A Randomized, Controlled Study on the Safety and E Cacy of Maraviroc
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
HIV Tropism Testing for Maraviroc Response
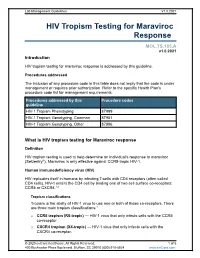
Lab Management Guidelines V1.0.2021 HIV Tropism Testing for Maraviroc Response MOL.TS.185.A v1.0.2021 Introduction HIV tropism testing for maraviroc response is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline HIV-1 Tropism Phenotyping 87999 HIV-1 Tropism Genotyping, Common 87901 HIV-1 Tropism Genotyping, Other 87906 What is HIV tropism testing for Maraviroc response Definition HIV tropism testing is used to help determine an individual's response to maraviroc (Selzentry®). Maraviroc is only effective against CCR5-tropic HIV-1. Human immunodeficiency virus (HIV) HIV replicates itself in humans by infecting T-cells with CD4 receptors (often called CD4 cells). HIV-1 enters the CD4 cell by binding one of two cell surface co-receptors: CCR5 or CXCR4.1,2 Tropism classifications Tropism is the ability of HIV-1 virus to use one or both of these co-receptors. There are three main tropism classifications:3 o CCR5 tropism (R5-tropic) — HIV-1 virus that only infects cells with the CCR5 co-receptor. o CXCR4 tropism (X4-tropic) — HIV-1 virus that only infects cells with the CXCR4 co-receptor. © 2020 eviCore healthcare. All Rights Reserved. 1 of 5 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2021 o Dual or mixed tropism (D/M-tropic) — HIV-1 virus populations that can use either co-receptor to infect cells. -

Review CCR5 Antagonists: Host-Targeted Antivirals for the Treatment of HIV Infection
Antiviral Chemistry & Chemotherapy 16:339–354 Review CCR5 antagonists: host-targeted antivirals for the treatment of HIV infection Mike Westby* and Elna van der Ryst Pfizer Global R&D, Kent, UK *Corresponding author: Tel: +44 1304 649876; Fax: +44 1304 651819; E-mail: [email protected] The human chemokine receptors, CCR5 and suggest that these compounds have a long plasma CXCR4, are potential host targets for exogenous, half-life and/or prolonged CCR5 occupancy, which small-molecule antagonists for the inhibition of may explain the delay in viral rebound observed HIV-1 infection. HIV-1 strains can be categorised by following compound withdrawal in short-term co-receptor tropism – their ability to utilise CCR5 monotherapy studies. A switch from CCR5 to (CCR5-tropic), CXCR4 (CXCR4-tropic) or both (dual- CXCR4 tropism occurs spontaneously in approxi- tropic) as a co-receptor for entry into susceptible mately 50% of HIV-infected patients and has been cells. CCR5 may be the more suitable co-receptor associated with, but is not required for, disease target for small-molecule antagonists because a progression. The possibility of a co-receptor natural deletion in the CCR5 gene preventing its tropism switch occurring under selection pressure expression on the cell surface is not associated by CCR5 antagonists is discussed. The completion with any obvious phenotype, but can confer of ongoing Phase IIb/III studies of maraviroc, resistance to infection by CCR5-tropic strains – the aplaviroc and vicriviroc will provide further insight most frequently sexually-transmitted strains. into co-receptor tropism, HIV pathogenesis and The current leading CCR5 antagonists in clinical the suitability of CCR5 antagonists as a potent development include maraviroc (UK-427,857, new class of antivirals for the treatment of HIV Pfizer), aplaviroc (873140, GlaxoSmithKline) and infection. -

Product Monograph for CELSENTRI
PRODUCT MONOGRAPH PrCELSENTRI maraviroc Tablets 150 and 300 mg CCR5 antagonist ViiV Healthcare ULC 245, boulevard Armand-Frappier Laval, Quebec H7V 4A7 Date of Revision: July 05, 2019 Submission Control No: 226222 © 2019 ViiV Healthcare group of companies or its licensor. Trademarks are owned by or licensed to the ViiV Healthcare group of companies. Page 1 of 60 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION.........................................................3 SUMMARY PRODUCT INFORMATION ........................................................................3 INDICATIONS AND CLINICAL USE..............................................................................3 CONTRAINDICATIONS ...................................................................................................3 WARNINGS AND PRECAUTIONS..................................................................................4 ADVERSE REACTIONS....................................................................................................9 DRUG INTERACTIONS ..................................................................................................19 DOSAGE AND ADMINISTRATION..............................................................................28 OVERDOSAGE ................................................................................................................31 ACTION AND CLINICAL PHARMACOLOGY ............................................................31 STORAGE AND STABILITY..........................................................................................36 -

The CCR5-Delta32 Variant Might Explain Part of the Association Between COVID-19 and the Chemokine-Receptor Gene Cluster
medRxiv preprint doi: https://doi.org/10.1101/2020.11.02.20224659; this version posted November 4, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. All rights reserved. No reuse allowed without permission. The CCR5-delta32 variant might explain part of the association between COVID-19 and the chemokine-receptor gene cluster 1,8,12* 1,8* 2,8,9,10,11 Juan Gómez, Elías Cuesta-Llavona, Guillermo M. Albaiceta, Marta 3 4,8,9,12 2,8,10,11 García-Clemente, Carlos López-Larrea, Laura Amado-Rodríguez, Inés 8,10 3 3 1,8 1,8 López-Alonso, Tamara Hermida, Ana I. EnrÍquez, Helena Gil , Belén Alonso, 1,8 1 1,8,9,12 Sara Iglesias, Beatriz Suarez-Alvarez,4,8,12 Victoria Alvarez, Eliecer Coto *These authors contributed equally to this work. 1 Genética Molecular, Hospital Universitario Central Asturias, Oviedo, Spain. 2 Unidad de Cuidados Intensivos Cardiológicos, Hospital Universitario Central Asturias, Oviedo, Spain. 3 Neumología, Hospital Universitario Central Asturias, Oviedo, Spain. 4 Inmunología, Hospital Universitario Central Asturias, Oviedo, Spain. 5 Urgencias, Hospital Universitario Central Asturias, Oviedo, Spain. 8 Instituto de Investigación Sanitaria del Principado deAsturias, ISPA, Oviedo, Spain. 9 Universidad de Oviedo, Oviedo, Spain. 10 CIBER-Enfermedades Respiratorias. Instituto de Salud Carlos III. Madrid, Spain. 11 Instituto Universitario de Oncología del Principado de Asturias. Oviedo, Spain. 12 Red de Investigación Renal (REDINREN), Madrid, Spain. Correspondenceto: Dr.EliecerCoto Hospital Univ. Central Asturias 33011 – Oviedo – Spain Tel. 34.985.10.55.00 Email: [email protected] 1 NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. -
Australian Public Assessment Report for Maraviroc
Australian Public Assessment Report for Maraviroc Proprietary Product Name: Celsentri Sponsor: ViiV Healthcare Pty Ltd May 2013 Therapeutic Goods Administration About the Therapeutic Goods Administration (TGA) • The Therapeutic Goods Administration (TGA) is part of the Australian Government Department of Health and Ageing, and is responsible for regulating medicines and medical devices. • The TGA administers the Therapeutic Goods Act 1989 (the Act), applying a risk management approach designed to ensure therapeutic goods supplied in Australia meet acceptable standards of quality, safety and efficacy (performance), when necessary. • The work of the TGA is based on applying scientific and clinical expertise to decision- making, to ensure that the benefits to consumers outweigh any risks associated with the use of medicines and medical devices. • The TGA relies on the public, healthcare professionals and industry to report problems with medicines or medical devices. TGA investigates reports received by it to determine any necessary regulatory action. • To report a problem with a medicine or medical device, please see the information on the TGA website <http://www.tga.gov.au>. About AusPARs • An Australian Public Assessment Record (AusPAR) provides information about the evaluation of a prescription medicine and the considerations that led the TGA to approve or not approve a prescription medicine submission. • AusPARs are prepared and published by the TGA. • An AusPAR is prepared for submissions that relate to new chemical entities, generic medicines, major variations, and extensions of indications. • An AusPAR is a static document, in that it will provide information that relates to a submission at a particular point in time. • A new AusPAR will be developed to reflect changes to indications and/or major variations to a prescription medicine subject to evaluation by the TGA. -

Selected Properties of Maraviroc
Selected Properties of Maraviroc Other names UK-427,857, MVC, Celsentri , Selzentry (US) Manufacturer ViiV Healthcare ULC Pharmacology/Mechanism of Maraviroc is a selective, slowly reversible, small molecule Action antagonist of the interaction between human CCR5 and HIV-1 gp120. Blocking this interaction prevents CCR5-tropic HIV-1 entry into cells . CCR5 antagonists target a discrete step in the viral entry pathway. The mechanism of HIV entry into the host CD4 T cells involves a sequence of molecular interactions between the virion envelope glycoprotein (Env) and host cell surface receptors. Normally, the gp120 Env subunit binds to CD4, and subsequent binding of HIV to the host cell’s coreceptors (CCR5 or CXCR4) causes a conformational change leading to membrane fusion into the host cell. Allosteric binding of a CCR5 antagonist results in a receptor conformation that the virus cannot bind to, thus interfering with the fusion process. NB: Use of maraviroc is not recommended in patients with dual/mixed or CXCR4-tropic HIV-1 as efficacy was not demonstrated in a phase 2 study of this patient group. The mean EC value (50% effective concentration) for Activity 50 maraviroc against HIV-1 group M isolates (clades A to J) and group O isolates ranged from 0.1 to 1.25 nM (0.05 to 0.64 ng/mL) in cell culture. Mean potency against a range of CCR5- tropic clinical primary isolates: IC 90 2.03 nM (1.04 ng/mL). In 973 treatment-experienced HIV-1-infected subjects in studies A4001027 and A4001028, the C , baseline viral load, baseline min CD4, cell count and overall sensitivity score (OSS) were found to be important predictors of virologic success (defined as viral load < 400 copies/mL at 24 weeks). -

Emtricitabine and Tenofovir Alafenamide
HIGHLIGHTS OF PRESCRIBING INFORMATION ------------------------DOSAGE AND ADMINISTRATION---------------------- These highlights do not include all the information needed to use • Testing: Prior to initiation of DESCOVY, patients should be tested for DESCOVY safely and effectively. See full prescribing information hepatitis B virus infection, and estimated creatinine clearance, urine for DESCOVY. glucose and urine protein should be obtained. (2.1) • ® Recommended dosage: One tablet taken once daily with or without DESCOVY (emtricitabine and tenofovir alafenamide) tablets, for food in patients with body weight at least 25 kg and a creatinine oral use clearance greater than or equal to 30 mL per minute. (2.2) Initial U.S. Approval: 2015 • Renal impairment: DESCOVY is not recommended in patients with WARNING: POST TREATMENT ACUTE EXACERBATION OF estimated creatinine clearance below 30 mL per minute. (2.3) HEPATITIS B ----------------------DOSAGE FORMS AND STRENGTHS-------------------- See full prescribing information for complete boxed warning. Tablets: 200 mg of FTC and 25 mg of TAF (3) • DESCOVY is not approved for the treatment of chronic -------------------------------CONTRAINDICATIONS------------------------------ hepatitis B virus (HBV) infection. Severe acute None. exacerbations of hepatitis B have been reported in patients who are coinfected with HIV-1 and HBV and have -----------------------WARNINGS AND PRECAUTIONS----------------------- discontinued products containing emtricitabine (FTC) • Immune reconstitution syndrome: May necessitate further evaluation and/or tenofovir disoproxil fumarate (TDF), and may occur and treatment.(5.2) with discontinuation of DESCOVY. Hepatic function should • New onset or worsening renal impairment: Assess creatinine be monitored closely in these patients. If appropriate, clearance, urine glucose, and urine protein in all patients before initiation of anti-hepatitis B therapy may be warranted. -

SELZENTRY (Maraviroc) Tablets, for Oral Use • Hepatotoxicity Accompanied by Severe Rash Or Systemic Allergic Reaction
---------------------------------- CONTRAINDICATIONS --------------------------------- HIGHLIGHTS OF PRESCRIBING INFORMATION • SELZENTRY is contraindicated in patients with severe renal impairment These highlights do not include all the information needed to use or end-stage renal disease (ESRD) (CrCl less than 30 mL per minute) SELZENTRY safely and effectively. See full prescribing information for who are concomitantly taking potent CYP3A inhibitors or inducers. (4) SELZENTRY. -------------------------- WARNINGS AND PRECAUTIONS -------------------------- SELZENTRY (maraviroc) tablets, for oral use • Hepatotoxicity accompanied by severe rash or systemic allergic reaction, SELZENTRY (maraviroc) oral solution including potentially life-threatening events, has been reported. Hepatic Initial U.S. Approval: 2007 laboratory parameters including ALT, AST, and bilirubin should be obtained prior to starting SELZENTRY and at other time points during WARNING: HEPATOTOXICITY See full prescribing information for complete boxed warning. treatment as clinically indicated. If rash or symptoms or signs of hepatitis or allergic reaction develop, hepatic laboratory parameters should be • Hepatotoxicity has been reported which may be preceded by severe monitored and discontinuation of treatment should be considered. When rash or other features of a systemic allergic reaction (e.g., fever, administering SELZENTRY to patients with pre-existing liver eosinophilia, or elevated IgE). (5.1) dysfunction or who are co-infected with hepatitis B and/or C virus, • -

Cytokines and Chemokines in SARS-Cov-2 Infections—Therapeutic Strategies Targeting Cytokine Storm
biomolecules Review Cytokines and Chemokines in SARS-CoV-2 Infections—Therapeutic Strategies Targeting Cytokine Storm Alexandra Pum 1, Maria Ennemoser 1, Tiziana Adage 2 and Andreas J. Kungl 1,3,* 1 Institute Of Pharmaceutical Sciences, Karl-Franzens-University Graz, Schubertstrasse 1, 8010 Graz, Austria; [email protected] (A.P.); [email protected] (M.E.) 2 Brain Implant Therapeutics (BIT) Pharma, Leonhardstrasse 109, 8010 Graz, Austria; [email protected] 3 Antagonis Biotherapeutics GmbH, Strasserhofweg 77, 8045 Graz, Austria * Correspondence: [email protected] Abstract: The recently identified severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus, the cause of coronavirus disease (COVID-19) and the associated ongoing pandemic, frequently leads to severe respiratory distress syndrome and pneumonia with fatal consequences. Although several factors of this infection and its consequences are not completely clear, the presence and involvement of specific chemokines is undoubtedly crucial for the development and progression of COVID-19. Cytokine storm and the often-resulting cytokine release syndrome (CRS) are patho- physiological hallmarks in COVID-19 infections related to its most severe and fatal cases. In this hyperinflammatory event, chemokines and other cytokines are highly upregulated and are therefore not fulfilling their beneficial function in the host response anymore but causing harmful effects. Here, we present the recent views on the involvement of chemokines and selected cytokines in COVID-19 and the therapeutics currently in clinical development targeting or interfering with them, discussing their potentials in the treatment of COVID-19 infections. Keywords: chemokines; SARS-CoV-2; COVID-19; coronavirus; cytokine storm Citation: Pum, A.; Ennemoser, M.; Adage, T.; Kungl, A.J. -

Design, Chemical Synthesis and Biological Evaluation of Potential New Antiviral Agents
International Doctoral School in Biomolecular Sciences XXV Cycle Design, Chemical Synthesis and Biological Evaluation of Potential New Antiviral Agents Tutor Prof. Ines MANCINI University of Trento, Italy Ph.D. Thesis of Andrea DEFANT University of Trento, Italy 1 2 to my parents 3 4 Contents List of Abbreviations v List of Figures ix List of Schemes xii List of Tables xv Abstract 1 1. INTRODUCTION 3 1.1. Structure of HIV virion 4 1.2. HIV life cycle 6 1.3. Possible targets for anti-HIV agents and clinically used therapeutic agents 7 1.4. Reverse transcriptase enzyme 17 1.5. HIV-1 Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs) 19 1.6. Drug design of new potential NNRTI molecules 25 2. MATERIAL AND METHODS 37 2.1. Computational approach 37 2.2. Chemistry 37 2.2.1 General 38 2.2.2 Instruments 38 2.2.3 Chemical procedures of synthesis 2.3. Biological assays 39 2.3.1. ELISA enzymatic assay 39 2.3.2. In vitro anti-HIV activity 39 2.3.3. In vitro antiviral activity 39 2.3.4. Antibacterial activity 40 3. RESULTS 43 3.1. Drug design 43 3.1.1. Docking calculation 45 3.1.1.1. Proteins preparation 45 3.1.1.2. Preparation of ligands 46 3.1.1.3. Molecular docking 47 3.1.1.4 ADME and drug-like properties prediction 50 i 3.2. Chemical synthesis and structural characterization of the new molecules 55 3.2.1. Precursors 29, 30 and 35 58 3.2.2. Tosylate precursors 59 3.2.2.1. -

Recent Advances Targeting CCR5 for Cancer and Its Role in Immuno-Oncology Xuanmao Jiao1, Omar Nawab1,2,Tejal Patel2, Andrew V
Published OnlineFirst July 10, 2019; DOI: 10.1158/0008-5472.CAN-19-1167 Cancer Review Research Recent Advances Targeting CCR5 for Cancer and Its Role in Immuno-Oncology Xuanmao Jiao1, Omar Nawab1,2,Tejal Patel2, Andrew V. Kossenkov3, Niels Halama4, Dirk Jaeger4,5, and Richard G. Pestell1,3 Abstract Experiments of nature have revealed the peculiar impor- reexpression augments resistance to DNA-damaging agents tance of the G-protein–coupled receptor, C-C chemokine and is sufficient to induce cancer metastasis and "stemness". receptor type 5 (CCR5), in human disease since ancient times. Recent studies suggest important cross-talk between CCR5 The resurgence of interest in heterotypic signals in the onset signaling and immune checkpoint function. Because CCR5 and progression of tumorigenesis has led to the current focus onTregsservesasthecoreceptorforhumanimmunodefi- on CCR5 as an exciting new therapeutic target for metastatic ciency virus (HIV) entry, CCR5-targeted therapeutics used in cancer with clinical trials now targeting breast and colon HIV, [small molecules (maraviroc and vicriviroc) and a cancer. The eutopic expression of CCR5 activates calcium humanized mAb (leronlimab)], are now being repositioned signaling and thereby augments regulatory T cell (Treg) dif- in clinical trials as cancer therapeutics. As CCR5 is expressed ferentiation and migration to sites of inflammation. The mis- on a broad array of tumors, the opportunity for therapeutic expression of CCR5 in epithelial cells, induced upon onco- repositioning and the rationale for combination therapy genic transformation, hijacks this migratory phenotype. CCR5 approaches are reviewed herein. C-C Chemokine Receptor Type 5 and Signal is preserved in immune cells (3) and cancer cells (4, 5). -

Leronlimab, a Humanized Monoclonal Antibody to CCR5, Blocks Breast Cancer Metastasis and Enhances Cell Death Induced by DNA Dama
Leronlimab, a humanized monoclonal antibody to CCR5, blocks breast cancer metastasis and enhances cell death induced by DNA damaging chemotherapy Xuanmao Jiao1, Min Wang1, Zhiping Li1, Richard G. Pestell1, 2, 3, * 1Pennsylvania Cancer and Regenerative Medicine Research Center, Baruch S. Blumberg Institute, 3805 Old Easton Road, Doylestown, PA., 18902. 2CytoDyn Inc., 1111 Main St, Suite 660, Vancouver, WA, 98660. 3Lee Kong Chian School of Medicine, Nanyang Technological University, 637551, Singapore. Abstract 1.The binding of Leronlimab with CCR5 expressed in 2. The effects of PRO140 on CCL5 induced Ca2+ responses in breast cancer cells MDA-MB-231-CCR5 cells Purpose of the study. To assess binding and functional interaction of the humanized monoclonal antibody to CCR5 (Leronlimab) with A B A 20 sec before 60 sec after 240 sec after 60 sec after B C human breast cancer cell lines. The G protein coupled receptor CCR5, is adding CCL5 adding CCL5 adding CCL5 adding FBS FBS 4 CCL5 4 FBS - Leronlimab Leronlimab Leronlimab 1600 - 1600 CCL5 normally expressed on a subset of T cells and serves as a co-receptor 140 µg/ml 70 µg/ml 35 µg/ml 120 1200 1200 for HIV infection. During malignant transformation CCR5 expression is 100 800 800 80 known to increase in a number of cancers (breast cancer (BCa), Control 400 400 Mean FI of Fluo FI ofMean 60 Contro Fluo FI ofMean PRO140 prostate cancer, colon cancer, melanoma). CCR5 targeted cancer 0 l 0 40 0 200 400 600 800 1000 0 200 400 600 800 1000 clinical trials using small molecular inhibitors opened to accrual in late 20 Time Time (Sec) (Sec) binding to CCR5 (%) (%) CCR5 to binding 2018.