Lecture 21 Women's Reproductive Infectious Diseases And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Leucoplakic Vulva: Premalignant Determinants C
Henry Ford Hospital Medical Journal Volume 11 | Number 3 Article 3 9-1963 The Leucoplakic Vulva: Premalignant Determinants C. Paul Hodgkinson Roy B. P. Patton M. A. Ayers Follow this and additional works at: https://scholarlycommons.henryford.com/hfhmedjournal Part of the Life Sciences Commons, Medical Specialties Commons, and the Public Health Commons Recommended Citation Hodgkinson, C. Paul; Patton, Roy B. P.; and Ayers, M. A. (1963) "The Leucoplakic Vulva: Premalignant Determinants," Henry Ford Hospital Medical Bulletin : Vol. 11 : No. 3 , 279-287. Available at: https://scholarlycommons.henryford.com/hfhmedjournal/vol11/iss3/3 This Article is brought to you for free and open access by Henry Ford Health System Scholarly Commons. It has been accepted for inclusion in Henry Ford Hospital Medical Journal by an authorized editor of Henry Ford Health System Scholarly Commons. For more information, please contact [email protected]. Henry Ford Hosp. Med. Bull. Vol. 11, September, 1963 THE LEUCOPLAKIC VULVA Premalignant Determinants C. PAUL HODGKINSON, M.D.,* ROY B. P. PATTON, M.D., AND M. A. AYERS, M.D.* IN A PAPER proposing to discuss the leucoplakic vulva and any predisposing ten dency it may have to the development of squamous cell carcinoma, the term "pre malignant" has presumptuous connotations. This is presumptuous because it implies that more is known about cancer and its mode of development than can be supported by facts. What happens in the cell prior to the stage of carcinoma-in-situ is a burning and unsolved question in cancer research. How to detect and appraise the parameters of malignant potential is the essence of meaning connoted by the word "premalignant". -

Vaginitis and Abnormal Vaginal Bleeding
UCSF Family Medicine Board Review 2013 Vaginitis and Abnormal • There are no relevant financial relationships with any commercial Vaginal Bleeding interests to disclose Michael Policar, MD, MPH Professor of Ob, Gyn, and Repro Sciences UCSF School of Medicine [email protected] Vulvovaginal Symptoms: CDC 2010: Trichomoniasis Differential Diagnosis Screening and Testing Category Condition • Screening indications – Infections Vaginal trichomoniasis (VT) HIV positive women: annually – Bacterial vaginosis (BV) Consider if “at risk”: new/multiple sex partners, history of STI, inconsistent condom use, sex work, IDU Vulvovaginal candidiasis (VVC) • Newer assays Skin Conditions Fungal vulvitis (candida, tinea) – Rapid antigen test: sensitivity, specificity vs. wet mount Contact dermatitis (irritant, allergic) – Aptima TMA T. vaginalis Analyte Specific Reagent (ASR) Vulvar dermatoses (LS, LP, LSC) • Other testing situations – Vulvar intraepithelial neoplasia (VIN) Suspect trich but NaCl slide neg culture or newer assays – Psychogenic Physiologic, psychogenic Pap with trich confirm if low risk • Consider retesting 3 months after treatment Trichomoniasis: Laboratory Tests CDC 2010: Vaginal Trichomoniasis Treatment Test Sensitivity Specificity Cost Comment Aptima TMA +4 (98%) +3 (98%) $$$ NAAT (like GC/Ct) • Recommended regimen Culture +3 (83%) +4 (100%) $$$ Not in most labs – Metronidazole 2 grams PO single dose Point of care – Tinidazole 2 grams PO single dose •Affirm VP III +3 +4 $$$ DNA probe • Alternative regimen (preferred for HIV infected -

Localised Provoked Vestibulodynia (Vulvodynia): Assessment and Management
FOCUS Localised provoked vestibulodynia (vulvodynia): assessment and management Helen Henzell, Karen Berzins Background hronic vulvar pain (pain lasting more than 3–6 months, but often years) is common. It is estimated to affect 4–8% of Vulvodynia is a chronic vulvar pain condition. Localised C women at any one time and 10–20% in their lifetime.1–3 provoked vestibulodynia (LPV) is the most common subset Little attention has been paid to the teaching of this condition of vulvodynia, the hallmark symptom being pain on vaginal so medical practitioners may not recognise the symptoms, and penetration. Young women are predominantly affected. LPV diagnosis is often delayed.2 Community awareness is low, but is a hidden condition that often results in distress and shame, increasing with media attention. Women can be confused by the is frequently unrecognised, and women usually see a number symptoms and not know how to discuss vulvar pain. The onus is of health professionals before being diagnosed, which adds to on medical practitioners to enquire about vulvar pain, particularly their distress and confusion. pain with sex, when taking a sexual or reproductive health history. Objective Vulvodynia The aim of this article is to inform health providers about the Vulvodynia is defined by the International Society for the Study assessment and management of LPV. of Vulvovaginal Disease (ISSVD) as ‘chronic vulvar discomfort, most often described as burning pain, occurring in the absence Discussion of relevant findings or a specific, clinically identifiable, neurologic 4 Diagnosis is based on history. Examination is used to support disorder’. It is diagnosed when other causes of vulvar pain have the diagnosis. -
Effect of Educational Program on Vulvitis Prevention Among Nursing Students
American Journal of Nursing Science 2018; 7(6): 254-267 http://www.sciencepublishinggroup.com/j/ajns doi: 10.11648/j.ajns.20180706.19 ISSN: 2328-5745 (Print); ISSN: 2328-5753 (Online) Effect of Educational Program on Vulvitis Prevention Among Nursing Students Somaya Ouda Abd EL-Menim 1, Huda Abdalla Moursi 2, Ahlam Elahmady Mohamed Sarhan 2 1Obstetric and Woman Health Nursing, Faculty of Nursing, Benha University, Benha, Egypt 2Community Health Nursing, Benha University, Benha, Egypt Email address: To cite this article: Somaya Ouda Abd EL-Menim, Huda Abdalla Moursi, Ahlam Elahmady Mohamed Sarhan. Effect of Educational Program on Vulvitis Prevention among Nursing Students. American Journal of Nursing Science . Vol. 7, No. 6, 2018, pp. 254-267. doi: 10.11648/j.ajns.20180706.19 Received : November 7, 2018; Accepted : November 23, 2018; Published : January 2, 2019 Abstract: The aim of this study was to evaluate the effect of educational program on vulvitis prevention among nursing students Research design: A quasi-experimental design was utilized. Setting: This study was conducted at Faculty of Nursing, Benha University. Sample: convenient sample included two hundred and fifty nursing students female all enrolled in first academic years. Tools of data collection1) a structured interviewing sheet to collect data about socio-demographic characteristics, menstrual and gynecological history and knowledge of nursing students regarding vulvitis 2) reported practices assessment 3) modified likert scale for students' attitude regarding vulvitis. Results: there were general improvements regarding students' knowledge, attitude and practice regarding prevention of vulvitis with highly significant (P ≤ 0.001) difference after educational Program. The mother was the main sources of knowledge to students (60%). -

Female Genital Tuberculosis: a Clinicopathological Study
International Journal of Reproduction, Contraception, Obstetrics and Gynecology Desai RM et al. Int J Reprod Contracept Obstet Gynecol. 2016 Aug;5(8):2780-2783 www.ijrcog.org pISSN 2320-1770 | eISSN 2320-1789 DOI: http://dx.doi.org/10.18203/2320-1770.ijrcog20162665 Research Article Female genital tuberculosis: a clinicopathological study Rathnamala M. Desai*, Sunil Kumar, Usha Brindini Department of Obstetrics and Gynaecology, Sri Dharmasthala Manjunatheshwara College of Medical Sciences and Hospital, Dharwad, Karnataka, India Received: 21 June 2016 Accepted: 09 July 2016 *Correspondence: Dr. Rathnamala M. Desai, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: The aim of this study was to describe the various clinical presentations of female genital tuberculosis and study the different methods of diagnosis and treatment. Methods: A study of all cases of female genital tuberculosis diagnosed in the last five years was done. Results: Female genital tuberculosis was diagnosed in 25 cases over a period of five years. Majority of the women (60%) were in the younger age group. Most of the women (60%) presented with infertility. Twelve (48%) women had primary infertility and 3 (12%) had secondary infertility. Nine (36%) women had secondary amenorrhea. Five (20%) women complained of abdominal pain. Thirteen (52%) women who underwent diagnostic hysterolaparoscopy as a part of evaluation for infertility were diagnosed to have genital tuberculosis. -

An Overview of Vulvovaginal Atrophy‑Related Sexual Dysfunction in Postmenopausal Women
Review Article An Overview of Vulvovaginal Atrophy‑Related Sexual Dysfunction in Postmenopausal Women Tochukwu Christopher Okeke, Cyril Chukwuma Tochukwu Ezenyeaku1, Lawrence Chigbata Ikeako1, Polycarp Uchenna Agu Department of Obstetrics and Gynaecology, University of Nigeria Teaching Hospital (UNTH), Enugu, 1Anambra State University Teaching Hospital, Awka, Nigeria ABSTRACT Menopause and the climacteric period are associated with adverse risk factors for the development of vulvovaginal atrophy‑ related sexual dysfunction. Sexual dysfunction is a common problem in postmenopausal women, often underdiagnosed, inadequately treated, frequently overlooked, and most often impairing the quality of life of these women. To provide clinicians with current information on vulvovaginal atrophy‑related sexual dysfunction in postmenopausal women. This study is a literature review on vulvovaginal atrophy‑related sexual dysfunction in postmenopausal women. Relevant publications were identified through a search of PubMed and Medline, selected references, journals, and textbooks on this topic, and were included in the review. The prevalence of female sexual dysfunction increases with age. It is a common multidimensional problem for postmenopausal women that alter the physiological, biochemical, psychological, and sociocultural environment of a woman. Menopause‑related sexual dysfunction may not be reversible without therapy. Estrogen therapy is the most effective option and is the current standard of care for vulvovaginal atrophy‑related sexual dysfunction in postmenopausal women. Sexual dysfunction is a common multidimensional problem for postmenopausal women and often impairs the quality of life of these women. Estrogen preparations are the most effective treatment. Selective estrogen receptor modulators, vaginal dehydroepiandrostenedione, vaginal testosterone, and tissue‑selective estrogen complexes are promising therapies, but further studies are required to confirm their role, efficacy, and safety. -

The Older Woman with Vulvar Itching and Burning Disclosures Old Adage
Disclosures The Older Woman with Vulvar Mark Spitzer, MD Itching and Burning Merck: Advisory Board, Speakers Bureau Mark Spitzer, MD QiagenQiagen:: Speakers Bureau Medical Director SABK: Stock ownership Center for Colposcopy Elsevier: Book Editor Lake Success, NY Old Adage Does this story sound familiar? A 62 year old woman complaining of vulvovaginal itching and without a discharge self treatstreats with OTC miconazole.miconazole. If the only tool in your tool Two weeks later the itching has improved slightly but now chest is a hammer, pretty she is burning. She sees her doctor who records in the chart that she is soon everyyggthing begins to complaining of itching/burning and tells her that she has a look like a nail. yeast infection and gives her teraconazole cream. The cream is cooling while she is using it but the burning persists If the only diagnoses you are aware of She calls her doctor but speaks only to the receptionist. She that cause vulvar symptoms are Candida, tells the receptionist that her yeast infection is not better yet. The doctor (who is busy), never gets on the phone but Trichomonas, BV and atrophy those are instructs the receptionist to call in another prescription for teraconazole but also for thrthreeee doses of oral fluconazole the only diagnoses you will make. and to tell the patient that it is a tough infection. A month later the patient is still not feeling well. She is using cold compresses on her vulva to help her sleep at night. She makes an appointment. The doctor tests for BV. -

Diagnosing and Managing Vulvar Disease
Diagnosing and Managing Vulvar Disease John J. Willems, M.D. FRCSC, FACOG Chairman, Department of Obstetrics & Gynecology Scripps Clinic La Jolla, California Objectives: IdentifyIdentify thethe majormajor formsforms ofof vulvarvulvar pathologypathology DescribeDescribe thethe appropriateappropriate setupsetup forfor vulvarvulvar biopsybiopsy DescribeDescribe thethe mostmost appropriateappropriate managementmanagement forfor commonlycommonly seenseen vulvarvulvar conditionsconditions Faculty Disclosure Unlabeled Product Company Nature of Affiliation Usage Warner Chilcott Speakers Bureau None ClassificationClassification ofof VulvarVulvar DiseaseDisease byby ClinicalClinical CharacteristicCharacteristic • Red lesions • White lesions • Dark lesions •Ulcers • Small tumors • Large tumors RedRed LesionsLesions • Candida •Tinea • Reactive vulvitis • Seborrheic dermatitis • Psoriasis • Vulvar vestibulitis • Paget’s disease Candidal vulvitis Superficial grayish-white film is often present Thick film of candida gives pseudo-ulcerative appearance. Acute vulvitis from coital trauma Contact irritation from synthetic fabrics Nomenclature SubtypesSubtypes ofof VulvodyniaVulvodynia:: VulvarVulvar VestibulitisVestibulitis SyndromeSyndrome (VVS)(VVS) alsoalso knownknown asas:: • Vestibulodynia • localized vulvar dysesthesia DysestheticDysesthetic VulvodyniaVulvodynia alsoalso knownknown asas:: • “essential” vulvodynia • generalized vulvar dysesthesia Dysesthesia Unpleasant,Unpleasant, abnormalabnormal sensationsensation examplesexamples include:include: -

Comparative Study of Tubal Patency by Hysterosalpingography, Transvaginal Sonosalpingography and Laparoscopy
J. Anuradha, K. Aruna Kumari, A. Sujatha. Comparative study of tubal patency by hysterosalpingography, transvaginal sonosalpingography and laparoscopy. IAIM, 2016; 3(9): 126-133. Original Research Article Comparative study of tubal patency by hysterosalpingography, transvaginal sonosalpingography and laparoscopy J. Anuradha1*, K. ArunaKumari1, A. Sujatha1 1Assistant Professor, Department of Obstetrics and Gynaecology, Modern Government Maternity Hospital, Osmania Medical College, Hyderabad, India *Corresponding author email: [email protected] International Archives of Integrated Medicine, Vol. 3, Issue 9, September, 2016. Copy right © 2016, IAIM, All Rights Reserved. Available online at http://iaimjournal.com/ ISSN: 2394-0026 (P) ISSN: 2394-0034 (O) Received on: 20-08-2016 Accepted on: 30-08-2016 Source of support: Nil Conflict of interest: None declared. How to cite this article: J. Anuradha, K. Arunakumari, A. Sujatha. Comparative study of tubal patency by hysterosalpingography, transvaginal sonosalpingography and laparoscopy. IAIM, 2016; 3(9): 126-133. Abstract Background: Infertility is a global issue in reproductive health. In many cultures the ability to have children is important sign of an individual's worth. Aim and objective: To compare hysterosalpingography, transvaginal sonosalpingography and laparoscopic chromotubation for evaluation of tubal factor in infertility. Materials and methods: This consisted of 50 infertile women with either primary or secondary infertility. Including investigations for other factors, tubal factor was evaluated by hysterosalpingography, transvaginal sonosalpingography and laparoscopic chromotubation (in one or two cycles). Results: The results of 50 cases of Infertility for Tubal patency by sonosalpingography, HSG, laparoscopy. 36 cases were of primary infertility and 14 cases of secondary infertility. Mean duration of primary and secondary infertility were 5.79 ± 3.19 and 5.97 ± 3.36 years respectively. -
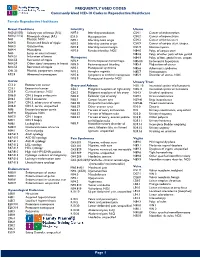
Commonly Used ICD-10 Codes in Reproductive Healthcare
FREQUENTLY USED CODES Commonly Used ICD-10 Codes in Reproductive Healthcare Female Reproductive Healthcare Breast Conditions Infertility Uterus N60.(01/02) Solitary cyst of breast (R/L) N97.0 Infertility-anovulation C54.1 Cancer of endometrium N60.(11/12) Fibrocystic change (R/L) E23.0 Hypopituarism C54.2 Cancer of myometrium N61 Mastitis, NOS N97.1 Infertility-tubal origin C54.3 Cancer of fundus uteri N64.0 Fissure and fistula of nipple N97.2 Infertility-uterine origin C54.9 Cancer of corpus uteri, unspec. N64.3 Galactorrhea N97.8 Infertility-cervical origin D25.9 Uterine myoma N64.4 Mastodynia N97.9 Female infertility, NOS N84.0 Polyp of corpus uteri N63 Lump or mass in breast N84.8 Polyp of other parts of fem genital N64.51 Induration of breast Menopause N84.9 Polyptract of fem. genital tract, unspec. N64.53 Retraction of nipple N92.4 Perimenopausal menorrhagia N85.00 Endometrial hyperplasia N64.59 Other signs/ symptoms in breast N95.0 Postmenopausal bleeding N85.4 Malposition of uterus N64.53 Retraction of nipple N95.1 Menopausal syndrome N85.6 Asherman’s syndrome O91.23 Mastitis, postpartum, unspec. N95.2 Atrophic vaginitis N85.7 Hematometra R92.8 Abnormal mammogram N95.8 Symptoms w artificial menopause N85.9 Disorder of uterus, NOS N95.9 Menopausal disorder NOS Cervix Urinary Tract C53.0 Endocervical cancer Ovary and Adnexa N30. 10 Interstitial cystitis w/o hematuria C53.1 Exocervical cancer C56.1 Malignant neoplasm of right ovary N30.11 Interstitial cystitis w/ hematuria C53.9 Cervical cancer, NOS C56.2 Malignant neoplasm of left -

A Retrospective Study of the Management of Vulvodynia
www.kjurology.org http://dx.doi.org/10.4111/kju.2013.54.1.48 Sexual Dysfunction A Retrospective Study of the Management of Vulvodynia Yongseok Jeon, Youngjun Kim, Bosun Shim, Hana Yoon, Youngyo Park, Bongsuk Shim, Woosik Jeong, Donghyun Lee Department of Urology, Ewha Womans University School of Medicine, Seoul, Korea Purpose: Vulvodynia is characterized by chronic vulvar pain caused by sexual inter- Article History: course and often results in female sexual dysfunction. Because the causes of vulvodynia received 11 June, 2012 10 September, 2012 are not clear, many patients do not receive optimal treatment. Recently, gabapentin accepted and botulinum toxin A have both been shown to be effective treatments for vulvodynia. In this study, we retrospectively analyzed the clinical outcomes of botulinum toxin A and gabapentin treatment for chronic pain in women with this condition. Materials and Methods: Seventy-three women with vulvar pain were administered ei- ther gabapentin (n=62) or botulinum toxin A (n=11) injections. Effectiveness was meas- ured by use of a visual analogue scale (VAS). We analyzed the treatment method, treat- ment duration, success of treatment, and side effects or adverse reactions. Results: Pain levels in both groups significantly decreased after treatment. In the gaba- pentin group, the VAS score decreased from 8.6 before treatment to 3.2 after treatment (p<0.001). The VAS score in the botulinum toxin A group was reduced from 8.1 to 2.5 (p<0.001). Side effects for both therapies were few and subsided with treatment with general antibiotics and nonsteroidal antiinflammatory drugs. Conclusions: Gabapentin and botulinum toxin A are safe and effective treatments for vulvodynia. -

What's Going on Down There?
What’s Going on Down There? Denise Rizzolo, PhD, PA-C Introduction • Vulvovaginitis is inflammation of the vulva and vaginal tissues. • Characterized by vaginal discharge and/or vulvar itching and irritation as well as possible vaginal odor. • Accounts for 10 million visits yearly in the US and is the most common gynecologic complaint in prepubertal girls. History- What should you ask? • Pruritus -General or just one spot • Soreness: stinging / burning / pain • Difficulty with sex • Lumps • Discharge • Partner’s have any symptoms • History of similar symptoms Physical Examination • Careful gynecologic exam • Inspection of discharge • Close examination of vulvovaginal area • Careful inspection of cervix • Look at perineum as well Physiologic Discharge • Responsible for 10 percent of cases of vaginal discharge. • Composed of vaginal squamous cells suspended in fluid medium. • Clinical characteristics: • clear to slightly cloudy • non-homogeneous • highly viscous • Changes throughout the month Normal Vaginal Discharge • Not associated with: • itching • burning • malodor • Normal increase in volume • ovulation • following coitus • after menses • during pregnancy The Big 3 •Three most common causes of vulvovaginitis include: • Bacterial Vaginosis • Vaginal candidiasis • Trichomonas Vaginalis •Others include: atrophic vaginitis, irritant vaginitis, and other STIs. Vaginal Candidiasis- Overview • Less common in postmenopausal women, unless taking estrogen. • 90% of yeast infections are secondary to Candida Albican (Most common). • Risk Factors