Enhanced Delivery of Actives Through Skin from Patches
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Long-Acting Cabotegravir: the Future of HIV Prep
Long-Acting Injectable Cabotegravir: the Future of HIV PrEP? Brian R. Wood, MD Associate Professor of Medicine University of Washington Mountain West AIDS Education & Training Center June 4, 2020 Disclosures No conflicts of interest or relationships to disclose. Will be discussing an investigational antiretroviral. Full HPTN 083 study results not yet available. Will be reviewing data from a preliminary DSMB analysis today. See press release and webinar: https://www.hptn.org/news-and-events/announcements/cab- la-proves-be-highly-effective-prevention-hiv-acquisition Outline • General notes about cabotegravir • News from the phase 3 PrEP trial (and why it’s a big deal) • Questions, concerns, and next steps for long-acting PrEP What is Cabotegravir? Cabotegravir (CAB) • Investigational integrase strand transfer inhibitor • Potential infrequent dosing and parenteral administration - Oral half-life: 40 hours - Parenteral nanosuspension (IM, SC) half-life: 21-50 days - Median time from discontinuation to undetectable plasma level (IM, SC): 43-66 weeks • Metabolized by UGT1A1 (main pathway) & UGT1A9 - Minimal CYP metabolism; likely few drug interactions • Relatively low barrier to resistance Aidsinfo.nih.gov/drugs Injectable Long-Acting Cabotegravir Image courtesy of Dr. Raphael Landovitz, UCLA What is the HPTN 083 Trial and What’s the Big News? HPTN 083 A Phase 2b/3 Double Blind Safety and Efficacy Study of Injectable Cabotegravir Compared to Daily Oral TDF/FTC, for Pre-Exposure Prophylaxis in HIV-Uninfected Cisgender Men and TranHPTNsgender Women wh o 083have Sex wi thSites Men – Phase 2b/3 Target enrollment: 4,500 HIV- uninfected cisgender men and transgender 45 Sites in 8 Countrieswomen who have sex with men and who are at risk of HIV acquisition Primary outcome: HIV Prevention effectiveness of cabotegravir compared to daily oral TDF/FTC United States India Vietnam Thailand Peru Brazil South Argentina Africa ClinicalTrials.gov Identifier: NCT02720094 Slide courtesy of Dr. -
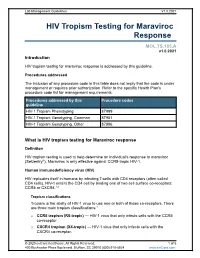
HIV Tropism Testing for Maraviroc Response
Lab Management Guidelines V1.0.2021 HIV Tropism Testing for Maraviroc Response MOL.TS.185.A v1.0.2021 Introduction HIV tropism testing for maraviroc response is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline HIV-1 Tropism Phenotyping 87999 HIV-1 Tropism Genotyping, Common 87901 HIV-1 Tropism Genotyping, Other 87906 What is HIV tropism testing for Maraviroc response Definition HIV tropism testing is used to help determine an individual's response to maraviroc (Selzentry®). Maraviroc is only effective against CCR5-tropic HIV-1. Human immunodeficiency virus (HIV) HIV replicates itself in humans by infecting T-cells with CD4 receptors (often called CD4 cells). HIV-1 enters the CD4 cell by binding one of two cell surface co-receptors: CCR5 or CXCR4.1,2 Tropism classifications Tropism is the ability of HIV-1 virus to use one or both of these co-receptors. There are three main tropism classifications:3 o CCR5 tropism (R5-tropic) — HIV-1 virus that only infects cells with the CCR5 co-receptor. o CXCR4 tropism (X4-tropic) — HIV-1 virus that only infects cells with the CXCR4 co-receptor. © 2020 eviCore healthcare. All Rights Reserved. 1 of 5 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2021 o Dual or mixed tropism (D/M-tropic) — HIV-1 virus populations that can use either co-receptor to infect cells. -

LATTE Study Oral Cabotegravir + Rilpivirine Versus Efavirenz + 2 NRTI’S LATTE Study: Design
Oral Cabotegravir + Rilpivirine versus Efavirenz + 2 NRTI’s LATTE Study Oral Cabotegravir + Rilpivirine versus Efavirenz + 2 NRTI’s LATTE Study: Design Study Design: CAB 10 mg CAB 10 mg + 2 NRTI’s + RPV 25 mg • BacKground: Phase 2b, (n = 60) (n = 52) randoMized, partially blinded study done at Multiple centers CAB 30 mg CAB 30 mg in the U.S. and Canada + 2 NRTI’s + RPV 25 mg (n = 60) (n = 51) • Inclusion Criteria (n = 244) - Age ≥18 years - Antiretroviral-naïve CAB 60 mg CAB 60 mg - HIV RNA >1,000 copies/ML + 2 NRTI’s + RPV 25 mg - CD4 count >200 cells/MM3 (n = 61) (n = 53) - CrCl >50 ML/Min - No hepatitis B Efavirenz 600 mg Efavirenz 600 mg - No significant transaMinitis + 2 NRTI’s + 2 NRTI’s (n = 62) (n = 46) 24-week lead-in phase Source: Margolis DA, et al. Lancet Infect Dis. 2015;15:1145-55. Oral Cabotegravir + Rilpivirine versus Efavirenz + 2 NRTI’s LATTE Study: Results Cabotegravir + 2NRTIs Cabotegravir + Rilpivirine Efavirenz + 2NRTIs Induction* Maintenance* 100 80 86 82 76 74 71 60 63 40 HIV RNA <50 copies/mL (%) <50 copies/mL HIV RNA 20 156/181 46/62 149/181 44/62 137/181 39/62 0 Week 24 Week 48 Week 96 *Cabotegravir data is composite of all cabotegravir doses Source: Margolis DA, et al. Lancet Infect Dis. 2015;15:1145-55. Oral Cabotegravir + Rilpivirine versus Efavirenz + 2 NRTI’s LATTE Study: Results 100 Induction* Maintenance 80 60 Cabotegravir 10 mg + Rilpivirine 40 Cabotegravir 30 mg + Rilpivirine HIV RNA <40 copies/mL HIV RNA 20 Cabotegravir 60 mg + Rilpivirine Efavirenz 600 mg + 2NRTIs 0 0 12 24 36 48 60 72 84 96 Treatment Week *During induction phase cabotegravir administered with investigator chosen 2NRTIs Source: Margolis DA, et al. -

Review CCR5 Antagonists: Host-Targeted Antivirals for the Treatment of HIV Infection
Antiviral Chemistry & Chemotherapy 16:339–354 Review CCR5 antagonists: host-targeted antivirals for the treatment of HIV infection Mike Westby* and Elna van der Ryst Pfizer Global R&D, Kent, UK *Corresponding author: Tel: +44 1304 649876; Fax: +44 1304 651819; E-mail: [email protected] The human chemokine receptors, CCR5 and suggest that these compounds have a long plasma CXCR4, are potential host targets for exogenous, half-life and/or prolonged CCR5 occupancy, which small-molecule antagonists for the inhibition of may explain the delay in viral rebound observed HIV-1 infection. HIV-1 strains can be categorised by following compound withdrawal in short-term co-receptor tropism – their ability to utilise CCR5 monotherapy studies. A switch from CCR5 to (CCR5-tropic), CXCR4 (CXCR4-tropic) or both (dual- CXCR4 tropism occurs spontaneously in approxi- tropic) as a co-receptor for entry into susceptible mately 50% of HIV-infected patients and has been cells. CCR5 may be the more suitable co-receptor associated with, but is not required for, disease target for small-molecule antagonists because a progression. The possibility of a co-receptor natural deletion in the CCR5 gene preventing its tropism switch occurring under selection pressure expression on the cell surface is not associated by CCR5 antagonists is discussed. The completion with any obvious phenotype, but can confer of ongoing Phase IIb/III studies of maraviroc, resistance to infection by CCR5-tropic strains – the aplaviroc and vicriviroc will provide further insight most frequently sexually-transmitted strains. into co-receptor tropism, HIV pathogenesis and The current leading CCR5 antagonists in clinical the suitability of CCR5 antagonists as a potent development include maraviroc (UK-427,857, new class of antivirals for the treatment of HIV Pfizer), aplaviroc (873140, GlaxoSmithKline) and infection. -

Product Monograph for CELSENTRI
PRODUCT MONOGRAPH PrCELSENTRI maraviroc Tablets 150 and 300 mg CCR5 antagonist ViiV Healthcare ULC 245, boulevard Armand-Frappier Laval, Quebec H7V 4A7 Date of Revision: July 05, 2019 Submission Control No: 226222 © 2019 ViiV Healthcare group of companies or its licensor. Trademarks are owned by or licensed to the ViiV Healthcare group of companies. Page 1 of 60 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION.........................................................3 SUMMARY PRODUCT INFORMATION ........................................................................3 INDICATIONS AND CLINICAL USE..............................................................................3 CONTRAINDICATIONS ...................................................................................................3 WARNINGS AND PRECAUTIONS..................................................................................4 ADVERSE REACTIONS....................................................................................................9 DRUG INTERACTIONS ..................................................................................................19 DOSAGE AND ADMINISTRATION..............................................................................28 OVERDOSAGE ................................................................................................................31 ACTION AND CLINICAL PHARMACOLOGY ............................................................31 STORAGE AND STABILITY..........................................................................................36 -

PATIENT INFORMATION STRIBILD® (STRY-Bild) (Elvitegravir, Cobicistat
PATIENT INFORMATION STRIBILD® (STRY-bild) (elvitegravir, cobicistat, emtricitabine, and tenofovir disoproxil fumarate) tablets Important: Ask your healthcare provider or pharmacist about medicines that should not be taken with STRIBILD. For more information, see the section “What should I tell my healthcare provider before taking STRIBILD?” What is the most important information I should know about STRIBILD? STRIBILD can cause serious side effects, including: • Worsening of Hepatitis B infection. If you have hepatitis B virus (HBV) infection and take STRIBILD, your HBV may get worse (flare-up) if you stop taking STRIBILD. A “flare-up” is when your HBV infection suddenly returns in a worse way than before. o Do not run out of STRIBILD. Refill your prescription or talk to your healthcare provider before your STRIBILD is all gone. o Do not stop taking STRIBILD without first talking to your healthcare provider. o If you stop taking STRIBILD, your healthcare provider will need to check your health often and do blood tests regularly for several months to check your HBV infection. Tell your healthcare provider about any new or unusual symptoms you may have after you stop taking STRIBILD. See “What are the possible side effects of STRIBILD?” for more information about side effects. What is STRIBILD? STRIBILD is a prescription medicine that is used without other antiretroviral medicines to treat Human Immunodeficiency Virus-1 (HIV-1) in people 12 years of age and older: • who have not received anti-HIV-1 medicines in the past, or • to replace their current anti-HIV-1 medicines: o in people who have been on the same anti-HIV-1 medicine regimen for at least 6 months, and o who have an amount of HIV-1 in their blood (this is called “viral load”) that is less than 50 copies/mL, and o have never failed past HIV-1 treatment. -

(KPIC) PPO and Out-Of- Area Indemnity (OOA) Drug Formulary with Specialty Drug Tier
Kaiser Permanente Insurance Company (KPIC) PPO and Out-of- Area Indemnity (OOA) Drug Formulary with Specialty Drug Tier This Drug Formulary was updated: September 1, 2021 NOTE: This drug formulary is updated often and is subject to change. Upon revision, all previous versions of the drug formulary are no longer in effect. This document contains information regarding the drugs that are covered when you participate in the California Nongrandfathered PPO and Out-of- Area Indemnity (OOA) Health Insurance Plans with specialty drug tier offered by Kaiser Permanente Insurance Company (KPIC) and fill your prescription at a MedImpact network pharmacy. Access to the most current version of the Formulary can be obtained by visiting kp.org/kpic-ca-rx-ppo-ngf. For help understanding your KPIC insurance plan benefits, including cost sharing for drugs under the prescription drug benefit and under the medical benefit, please call 1-800-788-0710 or 711 (TTY) Monday through Friday, 7a.m. to 7p.m. For help with this Formulary, including the processes for submitting an exception request and requesting prior authorization and step therapy exceptions, please call MedImpact 24 hours a day, 7 days a week, at 1-800-788-2949 or 711 (TTY). For cost sharing information for the outpatient prescription drug benefits in your specific plan, please visit: kp.org/kpic-ca-rx-ppo-ngf. For help in your preferred language, please see the Kaiser Permanente Insurance Company Notice of Language Assistance in this document. KPIC PPO NGF Table of Contents Informational Section................................................................................................................................2 -

Elvitegravir, Cobicistat, Emtricitabine, and Tenofovir Alafenamide
PATIENT & CAREGIVER EDUCATION Elvitegravir, Cobicistat, Emtricitabine, and Tenofovir Alafenamide This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. Brand Names: US Genvoya Brand Names: Canada Genvoya Warning Hepatitis B has gotten worse when this drug was stopped in some people with hepatitis B. Close follow-up for a few months is needed when therapy is stopped in people who have hepatitis B. Do not stop giving this drug to your child without calling your child’s doctor. Hepatitis B testing needs to be done as you were told by the doctor. Talk with the doctor. Elvitegravir, Cobicistat, Emtricitabine, and Tenofovir Alafenamide 1/9 What is this drug used for? It is used to treat HIV infection. What do I need to tell the doctor BEFORE my child takes this drug? If your child is allergic to this drug; any part of this drug; or any other drugs, foods, or substances. Tell the doctor about the allergy and what signs your child had. If your child has any of these health problems: Kidney disease or liver disease. If your child takes any drugs (prescription or OTC, natural products, vitamins) that must not be taken with this drug, like certain drugs that are used for high cholesterol, migraines, or mood problems. There are many drugs that must not be taken with this drug. If your child is taking any other drugs to treat HIV. If your child is pregnant: Do not give this drug to your child during pregnancy. -

The CCR5-Delta32 Variant Might Explain Part of the Association Between COVID-19 and the Chemokine-Receptor Gene Cluster
medRxiv preprint doi: https://doi.org/10.1101/2020.11.02.20224659; this version posted November 4, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. The CCR5-delta32 variant might explain part of the association between COVID-19 and the chemokine-receptor gene cluster 1,8,12* 1,8* 2,8,9,10,11 Juan Gómez, Elías Cuesta-Llavona, Guillermo M. Albaiceta, Marta 3 4,8,9,12 2,8,10,11 García-Clemente, Carlos López-Larrea, Laura Amado-Rodríguez, Inés 8,10 3 3 1,8 1,8 López-Alonso, Tamara Hermida, Ana I. EnrÍquez, Helena Gil , Belén Alonso, 1,8 1 1,8,9,12 Sara Iglesias, Beatriz Suarez-Alvarez,4,8,12 Victoria Alvarez, Eliecer Coto *These authors contributed equally to this work. 1 Genética Molecular, Hospital Universitario Central Asturias, Oviedo, Spain. 2 Unidad de Cuidados Intensivos Cardiológicos, Hospital Universitario Central Asturias, Oviedo, Spain. 3 Neumología, Hospital Universitario Central Asturias, Oviedo, Spain. 4 Inmunología, Hospital Universitario Central Asturias, Oviedo, Spain. 5 Urgencias, Hospital Universitario Central Asturias, Oviedo, Spain. 8 Instituto de Investigación Sanitaria del Principado deAsturias, ISPA, Oviedo, Spain. 9 Universidad de Oviedo, Oviedo, Spain. 10 CIBER-Enfermedades Respiratorias. Instituto de Salud Carlos III. Madrid, Spain. 11 Instituto Universitario de Oncología del Principado de Asturias. Oviedo, Spain. 12 Red de Investigación Renal (REDINREN), Madrid, Spain. Correspondenceto: Dr.EliecerCoto Hospital Univ. Central Asturias 33011 – Oviedo – Spain Tel. 34.985.10.55.00 Email: [email protected] 1 NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. -

EVOTAZ (Atazanavir Or Cobicistat) to Pregnant Rats and Rabbits (See Data)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Assess creatinine clearance (CLcr) before initiating treatment. Consider These highlights do not include all the information needed to use EVOTAZ alternative medications that do not require dosage adjustments in patients safely and effectively. See full prescribing information for EVOTAZ. with renal impairment. (5.3) • When cobicistat, a component of EVOTAZ, is used in combination with a EVOTAZ (atazanavir and cobicistat) tablet, for oral use tenofovir disoproxil fumarate (tenofovir DF)-containing regimen, cases of Initial U.S. Approval: 2015 acute renal failure and Fanconi syndrome have been reported. (5.4) • When used with tenofovir DF, assess urine glucose and urine protein at ---------------------------RECENT MAJOR CHANGES-------------------------- baseline and monitor CLcr, urine glucose, and urine protein. Monitor serum Indications and Usage phosphorus in patients with or at risk for renal impairment. Coadministration Indications (1.1) 07/2020 with tenofovir DF is not recommended in patients with CLcr below 70 Dosage and Administration mL/min or in patients also receiving a nephrotoxic agent. (5.4) Laboratory Testing Prior to Initiation and During • Chronic kidney disease has been reported during postmarketing surveillance Treatment with EVOTAZ (2.1) 04/2020 in patients with HIV-1 infection treated with atazanavir, with or without Recommended Dosage (2.2) 07/2020 ritonavir. Consider alternatives in patients at high risk for renal disease or Not Recommended During Pregnancy (2.5) 04/2020 with preexisting renal disease. Monitor renal laboratory tests prior to therapy Contraindications (4) 04/2020 and during treatment with EVOTAZ. Consider discontinuation of EVOTAZ Warnings and Precautions in patients with progressive renal disease. (5.5) Immune Reconstitution Syndrome (5.11) 07/2020 • Nephrolithiasis and cholelithiasis have been reported. -
Australian Public Assessment Report for Maraviroc
Australian Public Assessment Report for Maraviroc Proprietary Product Name: Celsentri Sponsor: ViiV Healthcare Pty Ltd May 2013 Therapeutic Goods Administration About the Therapeutic Goods Administration (TGA) • The Therapeutic Goods Administration (TGA) is part of the Australian Government Department of Health and Ageing, and is responsible for regulating medicines and medical devices. • The TGA administers the Therapeutic Goods Act 1989 (the Act), applying a risk management approach designed to ensure therapeutic goods supplied in Australia meet acceptable standards of quality, safety and efficacy (performance), when necessary. • The work of the TGA is based on applying scientific and clinical expertise to decision- making, to ensure that the benefits to consumers outweigh any risks associated with the use of medicines and medical devices. • The TGA relies on the public, healthcare professionals and industry to report problems with medicines or medical devices. TGA investigates reports received by it to determine any necessary regulatory action. • To report a problem with a medicine or medical device, please see the information on the TGA website <http://www.tga.gov.au>. About AusPARs • An Australian Public Assessment Record (AusPAR) provides information about the evaluation of a prescription medicine and the considerations that led the TGA to approve or not approve a prescription medicine submission. • AusPARs are prepared and published by the TGA. • An AusPAR is prepared for submissions that relate to new chemical entities, generic medicines, major variations, and extensions of indications. • An AusPAR is a static document, in that it will provide information that relates to a submission at a particular point in time. • A new AusPAR will be developed to reflect changes to indications and/or major variations to a prescription medicine subject to evaluation by the TGA. -

Cobicistat + Elvitegravir + Emtricitabine + Tenofovir Alfenamide
20, AVENUE APPIA – CH-1211 GENEVA 27 – SWITZERLAND – TEL CENTRAL +41 22 791 2111 – FAX CENTRAL +41 22 791 3111 – WWW.WHO.INT Comments on EML application : cobicistat + elvitegravir + emtricitabine + tenofovir alfenamide The WHO HIV Department does not support the addition of the formulation cobicistat + elvitegravir + emtricitabine + tenofovir alfenamide in 2017 WHO Model List of Essential Medicines for treatment of HIV infection for the following reasons Cobicisitat( COBI), elvitegravir (EVG) and tenofovir alfenamide (TAF) are not included as options in 2016 WHO consolidated guidelines on use of antiretrovirals for treating and preventing of HIV infection 1. A recent WHO systematic review comparing the use of integrase inhibitors in 1st line showed that dolutegravir and raltegravir were superior to elvitegravir/cobicistat (EVG/COBI) in terms of viral suppression, CD4 recovery and risk of treatment discontinuation.2 There are important concerns with the use of TAF and EVG/COBI in TB co-infection. EGV/COBI has important and well documented drug interactions with rifampicin and must not be co-administrated, as will result in loss of its antiviral effect3 4 Regarding TAF, there are no published data available on the pharmacokinetics and real-world efficacy of TAF in TB- coinfected patients. While the current available tenofovir prodrug (tenofovir disoproxil fumarate or TDF) does not require dose-adjustment if co-administered with rifampicin, TAF is currently contraindicated by the originator in patients being treated with rifampicin, as significant drug interaction is predicted based on pK modelling 56. Data on the potential for TAF dose adjustment are awaited. There are very limited data available on the safety of EVG/COBI and TAF during pregnancy.