Antibiotic Resistance: Mechanisms and New Antimicrobial Approaches
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mechanisms and Strategies to Overcome Multiple Drug Resistance in Cancer
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector FEBS Letters 580 (2006) 2903–2909 Minireview Mechanisms and strategies to overcome multiple drug resistance in cancer Tomris Ozben* Akdeniz University, Faculty of Medicine, Department of Biochemistry, 07070 Antalya, Turkey Received 30 January 2006; accepted 9 February 2006 Available online 17 February 2006 Edited by Horst Feldmann The cytotoxic drugs that are most frequently associated with Abstract One of the major problems in chemotherapy is multi- drug resistance (MDR) against anticancer drugs. ATP-binding MDR are hydrophobic, amphipathic natural products, such as cassette (ABC) transporters are a family of proteins that medi- the taxanes (paclitaxel and docetaxel), vinca alkaloids (vinorel- ate MDR via ATP-dependent drug efflux pumps. Many MDR bine, vincristine, and vinblastine), anthracyclines (doxorubicin, inhibitors have been identified, but none of them have been pro- daunorubicin, and epirubicin), epipodophyllotoxins (etoposide ven clinically useful without side effects. Efforts continue to dis- and teniposide), antimetabolites (methorexate, fluorouracil, cover not toxic MDR inhibitors which lack pharmacokinetic cytosar, 5-azacytosine, 6-mercaptopurine, and gemcitabine) interactions with anticancer drugs. Novel approaches have also topotecan, dactinomycin, and mitomycin C [4,6–8]. been designed to inhibit or circumvent MDR. In this review, Overexpression of ATP-binding cassette (ABC) transporters the structure and function of ABC transporters and development has been shown to be responsible for MDR [5]. Therefore eluci- of MDR inhibitors are described briefly including various ap- dation of the structure and function for each ABC transporter is proaches to suppress MDR mechanisms. -

A Review on Antimicrobial Resistance in Developing Countries
mac har olo P gy : & O y r p t e s i n Biochemistry & Pharmacology: Open A m c e c h e c Ravalli, et al. Biochem Pharmacol 2015, 4:2 s o i s B Access DOI: 10.4172/2167-0501.1000r001 ISSN: 2167-0501 Review Open Access A Review on Antimicrobial Resistance in Developing Countries Ravalli R1*, NavaJyothi CH2, Sushma B3 and Amala Reddy J4 1Deparment of Pharmaceutical Sciences, Andhra University, Vishakapatnam, India 2University College of Technology, Osmania University, Hyderabad, India 3Deparment of Medicinal Chemistry, National Institute of Pharmaceutical Education and Research (NIPER) Hyderabad, India 4Deparment of Pharmaceutical Sciences, Osmania University, Hyderabad, India *Corresponding author: Ravalli R, Deparment of Pharmaceutical Sciences, Andhra University, Vishakapatnam, India, Tel: + 0437-869-033; E-mail: [email protected] Received date: April 13, 2015; Accepted date: April 14, 2015; Published date: April 21, 2015 Copyright: © 2015 Ravalli Remella. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestri cted use, distribution, and reproduction in any medium, provided the original author and source are credited. Availability of Antimicrobial Drugs isolates were proof against Principen, Co-trimoxazole, and bactericide, and 14-40% were given with Mecillinam [6]. This was associate degree Although foremost potent and recently developed antimicrobial outsized increase over the half resistant isolates notable in 1991, before medicine are offered throughout the globe, in developing countries the drug was wide on the market. Throughout infectious disease their use is confined to people who are flush enough to afford them. In epidemics the organism has the flexibleness to develop increasing tertiary referral hospitals like the Kenyatta National Hospital in resistance, typically by acquisition of plasmids. -

Expression of Cytokeratin Confers Multiple Drug Resistance (Multidrug Resance/Cytoskeleton) PATRICIA A
Proc. Nati. Acad. Sci. USA Vol. 91, pp. 5311-5314, June 1994 Pharmacology Expression of cytokeratin confers multiple drug resistance (multidrug resance/cytoskeleton) PATRICIA A. BAUMAN*, WILLIAM S. DALTON*t, JOHN M. ANDERSONt, AND ANNE E. CRESSO§ Departments of *Pharmacology and Toxicology, tMedicine, and *Radiation Oncology, The University of Arizona, The Arizona Cancer Center, Tucson, AZ 85724 Communicated by Gertrude B. Elion, February 23, 1994 (received for review October 21, 1993) ABSTRACT The cytokeratin network is an extensive fda- We utilized a mouse fibroblast cell line and a transfected mentous structure in the cytoplasm whose biological function(s) variant expressing cytokeratins 8 and 18 (9) to test whether is unknown. Based upon previous data showing the modifica- cytokeratin expression could alter the cell survival response tion ofcytokeratin by mitoxantrone, we investigated the ability to six different chemotherapeutic drugs. of cytokeratin networks to influence the survival response of cells to chemotherapeutic agents. We have compared the MATERIALS AND METHODS survival of mouse L fibroblasts lacking cytokeratins with that of L cells transfected with cytokeratins 8 and 18 in the presence Tumor Cell Lines, Growth Curves, and Cell Cycle Distri- of chemotherapeutic drugs. The expression of cytokeratins 8 butions. Parental L cells and transfected LK8+18 cells were and 18 conferred a multiple drug resistance phenotype on cells obtained from Robert Oshima (La Jolla Cancer Research exposed to mitoxantrone, doxorubicin, methotrexate, melpha- Foundation, La Jolla, CA) and maintained as described (9). Ian, Colcemid, and vincristine. The degree of drug resistance Mock transfectants (LPBMOC) were created by simultane- was 5-454 times that of parental cells, depending upon the ous calcium phosphate transfection of pGEM-3 (Promega) agent used. -
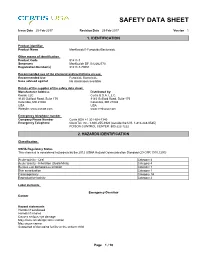
Mankocide® Fungicide/Bactericide
SAFETY DATA SHEET Issue Date 25-Feb-2017 Revision Date 25-Feb-2017 Version 1 1. IDENTIFICATION Product identifier Product Name ManKocide® Fungicide/Bactericide Other means of identification Product Code 91411-7 Synonyms ManKocide DF, B12262770 Registration Number(s) 91411-7-70051 Recommended use of the chemical and restrictions on use Recommended Use Fungicide Bactericide Uses advised against No information available Details of the supplier of the safety data sheet Manufacturer Address Distributed by: Kocide LLC Certis U.S.A. L.L.C. 9145 Guilford Road, Suite 175 9145 Guilford Road, Suite 175 Columbia, MD 21046 Columbia, MD 21046 USA USA Website: www.kocide.com www.certisusa.com Emergency telephone number Company Phone Number Certis USA +1 301-604-7340 Emergency Telephone ChemTel, Inc.: 1-800-255-3924 (outside the U.S. 1-813-248-0585) POISON CONTROL CENTER: 800-222-1222 2. HAZARDS IDENTIFICATION Classification OSHA Regulatory Status This chemical is considered hazardous by the 2012 OSHA Hazard Communication Standard (29 CFR 1910.1200) Acute toxicity - Oral Category 4 Acute toxicity - Inhalation (Dusts/Mists) Category 4 Serious eye damage/eye irritation Category 1 Skin sensitization Category 1 Carcinogenicity Category 1A Reproductive toxicity Category 2 Label elements Emergency Overview Danger Hazard statements Harmful if swallowed Harmful if inhaled Causes serious eye damage May cause an allergic skin reaction May cause cancer Suspected of damaging fertility or the unborn child _____________________________________________________________________________________________ -

Association of Genetic and Nongenetic Variabilities With
ASSOCIATION OF GENETIC AND NONGENETIC VARIABILITIES WITH PHENYTOIN AND CARBAMAZEPINE RESPONSE PHENOTYPES A DISSERTATION SUBMITTED TO THE FACULTY OF THE GRADUATE SCHOOL OF THE UNIVERSITY OF MINNESOTA BY PORNPIMOL KIJSANAYOTIN IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY RICHARD BRUNDAGE ADVISOR APRIL, 2012 © Pornpimol Kisanayotin 2012 Acknowledgements It has been a long time since I decided to pursue the PhD study in the US after receiving a scholarship from the Royal Thai Government. Without the following people I could not be able to follow my dream to successfully conduct this pharmacogenetic study for my PhD dissertation. First, I would like to express my deep gratitude to Prof. James C Cloyd and Prof. Ilo E Leppik for not only giving me the opportunity to carry out this research work by using data sets from the P50 program projects but also all their academic and financial support. I also would like to express my special gratitude to Prof. Richard Brundage, my advisor, for his kindness, academic advice as well as all his support and encouragement. I express my gratitude to Prof. William S Oetting, my co-advisor for his academic advice and encouraging words. I also express my gratitude to Prof. Richard King for allowing me to use his laboratory, facilities and providing technical support for genotyping work. I would like to thank Dr. Angela K Burnbaum and all the staff at the Epilepsy Reseach and Education Program, University of Minnesota for all their assistance in research. I would like to thank Dr. Elving Anderson for his kindness and academic advice. -

Antibiotic Resistance in Plant-Pathogenic Bacteria
PY56CH08-Sundin ARI 23 May 2018 12:16 Annual Review of Phytopathology Antibiotic Resistance in Plant-Pathogenic Bacteria George W. Sundin1 and Nian Wang2 1Department of Plant, Soil, and Microbial Sciences, Michigan State University, East Lansing, Michigan 48824, USA; email: [email protected] 2Citrus Research and Education Center, Department of Microbiology and Cell Science, Institute of Food and Agricultural Sciences, University of Florida, Lake Alfred, Florida 33850, USA Annu. Rev. Phytopathol. 2018. 56:8.1–8.20 Keywords The Annual Review of Phytopathology is online at kasugamycin, oxytetracycline, streptomycin, resistome phyto.annualreviews.org https://doi.org/10.1146/annurev-phyto-080417- Abstract 045946 Antibiotics have been used for the management of relatively few bacterial Copyright c 2018 by Annual Reviews. plant diseases and are largely restricted to high-value fruit crops because of Access provided by INSEAD on 06/01/18. For personal use only. All rights reserved the expense involved. Antibiotic resistance in plant-pathogenic bacteria has Annu. Rev. Phytopathol. 2018.56. Downloaded from www.annualreviews.org become a problem in pathosystems where these antibiotics have been used for many years. Where the genetic basis for resistance has been examined, antibiotic resistance in plant pathogens has most often evolved through the acquisition of a resistance determinant via horizontal gene transfer. For ex- ample, the strAB streptomycin-resistance genes occur in Erwinia amylovora, Pseudomonas syringae,andXanthomonas campestris, and these genes have pre- sumably been acquired from nonpathogenic epiphytic bacteria colocated on plant hosts under antibiotic selection. We currently lack knowledge of the effect of the microbiome of commensal organisms on the potential of plant pathogens to evolve antibiotic resistance. -

Socioeconomic Factors Associated with Antimicrobial Resistance Of
01 Pan American Journal Original research of Public Health 02 03 04 05 06 Socioeconomic factors associated with antimicrobial 07 08 resistance of Pseudomonas aeruginosa, 09 10 Staphylococcus aureus, and Escherichia coli in Chilean 11 12 hospitals (2008–2017) 13 14 15 Kasim Allel,1 Patricia García,2 Jaime Labarca,3 José M. Munita,4 Magdalena Rendic,5 Grupo 16 6 5 17 Colaborativo de Resistencia Bacteriana, and Eduardo A. Undurraga 18 19 20 21 Suggested citation Allel K, García P, Labarca J, Munita JM, Rendic M; Grupo Colaborativo de Resistencia Bacteriana; et al. Socioeconomic fac- 22 tors associated with antimicrobial resistance of Pseudomonas aeruginosa, Staphylococcus aureus, and Escherichia coli in 23 Chilean hospitals (2008–2017). Rev Panam Salud Publica. 2020;44:e30. https://doi.org/10.26633/RPSP.2020.30 24 25 26 27 ABSTRACT Objective. To identify socioeconomic factors associated with antimicrobial resistance of Pseudomonas aeru- 28 ginosa, Staphylococcus aureus, and Escherichia coli in Chilean hospitals (2008–2017). 29 Methods. We reviewed the scientific literature on socioeconomic factors associated with the emergence and 30 dissemination of antimicrobial resistance. Using multivariate regression, we tested findings from the literature drawing from a longitudinal dataset on antimicrobial resistance from 41 major private and public hospitals and 31 a nationally representative household survey in Chile (2008–2017). We estimated resistance rates for three pri- 32 ority antibiotic–bacterium pairs, as defined by the Organisation for Economic Co-operation and Development; 33 i.e., imipenem and meropenem resistant P. aeruginosa, cloxacillin resistant S. aureus, and cefotaxime and 34 ciprofloxacin resistant E. coli. 35 Results. -

The Use of Bactericides in Plant Agriculture with Reference to Use in Ci
The Use of Bactericides in Plant Agriculture with Reference to Use in Ci... http://citrusrdf.org/use_of_bactericides_in_plant_ag_2016-02-04#more-4047 … Stephanie L. Slinski, Ph.D., Bactericide Project Manager, CRDF February 2016 The purpose of this communication is to discuss the use of bactericides in plant agriculture to control disease epidemics and the approaches that have been tested to control Huanglongbing (HLB) in citrus trees. The Citrus Research and Development Foundation (CRDF) has made this topic a priority in responding to HLB in Florida citrus. HLB is a disease devastating the citrus industry in Florida and throughout the world. Presently, no chemical treatment or resistant plant is available that will control the disease. For the Florida citrus industry to survive this epidemic, a chemical control will be necessary to suppress the disease, keeping the trees in production until groves can be replanted with resistant or tolerant varieties. This is similar to approaches taken during plant disease epidemics in other crops, which were eventually controlled by the planting of resistant varieties. Oxytetracycline, streptomycin sulfate and copper have been the main chemicals available to treat bacterial plant diseases in the US. The use of copper is limited to foliar diseases in regions where copper resistance is not widespread. Streptomycin and oxytetracycline are routinely used on some crops when copper is inadequate. Oxytetracycline has also often been used in the past to help manage plant disease epidemics. Research using bactericides on citrus suggests that chemical control may improve citrus tree health and contribute to sustaining the citrus industry in the current epidemic. Introduction The disease HLB has been known in many regions of the world for over a century. -

Multiple Drug Resistance: a Fast-Growing Threat
Review Article ISSN: 2574 -1241 DOI: 10.26717/BJSTR.2019.21.003572 Multiple Drug Resistance: A Fast-Growing Threat Eremwanarue Aibuedefe Osagie1,2* and Shittu Hakeem Olalekan1 1Department of Plant Biology and Biotechnology, University of Benin, Nigeria 2Lahor Research Laboratories and Diagnostics Centre, Nigeria *Corresponding author: Eremwanarue Aibuedefe Osagie, Department of Plant Biology and Biotechnology, University of Benin, Nigeria ARTICLE INFO Abstract Received: September 03, 2019 The spread of antibiotic resistant bacteria is a growing problem and a public health Published: September 10, 2019 issue. Over the years, various genetic mechanisms concerned with antibiotic resistance have been identified to be natural and acquired resistance. The natural resistance Citation: Eremwanarue Aibuedefe Osag- ie, Shittu Hakeem Olalekan. Multiple Geneticinvolved Elements mutation [MGEs] via target such modification,as plasmid, transposon reduced permeability, and integrons efflux genetic system elements and Drug Resistance: A Fast-Growing Threat. on the other hand, acquired resistance via horizontal gene tranfer include Moblie Biomed J Sci & Tech Res 21(2)-2019. Integrons are widely distributed, especially in Gram-negative bacteria; they are carried BJSTR. MS.ID.003572. bythat Mobile can acquire, Genetic exchange, Elements and such express as plasmids, genes embeddedand transposons, within whichGene Cassettespromote [GC].their spread within bacterial communities and have been studied mainly in the clinical setting Keywords: Antibiotics; Multiple Drug for their involvement in antibiotic resistance, their role in the environment is now an Resistant Bacteria; Mobile Genetic increasing focus of attention. The aim of this review is to educate the populise about Element; Integrons Plasmid the mechanisms of multiple drug resistance bacteria isolates and the danger ahead if appropriate regulations are not put in place especially in developing country like Nigeria. -

Evaluation of Several Bactericides As Seed Treatments for the Control of Black Rot of Crucifers and Studies on an Antibacterial Substance from Cauliflower Seed
Louisiana State University LSU Digital Commons LSU Historical Dissertations and Theses Graduate School 1962 Evaluation of Several Bactericides as Seed Treatments for the Control of Black Rot of Crucifers and Studies on an Antibacterial Substance From Cauliflower Seed. (Parts I and II). Fereydoon Malekzadeh Louisiana State University and Agricultural & Mechanical College Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_disstheses Recommended Citation Malekzadeh, Fereydoon, "Evaluation of Several Bactericides as Seed Treatments for the Control of Black Rot of Crucifers and Studies on an Antibacterial Substance From Cauliflower Seed. (Parts I and II)." (1962). LSU Historical Dissertations and Theses. 787. https://digitalcommons.lsu.edu/gradschool_disstheses/787 This Dissertation is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Historical Dissertations and Theses by an authorized administrator of LSU Digital Commons. For more information, please contact [email protected]. This dissertation has been 63—2781 microfilmed exactly as received MALEKZADEH, Fereydoon, 1933- EVALUATION OF SEVERAL BACTERICIDES AS SEED TREATMENTS FOR THE CONTROL OF BLACK ROT OF CRUCIFERS AND STUDIES ON AN ANTIBACTERIAL SUBSTANCE FROM CAULI FLOWER SEED. (PARTS I AND II). Louisiana State University, Ph.D.,1962 Agriculture, plant pathology University Microfilms, Inc., Ann Arbor, Michigan EVALUATION OF SEVERAL BACTERICIDES AS SEED TREATMENTS FOR THE CONTROL OF BLACK ROT OF CRUCIFERS AND STUDIES ON AN ANTIBACTERIAL SUBSTANCE FROM CAULIFLOWER SEED A Dissertation Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College in partial fulfillment of the requirements for the degree of Doctor of Philosophy in The Department of Botany and Plant Pathology by Fereydoon Malekzadeh B.Sc., University of Teheran, 1956 M .Sc., University of Teheran, 1958 August, 1962 ACKNOWLEDGMENT The writer wishes to express his sincere appreciation and gratitude to Dr. -

Resistance to Cancer Chemotherapy
Alfarouk et al. Cancer Cell Int (2015) 15:71 DOI 10.1186/s12935-015-0221-1 REVIEW Open Access Resistance to cancer chemotherapy: failure in drug response from ADME to P‑gp Khalid O Alfarouk1*, Christian‑Martin Stock2, Sophie Taylor3, Megan Walsh3, Abdel Khalig Muddathir4, Daniel Verduzco5, Adil H H Bashir1, Osama Y Mohammed6, Gamal O Elhassan7,8, Salvador Harguindey9, Stephan J Reshkin10, Muntaser E Ibrahim1 and Cyril Rauch3 Abstract Cancer chemotherapy resistance (MDR) is the innate and/or acquired ability of cancer cells to evade the effects of chemotherapeutics and is one of the most pressing major dilemmas in cancer therapy. Chemotherapy resistance can arise due to several host or tumor-related factors. However, most current research is focused on tumor-specific factors and specifically genes that handle expression of pumps that efflux accumulated drugs inside malignantly transformed types of cells. In this work, we suggest a wider and alternative perspective that sets the stage for a future platform in modifying drug resistance with respect to the treatment of cancer. Keywords: Drug, Resistance, Pharmacokinetics, ADME, pH, MDR Background Macroscopic (systemic) resistance [host–related In US only, the newly diagnosed cancer patient is factors] 1,665,540 every year and the estimated death is 585,720 One of the major effects of host-related factors that [1] which are increasing as countries become more devel- determine the activity of the drug is pharmacokinetic. oped and more people reach advanced ages. Therefore, Pharmacokinetics is defined as the action of the body in many efforts are being done in the war against cancer [2]. -
Inventory of Projects
INVENTORY OF PROJECTS PROGRESS REPORT: IMPLEMENTATION OF A PUBLIC HEALTH ACTION PLAN TO COMBAT ANTIMICROBIAL RESISTANCE PROGRESS THROUGH 2007 FOCUS AREA I: SURVEILLANCE ACTION ITEM #1: DETERMINE WHICH ORGANISMS AND SUSCEPTIBILITY TO SPECIFIC ANTIMICROBIAL DRUGS SHOULD BE UNDER SURVEILLANCE AND CREATE A MECHANISM FOR PERIODIC UPDATING OF THIS LIST. PROJECT TITLE: PUBLIC HEALTH SURVEILLANCE • Agency: CDC, USDA, FDA, DoD, VA • Description: Organisms currently under public health surveillance for antimicrobial resistance include: Campylobacter, E. coli O157:H7, Gram negative and Gram positive organisms causing health care associated infections, group A Streptococcus, group B Streptococcus, Haemophilus influenzae, Helicobacter pylori, HIV, Influenza, Malaria, Mycobacterium tuberculosis, Neisseria gonorrhoeae, Neisseria meningitidis, Salmonella, Shigella, Staphylococcus aureus, Streptococcus pneumoniae, Streptococcus pyogenes, Trichomonas vaginalis, and Vancomycin Resistant Enterococcus. Organisms are added to this list when resistance emerges as a public health problem, as tools are developed for detecting resistance, and when there is capacity at the appropriate level. On August 30, 2006, FDA cleared a new test for the detection of vancomycin resistant Enterococci (VRE) by detecting vanA and vanB genes using an automated real-time PCR Instrument. It is indicated for use for patients at risk for VRE colonization. • Results: Ongoing. See Executive Summary and Surveillance Data (to be released following public comment period, summer 2007). PROJECT: CDC ANTIMICROBIAL RESISTANCE SURVEILLANCE ACTIVITIES MEETING • Agency: CDC • Description: The CDC Office of Antimicrobial Resistance, in response to the recently held Antimicrobial Resistance Task Force consultants meeting, convened an internal AR surveillance meeting to explore ways for programs to strengthen and enhance their current surveillance efforts. By sharing successes and failures and exploring potential collaborations, we may be able to increase the impact and utility of our overall surveillance programs.