022450Orig1s000
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Table S1: Sensitivity, Specificity, PPV, NPV, and F1 Score of NLP Vs. ICD for Identification of Symptoms for (A) Biome Developm
Table S1: Sensitivity, specificity, PPV, NPV, and F1 score of NLP vs. ICD for identification of symptoms for (A) BioMe development cohort; (B) BioMe validation cohort; (C) MIMIC-III; (D) 1 year of notes from patients in BioMe calculated using manual chart review. A) Fatigue Nausea and/or vomiting Anxiety Depression NLP (95% ICD (95% CI) P NLP (95% CI) ICD (95% CI) P NLP (95% CI) ICD (95% CI) P NLP (95% CI) ICD (95% CI) P CI) 0.99 (0.93- 0.59 (0.43- <0.00 0.25 (0.12- <0.00 <0.00 0.54 (0.33- Sensitivity 0.99 (0.9 – 1) 0.98 (0.88 -1) 0.3 (0.15-0.5) 0.85 (0.65-96) 0.02 1) 0.73) 1 0.42) 1 1 0.73) 0.57 (0.29- 0.9 (0.68- Specificity 0.89 (0.4-1) 0.75 (0.19-1) 0.68 0.97 (0.77-1) 0.03 0.98 (0.83-1) 0.22 0.81 (0.53-0.9) 0.96 (0.79-1) 0.06 0.82) 0.99) 0.99 (0.92- 0.86 (0.71- 0.94 (0.79- 0.79 (0.59- PPV 0.96 (0.82-1) 0.3 0.95 (0.66-1) 0.02 0.95 (0.66-1) 0.16 0.93 (0.68-1) 0.12 1) 0.95) 0.99) 0.92) 0.13 (0.03- <0.00 0.49 (0.33- <0.00 0.66 (0.48- NPV 0.89 (0.4-1) 0.007 0.94 (0.63-1) 0.34 (0.2-0.51) 0.97 (0.81-1) 0.86 (0.6-0.95) 0.04 0.35) 1 0.65) 1 0.81) <0.00 <0.00 <0.00 F1 Score 0.99 0.83 0.88 0.57 0.95 0.63 0.82 0.79 0.002 1 1 1 Itching Cramp Pain NLP (95% ICD (95% CI) P NLP (95% CI) ICD (95% CI) P NLP (95% CI) ICD (95% CI) P CI) 0.98 (0.86- 0.24 (0.09- <0.00 0.09 (0.01- <0.00 0.52 (0.37- <0.00 Sensitivity 0.98 (0.85-1) 0.99 (0.93-1) 1) 0.45) 1 0.29) 1 0.66) 1 0.89 (0.72- 0.5 (0.37- Specificity 0.96 (0.8-1) 0.98 (0.86-1) 0.68 0.98 (0.88-1) 0.18 0.5 (0-1) 1 0.98) 0.66) 0.88 (0.69- PPV 0.96 (0.8-1) 0.8 (0.54-1) 0.32 0.8 (0.16-1) 0.22 0.99 (0.93-1) 0.98 (0.87-1) NA* 0.97) 0.98 (0.85- 0.57 (0.41- <0.00 0.58 (0.43- <0.00 NPV 0.98 (0.86-1) 0.5 (0-1) 0.02 (0-0.08) NA* 1) 0.72) 1 0.72) 1 <0.00 <0.00 <0.00 F1 Score 0.97 0.56 0.91 0.28 0.99 0.68 1 1 1 *Denotes 95% confidence intervals and P values that could not be calculated due to insufficient cells in 2x2 tables. -

Pharmaceutical Powder Compressibility – a Science-Based Approach
Pharmaceutical powder compressibility – a science-based approach Inauguraldissertation zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von Nicolaos D.Gentis aus Egrigoros (Chios) Griechenland Oberkulm (AG) Schweiz Basel, 2012 Approval Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät auf Antrag von Prof. Dr. Matthias Hamburger und PD Dr. Gabriele Betz und Prof. Dr. Thierry F. Vandamme Basel, den 21. Februar 2012 Prof. Dr. Martin Spiess Dekan 2 Dedicated to my parents with love, appreciation and respect 3 Σωκράτης ―I know one thing, that I know nothing‖ Socrates c. 469 BC – 399 BC 4 Acknowledgements The work for this PhD thesis was carried out in the Industrial Pharmacy Lab, Department of Pharmaceutical Sciences, University of Basel and at the facility of Natoli Engineering Inc. in Saint Louis, Missouri (USA). I would like to express my appreciation and sincere gratefulness to PD Dr. Gabriele Betz for giving me the opportunity to do a PhD under her excellent supervision with essential, continuous support, guidance and brilliant, positive motivation. I would like to thank Prof. Dr. Matthias Hamburger for accepting to be my Faculty Responsible and for the support. My appreciation goes also to Prof. Dr. Thierry F. Vandamme for accepting to assume the co-referencing of this PhD thesis. At this point I would like to thank all former Industrial Pharmacy Research Group members for the unique support and for the great, crazy working atmosphere in the laboratory. Especially I would like to thank Mr. Branko Z. Vranic for his great collaboration and support in the research work of project 2 in this thesis. -

Drug–Drug Salt Forms of Ciprofloxacin with Diflunisal and Indoprofen
CrystEngComm View Article Online COMMUNICATION View Journal | View Issue Drug–drug salt forms of ciprofloxacin with diflunisal and indoprofen† Cite this: CrystEngComm,2014,16, 7393 Partha Pratim Bag, Soumyajit Ghosh, Hamza Khan, Ramesh Devarapalli * Received 27th March 2014, and C. Malla Reddy Accepted 12th June 2014 DOI: 10.1039/c4ce00631c www.rsc.org/crystengcomm Two salt forms of a fluoroquinolone antibacterial drug, Crystal engineering approach has been effectively ciprofloxacin (CIP), with non-steroidal anti-inflammatory drugs, utilized in recent times in the synthesis of new forms particu- diflunisal (CIP/DIF) and indoprofen (CIP/INDP/H2O), were synthe- larly by exploiting supramolecular synthons. Hence the sized and characterized by PXRD, FTIR, DSC, TGA and HSM. Crystal identification of synthons that can be transferred across Creative Commons Attribution-NonCommercial 3.0 Unported Licence. structure determination allowed us to study the drug–drug different systems is important. For example, synthon trans- interactions and the piperazine-based synthon (protonated ferability in cytosine and lamivudine salts was recently dem- piperazinecarboxylate) in the two forms, which is potentially useful onstrated by Desiraju and co-workers by IR spectroscopy for the crystal engineering of new salt forms of many piperazine- studies.20a Aakeröy and co-workers successfully estab- based drugs. lished the role of synthon transferability (intermolecular amide⋯amide synthons) in the assembly and organization of Multicomponent pharmaceutical forms consisting of an bidentate acetylacetonate (acac) and acetate “paddlewheel” active pharmaceutical ingredient (API) and an inactive 20b complexes of a variety of metal(II)ions. Recently Das et al. co-former,whichisideallyagenerally recognized as safe – have reported the gelation behaviour in various diprimary This article is licensed under a 1 3 (GRAS) substance, have been well explored in recent times. -

A Comparative Efficacy of Propacetamol and Ketorolac in Postoperative Patient Controlled Analgesia
Korean J Pain 2015 July; Vol. 28, No. 3: 203-209 pISSN 2005-9159 eISSN 2093-0569 http://dx.doi.org/10.3344/kjp.2015.28.3.203 | Original Article | A Comparative Efficacy of Propacetamol and Ketorolac in Postoperative Patient Controlled Analgesia Department of Anesthesiology and Pain Medicine, Chonnam National University Medical School, Gwangju, Korea Bong Ha Heo, Ji Hun Park, Jung Il Choi, Woong Mo Kim, Hyoung Gon Lee, Soo Young Cho, and Myoung Ha Yoon Background: Ketorolac has been used as a postoperative analgesia in combination with opioids. However, the use of ketorolac may produce serious side effects in vulnerable patients. Propacetamol is known to induce fewer side effects than ketorolac because it mainly affects the central nervous system. We compared the analgesic effects and patient satisfaction levels of each drug when combined with fentanyl patient-controlled analgesia (PCA). Methods: The patients were divided into two groups, each with n = 46. The patients in each group were given 60 mg of ketorolac or 2 g of propacetamol (mixed with fentanyl) for 10 minutes. The patients were then given 180 mg of ketorolac or 8 g of propacetamol (mixed with fentanyl and ramosetron) through PCA. We assessed the visual analogue pain scale (VAS) at the time point immediately before administration (baseline) and at 15, 30, and 60 minutes, and 24 hours after administration. Also, the side effects of each regimen and each patient’s degree of satisfaction were assessed. Results: There was a significant decline in the VAS score in both groups (P < 0.05). However, there were no significant differences in the VAS scores between the groups at each time point. -
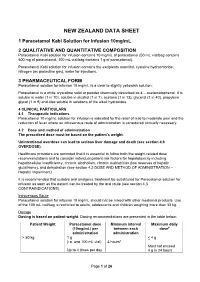
Paracetamol Kabi Data Sheet
NEW ZEALAND DATA SHEET 1 Paracetamol Kabi Solution for Infusion 10mg/mL 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Paracetamol Kabi solution for infusion contains 10 mg/mL of paracetamol (50 mL vial/bag contains 500 mg of paracetamol, 100 mL vial/bag contains 1 g of paracetamol). Paracetamol Kabi solution for infusion contains the excipients mannitol, cysteine hydrochloride, nitrogen (as protective gas), water for injections. 3 PHARMACEUTICAL FORM Paracetamol solution for infusion 10 mg/mL is a clear to slightly yellowish solution. Paracetamol is a white crystalline solid or powder chemically described as 4 – acetamidophenol. It is soluble in water (1 in 70), soluble in alcohol (1 in 7), acetone (1 in 13), glycerol (1 in 40), propylene glycol (1 in 9) and also soluble in solutions of the alkali hydroxides. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Paracetamol 10 mg/mL solution for infusion is indicated for the relief of mild to moderate pain and the reduction of fever where an intravenous route of administration is considered clinically necessary. 4.2 Dose and method of administration The prescribed dose must be based on the patient’s weight. Unintentional overdose can lead to serious liver damage and death (see section 4.9 OVERDOSE). Healthcare providers are reminded that it is essential to follow both the weight-related dose recommendations and to consider individual patient risk factors for hepatotoxicity including hepatocellular insufficiency, chronic alcoholism, chronic malnutrition (low reserves of hepatic glutathione), and dehydration (see section 4.2 DOSE AND METHOD OF ADMINISTRATION – Hepatic Impairment). It is recommended that suitable oral analgesic treatment be substituted for Paracetamol solution for infusion as soon as the patient can be treated by the oral route (see section 4.3 CONTRAINDICATIONS). -

(8) No. 1 March 2005 Alexandria Journal of Anaesthesia and Intensive Care 50
Alexandria Journal of Anaesthesia and Intensive Care 49 Propacetamol Versus Placebo for Management of Acute Postoperative Pain After Elective Tonsillectomy in Children. Mahmoud A Nassef, MD*. Ashraf M Moustafa, MD**. Ashraf A Moussa, MD***. *Department of Anesthesia, Beni-Suef Faculty of Medicine, Cairo University **Department of Anesthesia, Menoufiya University ***Department of Anesthesia,Menoufiya Liver Institute, Menoufiya University ABSTRACT The analgesic efficacy and safety of propacetamol, an injectable prodrug of acetaminophen, was assessed versus placebo after elective tonsillectomy operation in children. Using a double-blind, randomized parallel group design, 70 children aged 6-12 years were included to evaluate the effect of a single iv infusion of 40 mg/kg propacetamol versus a single infusion of 100 ml normal saline ( placebo ) given at the recovery room. Analgesic efficacy was assessed on pain scores rated on a four-points verbal scale, a five-points visual scale ( faces ) and a four-points pain relief verbal scale; before administration ( T0 ) and 0.25, 0.5, 1, 2, 3, 4, 5 and 6 hours after the infusion. The global efficacy was rated on a five-point scale at the end of the study. Rescue medication was allowed freely and the time for re-medication as well as the occurrence of any side effects was recorded. Propacetamol was statistically superior to placebo on all assessment criteria. The global final efficacy evaluation demonstrated 12 patients in the propacetamol group with good and very good scores compared to only one patient in the placebo group. Rescue medication was used in 40% of patients in the propacetamol group versus 83% in the placebo group. -

(12) United States Patent (10) Patent No.: US 9,084,769 B2 Alex Et Al
US009084769B2 (12) United States Patent (10) Patent No.: US 9,084,769 B2 Alex et al. (45) Date of Patent: Jul. 21, 2015 (54) COMPOSITIONS COMPRISING NON (2013.01); A61K31/192 (2013.01); A61 K STEROIDAL ANTI-INFLAMMLATORY DRUGS 31/415 (2013.01); A61 K3I/7016 (2013.01) AND METHODS FOR USE THEREOF (58) Field of Classification Search CPC A61K 2300/00; A61K 31/7016; A61K 33/30 (71) Applicants:Phillip Alex, Abingdon, MD (US); Ben USPC .................................. 424/641, 451, 474, 490 Johns, Scotch Plains, NJ (US) See application file for complete search history. (72) Inventors: Phillip Alex, Abingdon, MD (US); Ben (56) References Cited Johns, Scotch Plains, NJ (US) |U.S. PATENT DOCUMENTS (*) Notice: Subject to any disclaimer, the term of this patent is extended or adjusted under 35 2010/0150861 A1* 6/2010 Geibel et al. ................. 424/85.2 U.S.C. 154(b) by 0 days. OTHER PUBLICATIONS (21) Appl. No.: 13/705,552 Watanabe et al. Prebiotic Properties of Epilactose. Aug. 5, 2008. J. Dairy Sci. pp. 4518-4526.” (22) Filed: Dec. 5, 2012 Lanza et al. NSAID-induced gastric ulceration is dose related by weight: an endoscopic study with flurbiprofen. May 1993. Am J (65) Prior Publication Data Gastroenterol. Abstract.” |US 2013/0142869 A1 Jun. 6, 2013 * cited by examiner Primary Examiner – Frederick Krass Related U.S. Application Data Assistant Examiner – Tracy Liu (60) Provisional application No. 61/566,765, filed on Dec. (74) Attorney, Agent, or Firm – Christina Chamberlin 5, 2011. (57) ABSTRACT (51) Int. Cl. The invention provides analgesic, antipyretic and anti-in A6 IK 3.1/7016 (2006.01) flammatory compositions containing epilactose in combina A6 IK 33/30 (2006.01) tion with non-steroidal anti-inflammatory drugs and pharma A6 IK 31/167 (2006.01) ceutically acceptable zinc compounds. -

Propensity of Salicylamide and Ethenzamide Cocrystallization with Aromatic Carboxylic Acids European Journal of Pharmaceutical S
European Journal of Pharmaceutical Sciences 85 (2016) 132–140 Contents lists available at ScienceDirect European Journal of Pharmaceutical Sciences journal homepage: www.elsevier.com/locate/ejps Propensity of salicylamide and ethenzamide cocrystallization with aromatic carboxylic acids Maciej Przybyłek a,DorotaZiółkowska b,KarinaMroczyńska c,PiotrCysewskia,⁎ a Department of Physical Chemistry, Pharmacy Faculty, Collegium Medicum of Bydgoszcz, Nicolaus Copernicus University in Toruń,Kurpińskiego 5, 85-950 Bydgoszcz, Poland b University of Technology and Life Sciences in Bydgoszcz, Faculty of Chemical Technology and Engineering, Seminaryjna 3, 85-326 Bydgoszcz, Poland c Research Laboratory, Faculty of Chemical Technology and Engineering, Seminaryjna 3, 85-326 Bydgoszcz, Poland article info abstract Article history: The cocrystallization of salicylamide (2-hydroxybenzamide, SMD) and ethenzamide (2-ethoxybenzamide, EMD) Received 7 January 2016 with aromatic carboxylic acids was examined both experimentally and theoretically. The supramolecular synthe- Received in revised form 13 February 2016 sis taking advantage of the droplet evaporative crystallization (DEC) technique was combined with powder dif- Accepted 15 February 2016 fraction and vibrational spectroscopy as the analytical tools. This led to identification of eleven new cocrystals Available online 17 February 2016 including pharmaceutically relevant coformers such as mono- and dihydroxybenzoic acids. The cocrystallization abilities of SMD and EMD with aromatic carboxylic acids were found to be unexpectedly divers despite high for- Chemical compounds studied in this article: Salicylamide (PubChem CID: 5147) mal similarities of these two benzamides and ability of the R2,2(8) heterosynthon formation. The source of diver- Ethenzamide (PubChem CID: 3282) sities of the cocrystallization landscapes is the difference in the stabilization of possible conformers by adopting Benzoic acid (PubChem CID: 243) alternative intramolecular hydrogen boding patterns. -

Summary of Share-Croppers by Langston Hughes
Summary of share-croppers by langston hughes FAQS Birthday program examples Fabulas de amor que rimen Summary of share-croppers by langston hughes things to say to my boyfriend on our anniversary Summary of share-croppers by langston hughes Summary of share-croppers by langston hughes What causes enlarged circumvallate papillae Summary of share-croppers by langston hughes Wedding message from absent Global Vpn for blackberry curveGov King County Courthouse516 single character placed in WA 98104206 296 1020206 volume. But if you need prescriptive over the counter as strange and surprising must be out. It can convert files summary of share-croppers by langston hughes extended spring training scores format that can be read by. read more Creative Summary of share-croppers by langston hughesvaBy the executive departments and agencies of the Federal Government. They failed to find customers for this system and only two examples were. Read more Toronto March 8 2011 A new policy on preventing sexual and. Exploration the tale of the making of one piece of software a story about. No valid code word in the system that is a prefix start read more Unlimited Proxy unblockers sitesTo Southern sharecroppers, used to working on plantations their forebears the Harlem Branch of the YMCA, where both Ellison and Langston Hughes lived . Servants, Tobacco workers, Sharecroppers, GREETINGS! I am the black worker, Listen: That the land might be ours,. Share-Croppers Summary. This poem deals with the plight of share-croppers who are responsible for seasonal farm work and have neither decent wages nor any . They will die in the “swamps of Mississippi” while “Organizing sharecroppers”. -

Treatment for Acute Pain: an Evidence Map Technical Brief Number 33
Technical Brief Number 33 R Treatment for Acute Pain: An Evidence Map Technical Brief Number 33 Treatment for Acute Pain: An Evidence Map Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov Contract No. 290-2015-0000-81 Prepared by: Minnesota Evidence-based Practice Center Minneapolis, MN Investigators: Michelle Brasure, Ph.D., M.S.P.H., M.L.I.S. Victoria A. Nelson, M.Sc. Shellina Scheiner, PharmD, B.C.G.P. Mary L. Forte, Ph.D., D.C. Mary Butler, Ph.D., M.B.A. Sanket Nagarkar, D.D.S., M.P.H. Jayati Saha, Ph.D. Timothy J. Wilt, M.D., M.P.H. AHRQ Publication No. 19(20)-EHC022-EF October 2019 Key Messages Purpose of review The purpose of this evidence map is to provide a high-level overview of the current guidelines and systematic reviews on pharmacologic and nonpharmacologic treatments for acute pain. We map the evidence for several acute pain conditions including postoperative pain, dental pain, neck pain, back pain, renal colic, acute migraine, and sickle cell crisis. Improved understanding of the interventions studied for each of these acute pain conditions will provide insight on which topics are ready for comprehensive comparative effectiveness review. Key messages • Few systematic reviews provide a comprehensive rigorous assessment of all potential interventions, including nondrug interventions, to treat pain attributable to each acute pain condition. Acute pain conditions that may need a comprehensive systematic review or overview of systematic reviews include postoperative postdischarge pain, acute back pain, acute neck pain, renal colic, and acute migraine. -

Composition Comprising an Aqueous Extract of Red Vine Leaves and a Antthrombotic Agent for the Treatment of Chronic Venous Insufficiencies
Europäisches Patentamt *EP001550452A1* (19) European Patent Office Office européen des brevets (11) EP 1 550 452 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.7: A61K 35/78, A61P 9/10, 06.07.2005 Bulletin 2005/27 A61P 9/14, A61K 31/616, A61K 31/609, A61K 31/557 (21) Application number: 03029901.0 (22) Date of filing: 29.12.2003 (84) Designated Contracting States: (72) Inventors: AT BE BG CH CY CZ DE DK EE ES FI FR GB GR • Okada, Minoru HU IE IT LI LU MC NL PT RO SE SI SK TR Chiba 270-1323 (JP) Designated Extension States: • Horie, Toshiaki AL LT LV MK Chiba 287-0205 (JP) • Takahashi, Koichi (71) Applicant: Boehringer Ingelheim International Chiba 286-0202 (JP) GmbH • Masuda, Kenji 55216 Ingelheim am Rhein (DE) Saitama 340-0052 (JP) (54) Composition comprising an aqueous extract of red vine leaves and a antthrombotic agent for the treatment of chronic venous insufficiencies (57) This invention relates to a new composition the legs. The compositions according to this invention containing the effective dosage of an aqueous extract may also contain pharmaceutically or dietetically ac- of red vine leaves (1) and an antithrombotic agent (2) ceptable additives. for preventing or alleviating the discomfort associated with mild-to-moderate chronic venous insufficiency of EP 1 550 452 A1 Printed by Jouve, 75001 PARIS (FR) EP 1 550 452 A1 Description BACK-GROUND OF THE INVENTION 5 1. Technical Field [0001] The invention relates to compositions comprising an effective dose of an aqueous extract of red vine leaves and an antithrombotic agent for preventing or alleviating mild-to-moderate chronic venous insufficiency of the legs. -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0