borstel Thore Lorenzen, Hamburg Tim Niehues, Krefeld Christian Noah, Hamburg Ramona Pauli, Munich Ansgar Rieke, Koblenz Jürgen Kurt Rockstroh, Bonn Thorsten Rosenkranz, Hamburg Bernhard Schaaf, Dortmund Ulrike Sonnenberg-Schwan, Munich Christoph D. Spinner, Munich Thomas Splettstoesser (Figures), Berlin Matthias Stoll, Hannover Hendrik Streeck, Essen/Boston (USA) Jan Thoden, Freiburg Markus Unnewehr, Dortmund Mechthild Vocks-Hauck, Berlin Jan-Christian Wasmuth, Bonn Michael Weigel, Schweinfurt Thomas Weitzel, Santiago (Chile) Eva Wolf, Munich HIV 2015/16 www.hivbook.com Edited by Christian Hoffmann and Jürgen K. Rockstroh Medizin Fokus Verlag IV Christian Hoffmann, M.D., Ph.D. ICH Stadtmitte (Infektionsmedizinisches Centrum Hamburg) Glockengiesserwall 1 20095 Hamburg, Germany Phone: + 49 40 2800 4200 Fax: + 49 40 2800 42020 [email protected] Jürgen K. Rockstroh, M.D., Ph.D. Department of Medicine I University of Bonn Sigmund-Freud-Strasse 25 53105 Bonn, Germany Phone: + 49 228 287 6558 Fax: + 49 228 287 5034 [email protected] HIV Medicine is an ever-changing field. The editors and authors of HIV 2015/16 have made every effort to provide information that is accurate and complete as of the date of publication. -
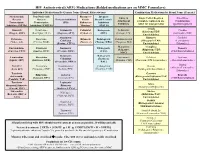
HIV Antiretroviral (ARV) Medications (Bolded Medications Are on MMC
HIV Antiretroviral (ARV) Medications (Bolded medications are on MMC Formulary) Individual Medications By Generic Name (Brand, Abbreviation) Combination Medications by Brand Name (Generic) Nucleos(t)ide Non-Nucleoside Pharmaco- Integrase Entry & Single Tablet Regimen Fixed Dose Reverse Reverse Protease Inhibitors kinetic Strand Transfer Attachment (complete regimen in one Combination Transcriptase Transcriptase (PIs) Enhancers Inhibitors Inhibitors tablet for most patients) (partial regimen) Inhibitors (NRTIs) Inhibitors (NNRTIs) “Boosters” (INSTIs) Atripla Abacavir Delavirdine Atazanavir Cobicistat Bictegravir Enfuvirtide Cimduo (Efavirenz/TDF/ (Ziagen, ABC) (Rescriptor, DLV) (Reyataz, ATV) (Tybost, c) (BIC) (Fuzeon, T20) (Lamivudine/TDF) Emtricitabine) Atazanavir/ Biktarvy Combivir Didanosine Doravirine Ritonavir Dolutegravir Ibalizumab-uiyk Cobicistat (Bictegravir/TAF/ (Lamivudine/ (Videx, ddl) (Pifeltro, DOR) (Norvir, r) (Tivicay, DTG) (Trogarzo, IBA) (Evotaz, ATV/c) Emtricitabine) Zidovudine) Maraviroc Complera Emtricitabine Efavirenz Darunavir Elvitegravir Descovy (Selzentry, (Rilpivirine/TDF/ (Emtriva, FTC) (Sustiva, EFV) (Prezista, DRV) (EVG) (TAF/Emtricitabine) MVC) Emtricitabine) Darunavir/ Raltegravir Lamivudine Etravirine Fostemsavir Delstrigo Epzicom Cobisistat (Isentress, (Epivir, 3TC) (Intelence, ETR) (Rukobia, FTR) (Doravirine/TDF/Lamivudine) (Abacavir/Lamivudine) (Prezcobix, DRV/c) RAL) Trizivir Stavudine Nevirapine Fosamprenavir Cabotegravir Dovato (Abacavir/Lamivudine/ (Viramune, NVP) (Lexiva, FPV) (Vocabria, CAB) (Dolutegravir/Lamivudine) -

Global HIV Prevention Study to Stop Early After Viiv Healthcare's Long
Issued: 18 May 2020, London UK – LSE announcement Global HIV prevention study to stop early after ViiV Healthcare’s long-acting injectable formulation of cabotegravir dosed every two months shows higher efficacy than daily oral PrEP • Interim analysis from HPTN 083 study shows investigational, long-acting injectable cabotegravir (CAB LA) administered every two months is 69% more effective than daily pills in preventing HIV acquisition • Participants who were in the daily oral emtricitabine/tenofovir disoproxil fumarate 200 mg and 300 mg (FTC/TDF) tablet arm of the study will be offered CAB LA London, 18 May 2020 – ViiV Healthcare, the global specialist HIV company majority owned by GSK, with Pfizer Inc. and Shionogi Limited as shareholders, today announced the interim analysis of the HIV Prevention Trials Network (HPTN) 083 study evaluating the safety and efficacy of investigational, long- acting, injectable cabotegravir for HIV prevention. In the study cabotegravir was found to be 69% more effective (95% CI 41%-84%) in preventing HIV acquisition in men who have sex with men (MSM) and transgender women who have sex with men when compared to the current standard of care, daily oral emtricitabine/tenofovir disoproxil fumarate 200 mg and 300 mg (FTC/TDF) tablets. The study achieved its primary objective of non-inferiority with the difference approaching superiority in favour of cabotegravir, pending final analysis. The HPTN 083 study, with approximately 4,600 participants across more than 40 sites in North and South America, Asia, and Africa, is one of the first-ever clinical trials to directly compare two active prevention agents. In a planned interim review, the independent Data and Safety Monitoring Board (DSMB) found the study data clearly indicated that long-acting injectable cabotegravir was highly effective at preventing HIV in the study population. -

The Impact of Modern Antiretroviral Therapy on Lipid Metabolism of HIV-1 Infected Patients
Chapter 6 The Impact of Modern Antiretroviral Therapy on Lipid Metabolism of HIV-1 Infected Patients Joel da Cunha, Luciana Morganti Ferreira Maselli, Sérgio Paulo Bydlowski and Celso Spada Additional information is available at the end of the chapter http://dx.doi.org/10.5772/61061 1. Introduction The highly active antiretroviral therapy (HAART) is the most efficient and safe alternative against HIV-1 infection, to allow the restoration of the immune system, with consequent reduction in mortality rate, increased survival and quality of life of infected patients. Apart from the great benefits of the use of different HAART regimens, laboratory and clinical experience has shown that HAART can induce severe and considerable adverse effects on metabolic complications of lipid metabolism, characterized by signs of dyslipidemia, increased risk of cardiovascular disease and even an increased risk of atherosclerosis. In this context, the class of protease inhibitors has been associated with a higher level of changes of lipid metab‐ olism and an increased risk for cardiovascular disease. In turn, the search for different therapeutic strategies to reverse HAART-associated lipid disorders has led to the use of less metabolically active antiretroviral drugs without compromising antiretroviral efficacy. Thus, the different interactions of antiretroviral drugs are recommended based on their degree of impact on lipid metabolism. Recently, fusion inhibitors, integrase strand transfer inhibitors, entry inhibitors, have been included in the therapeutic arsenal against HIV-1 infection, and are not associated with metabolic disorders, since their mechanisms of action are different from other classes of antiretrovirals. Instead, the use of hypolipidemic drug therapy (statins, fibrates, inhibitors of intestinal cholesterol) becomes necessary when HAART-associated dyslipidemia occurs or persists for a long period and when alterations in diet, exercise and other HAART strategies are ineffective. -

Cabotegravir
Paper No. 18 Utilization of Physiologically Based Pharmacokinetic Modelling (PBPK) to predict the effect of UGT enzyme inhibition and induction on the systemic exposure of Cabotegravir Kunal Taskar1, Parul Patel2, Simon Cozens1, Helen Tracey1, Jackie Bloomer1, Kelong Han3, Susan Ford3, Mark Baker4 and Aarti Patel1 1GlaxoSmithKline, Ware, UK; 2ViiV Healthcare, RTP, USA; 3GlaxoSmithKline, PA, USA; 4 ViiV Healthcare, Nyon, Switzerland. Disclosure • Aarti Patel is a full time employee of GlaxoSmithKline Proprietary and Confidential Introduction and PBPK Strategy Cabotegravir (CAB) is an HIV integrase inhibitor in Workflow for CAB PBPK Model Development, Verification, development for HIV treatment for monthly Application and Software Qualification administration as part of a combination dual therapy regimen with rilpivirine, and as monotherapy for HIV prevention. CAB undergoes glucuronidation via UGT1A1 with a minor contribution from UGT1A9. In HIV/TB coinfection, co-administration with anti-TB agents, rifampin or rifabutin, may be required. Rifampin is a potent UGT inducer and reduced oral plasma CAB exposure by 59% in the clinic. Reduction of only 21% was observed with rifabutin which is a weak UGT inducer. UGT inhibition effects on CAB exposure have not been clinically investigated. A physiologically based pharmacokinetic (PBPK) model of CAB was developed and verified to prospectively assess the impact of potent UGT inhibition by atazanavir (1A1) or mefenamic acid (1A9), and of a weak UGT1A1 inducer, phenobarbital. CAB Model Development, Verification and Software Qualification Key Input parameters for CAB PBPK Model in Simcyp®v17 Simulated and Observed CAB Plasma Profiles Following Single and Repeat 30 mg CAB Oral Dose Parameter Value Source 10 100 Molecular Weight 405.4 Measured value Log P 1.58 Measured value 1 10 pKa 7.71 Measured value 0.1 Fraction unbound in 0.006 Measured value from (µg/mL) (µg/mL) plasma (Fu) clinical and in vitro 1 investigations.